Abstract
Background
Specialist homelessness practices remain the main primary care access point for many persons experiencing homelessness. Prescribing practices are poorly understood in this population.
Objective
This study aims to investigate prescribing of medicines to homeless persons who present to specialist homelessness primary care practices and compares the data with the general population.
Setting
Analyses of publicly available prescribing and demographics data pertaining to primary care in England.
Methods
Prescribing data from 15 specialist homelessness practices in England were extracted for the period 04/2019-03/2020 and compared with data from (a) general populations, (b) the most deprived populations, and (c) the least deprived populations in England.
Main outcome measure
Prescribing rates, measured as the number of items/1000 population in key disease areas.
Results
Data corresponding to 20,572 homeless persons was included. Marked disparity were observed in regards to prescribing rates of drugs for Central Nervous System disorders. For example, prescribing rates were 83-fold (mean (SD) 1296.7(1447.6) vs. 15.7(9.2) p = 0.033) items), and 12-fold (p = 0.018) higher amongst homeless populations for opioid dependence and psychosis disorders respectively compared to the general populations. Differences with populations in the least deprived populations were even higher. Prescribing medicines for other long-term conditions other than mental health and substance misuse was lower in the homeless than in the general population.
Conclusions
Most of the prescribing activities in the homeless population relate to mental health conditions and substance misuse. It is possible that other long-term conditions that overlap with homelessness are under-diagnosed and under-managed. Wide variations in data across practices needs investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
-
The majority of prescribing activities focused on homeless populations relates to mental health conditions and substance misuse.
-
Our findings suggest potential under-diagnoses and under-treatment of other long-term health conditions such as cardiovascular and respiratory conditions in homeless populations.
-
Improving access to prevention and treatment of wider long term health conditions that overlap with homelessness and promoting medicines optimisation and adherence to prescribed treatments are key to improving the health of homeless populations.
Introduction
An estimated 280,000 people in England are known to be experiencing some form of homelessness [1]. Homelessness includes rooflessness (without a shelter of any kind, sleeping rough); houselessness (with a place to sleep but temporary in institutions or shelter); living in insecure housing (threatened with severe exclusion due to insecure tenancies, eviction, domestic violence); and living in inadequate housing (in caravans on illegal campsites, in unfit housing, in extreme overcrowding) [2]. In addition, in 2019 (i.e. prior to the COVID-19 pandemic), approximately 5,000 people slept rough on any given night in England [1]. During the first phase of the COVID-19 pandemic, an estimated 20,000 households became homeless in England [3]. However, those sleeping rough have been offered temporary accommodations such as emergency shelters and hotels during the pandemic. Findings from published literature suggest that persons experiencing homelessness (PEH) face extreme health inequalities [4] and 12 times higher mortality rates than the general population [5]. In England, males and females PEH are known to die at an average age of approximately 46 years and 43 years, respectively [6]. The majority of higher mortality is contributed by opioid overdose, accidents, heart failures and infectious diseases.
Historically, identifying healthcare and treatment needs amongst PEH has been difficult due to their secluded and unstable locations. Current epidemiological studies on the health status of PEH in the UK have tended to utilise local epidemiological datasets specific to a city, a region or a particular homelessness practice [4, 7]. The emergence of specialist primary care services has enabled accessibility of routine healthcare for PEH across the UK. At least one specialist homelessness general practice or healthcare centre currently operates in most UK cities, providing services exclusively for PEH [8]. Healthcare can also be accessed at general practices with homeless drop-in services, mobile homeless health teams, and volunteer organised healthcare days at local hostels and centres.
Currently, little is understood in regards to the prescribing of medicines to PEH in primary care. Analysis of prescribing data allows understanding of patient access to treatments and enables the development and strengthening of relevant primary care and public health prevention programmes to prevent ill health. One recently published study analysed prescribing medicines to PEH registered in mainstream general practices [9]. Medicines for mental health condition was identified to be the most frequently prescribed items. However, this study only included data of 43 patients registered with mainstream general practices. Two other studies [10, 11]) reported prescribing activities undertaken by pharmacist independent prescribers in specialist homeless health service and outreach settings. Medicines prescribed included treatments for depression, wounds, hypertension, pain and diabetes.
Aim of the study
This study aims to investigate prescribing medicines for persons who present to specialist general practices for PEH in England and compare the data with general populations.
Ethics approval
This study undertook an analysis of routinely collected deidentified and aggregated datasets that are publicly available. Therefore, formal ethical approval was not required.
Method
Prescribing datasets for 12 months between April 2019 and March 2020 relating to 20 British National Formulary (BNF) paragraphs were extracted from 15 specialist general practices for PEH in England through National Health Service (NHS) Digital Openprescribing dataset [12]. Literature mapping specialist primary care services for PEH in England were used to identify locations of specialist practices [8]. Data for specific practices were then searched one at a time in the national primary care prescribing dataset (Openprescribing). Datasets were extracted for each BNF paragraph relating to all general practices in England for comparison with the general populations. In addition, comparisons were made against prescribing datasets from all general practices in the top ten most deprived and ten least deprived Clinical Commissioning Groups (CCGs). The CCGs are clinically-led autonomous NHS bodies involved in providing services for their respective locality and constitute a cluster of general practices within a CCG [13]. The 20 CCGs at either end of deprivation were identified from the Ministry of Housing, Communities & Local Government 2019 summary statistics [14].
The selection of the 20 BNF chapters was based on the list of most commonly prescribed medicines in England in the general populations and epidemiological data related to disease prevalence and Quality and Outcomes Framework (QoF) disease areas [12, 15]. Descriptive analysis included mean and standard deviation of the number of medicinal items prescribed was extracted for mental health (hypnotics and anxiolytics, drugs used in psychoses and related disorders, antidepressant drugs, selective serotonin re-uptake inhibitors, Central Nervous System (CNS) stimulants and drugs used for ADHD, non-opioid analgesics and compound preparations, opioid analgesics, alcohol dependence, nicotine dependence and opioid dependence) and four other major BNF chapters (gastro-intestinal system, cardiovascular system, respiratory system and endocrine system). Populations and demographic data specific to each CCG were extracted from the Office of National Statistics and NHS digital databases [14, 16]. Data were extracted by one author (AK) and checked for accuracy by a second author (VP). Heterogeneity test for prescription items was carried out to compare the data across a) homelessness practices, c) general populations and c) practices in the most deprived and d) least deprived CCGs using a t-test for the continuous variables. All values are reported as the number of items prescribed per 1000 population. All analyses were carried out in Stata version 16, and figures were drawn using a Microsoft Excel sheet.
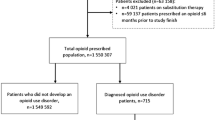
Results
The search identified 25 specialist general practices, of which seven practices were not accessible in the Openprescribing database, and three services had incomplete datasets and hence were excluded. A total of 15 specialist general practices were included (Table 1) [17,18,19,20,21,22,23,24,25,26] in this study, representing 20,572 PEH registrants. Nearly three-quarters of all registrants were males (n = 14,642, 73%).
Prescribing data.
Central Nervous system (CNS).
Specialist practices for PEH consistently showed higher rates of prescriptions for the ten CNS drug paragraphs extracted (Table 2). The least deprived regions showed the lowest volume of prescribing. The most commonly prescribed items in the PEH populations were antidepressant drugs, with 4594 items per 1000 population per year. The rate was 3-fold higher than the general populations (p = 0.019) and 3 times higher than the least deprived general populations in England (p = 0.003) (Table 2).
Data concerning drugs related to opioid dependence showed the highest difference in prescribing rates across the PEH and the general population. The rate in the PEH (x = 1296.7 items per 1000 population) was approximately 83-fold higher compared to the general populations (Table 2). Higher prescribing rates were observed for drugs for alcohol dependence (x = 50.2 vs. 2.6 per 1000 population, p = 0.161)) in PEH compared to the general population. Other BNF paragraphs which represented markedly higher prescribing rates in the PEH populations when compared to the general populations were related to drugs used in psychoses and related disorders (x = 2632.4 vs. 218.7 per 1000 population, p = 0.018), selective serotonin re-uptake inhibitors (x = 1633.9 vs. 738.5 per 1000 population, p = 0.040), and nicotine dependence (x = 114.5 vs. 13.0 per 1000 population, p = 0.051). While rates of prescribing opioid analgesics were approximately two-fold higher in the PEH population than the general population, prescribing non-opioid analgesics was similar across the two groups (Table 2).
Cardiovascular system.
Datasets were extracted for beta-blockers, calcium channel blockers (CCB), renin-angiotensin-aldosterone system (RAAS), antiplatelets and lipid-regulating drugs (Table 3, Electronic supplement 1). Fewer items were prescribed of RAAS drugs (x = 760.5 vs. 1186.3 per 1000 population, p = 0.005), antiplatelet drugs (x = 442.7 vs. 599.2 per 1000 population, p = 0.085), lipid-regulating drugs (x = 1043.9 vs. 1378.8 per 1000 population, p = 0.086) in PEH population compared to the general populations. The rates of prescribing these drugs in PEH populations were even lower when compared to the most deprived populations in England (Table 3, Electronic supplement 1).
Gastro-Intestinal system.
Prescribing data for proton pump inhibitors (PPIs) were extracted (Table 3, Electronic supplement 1). Significantly more items per 1000 population were prescribed to the PEH population than the general population (x = 1870.2 vs. 1145.5 per 1000 populations, p = 0.019).
Respiratory system.
Respiratory corticosteroids datasets were extracted (Fig. 1). Prescriptions in specialist practices for the homeless were approximately 20% higher than in mainstream practices (Table 3, Electronic supplement 1).
Endocrine system.
Datasets for antidiabetic drugs and thyroid hormones were extracted (Fig. 1). Fewer rates of antidiabetic medicines (x = 710.8 vs. 749.2 p = 0.826) and thyroid hormones (x = 191.3 vs. 602.2, p < 0.001) were prescribed in the PEH populations when compared to the general populations (Table 3, Electronic supplement 1).
Infections.
The prescribing frequency of anti-infectives was higher in the PEH population than mainstream general practices (x = 313.1 vs. 267.3 p = 0.319) and compared to the practices in the most and least deprived areas of England (Table 3, Electronic supplement 1).
Discussion
Statement of key findings
This study aimed to investigate trends of medicine prescribing to PEH populations in England. Datasets from 15 specialist general practices were retrieved and analysed, representing over 20,000 patients. Results demonstrate significantly higher prescribing rates for substance misuse and mental health conditions in the PEH than in the general population. However, fewer items aimed at other long-term health conditions, including cardiovascular and endocrine conditions, were prescribed to PEH compared to the general populations, suggesting that long-term conditions amongst PEH may be underdiagnosed and/or undertreated. Undiagnosed and under-treated long-term health conditions could explain the early and higher mortality rates observed in the PEH populations [6].
There were large variations in the rates of prescribing across the specialist homelessness general practices. Differences were most notably identified for mental health conditions, where some specialist general practices prescribed specific medicines categories approximately ten times more items than other specialist practices. Local commissioning arrangements in the services, discrepancies in local guidelines and formularies such as prescription thresholds and referral to mental health teams may have influenced such variations.
Strengths and weaknesses
The datasets represent a large sample of PEH from over 15 specialist general practices located in major urban areas across England, and the general population dataset provided a robust comparison. Given the large population size and completeness of Openprescribing dataset [12], any possibility of missing data is likely to be small and balanced across the comparison groups. Prescribing data in this study relied on registrants accessing healthcare exclusively from their specialist primary organisation. It is important to note that not all PEH have access to specialist homelessness health services, and some PEH may also be receiving services in mainstream general practices. However, previous studies have demonstrated PEH exclusion from mainstream services due to complexity in navigating services, inability to keep up appointments and perceived stigma and discrimination in practices by other patients and healthcare professionals [27,28,29]. These factors lead to PEH preferring to use specialist practices for their health services use. PEH are also frequent users of emergency departments and may often be excluded altogether from primary care [30]. Prescribing data was collected at a practice level, and therefore due to lack of access to patient-level data, it is important to undertake careful consideration. Large variations in prescribing rates were observed amongst specialist practices demonstrating the impact of local policies, practice level demographics, small sample size of the practices and unknown factors.
Interpretation
Epidemiological studies have demonstrated a high prevalence of mental health conditions and substance misuse problems [4, 7]. Causal and consequential relationships between mental health conditions, homelessness and substance misuse have been established [31, 32]. A recent systematic review showed that PEH are more likely to have a 3-fold higher risk of cardiovascular disease (OR 2.96) and 138% higher hypertension (OR 1.38) than general populations [33]. Literature suggests approximately 70% higher mortality rates in PEH due to all cardiovascular-related causes compared to the general population [34, 35]. Prescribing rates of cardiovascular drugs was observed to be lower in specialist homelessness practices in the current study compared to the general population suggesting potential under-diagnosis and under-treatment. Factors contributing to under-diagnoses and treatment can include prioritising treatment of substance misuse and mental health from patients and prescriber perspectives, asymptomatic nature of other long term health conditions, lack of holistic screening of health conditions and time constraints. In addition, long-term health and mortality compete with more immediate needs, such as obtaining adequate food and shelter. However, the literature suggests that PEH are willing to accept healthcare for chronic conditions if given the opportunity, and they believe such care to be important [36]. In relation to acute conditions, higher prescribing rates were observed with antibiotics demonstrating their vulnerability to injuries, infections and lack of opportunity to undertake self-care [37]. In addition, poor nutrition and stress increase the risk of exposure to a range of respiratory tract infections, viruses, and diseases.
Further research
Higher rates of prescribing of medicines for substance misuse and mental health demonstrate patient and/or prescriber priorities about their healthcare needs. Optimisation of prescribed medicines is important to ensure optimal outcomes from their treatment [38]. Introduction of prescribing pharmacists and nurses and outreach-based services conducted by the primary care team are likely to promote medicines optimisation and engagement with care [39, 40]. There is a need to develop and evaluate innovative service models to encourage access to services and treatments. Innovative service models are important also in the light of the recent COVID-19 pandemic, which has led to disruption in routine care provision [41,42,43] and is likely to widen inequality in access to service provisions. While our study demonstrated high prescribing rates in substance misuse and mental health, promoting adherence to prescribed medicines is key to optimal treatment outcomes. Patients with a dual diagnosis of mental health and substance misuse are most vulnerable to facing homelessness [44], and hence primary health and social care services should offer tailored services to prevent key causes and consequences of homelessness.
Many PEH are excluded from primary care due to various factors such as lack of ability to navigate services, perceived stigma and discrimination in healthcare settings and wrong application of registration criteria in mainstream practices [17]. It is imperative to capture the health status of those who do not have access to any primary care services. This study used aggregated dataset at practice level and future studies should consider exploring the extent of disparity using patient level data.
Conclusions
Currently, most of the prescribing activities in PEH relates to mental health conditions and substance misuse. It is possible that other long-term health conditions, such as diabetes and cardiovascular diseases, may be under-diagnosed and undermanaged. Primary healthcare professionals should offer targeted and opportunistic screening and treatment for other health conditions that overlap with poverty and deprivation. Optimisation of prescribed treatments and promoting adherence is key to achieving favourable health outcomes.
Data statement: Openprescribing datasets are developed and maintained by the University of Oxford EM DataLab [12]. It claims to cover anonymised data about the drugs prescribed by all general practices in England. However, it is likely that some general practices may be missing in the databases, particularly the specialist homelessness practices as reported in the results section of this paper. Data are shown per 1000 populations and are adjusted for England’s mid-year population size every year. The data are also normalised by drug name and classification and therefore, when drugs change their name or move across BNF chapters, it does not interfere with the analysis [45].
Availability of data and materials
All data generated or analysed during this study are included in this published article (and the supplemental materials).
References
Shelter England. 280,000 people in England are homeless, with thousands more at risk. https://england.shelter.org.uk/media/press_release/280,000_people_in_england_are_homeless,_with_thousands_more_at_risk. Accessed 25 July 2021.
ETHOS. European typology of homelessness ethos and housing exclusion. Available https://www.feantsa.org/download/ethos2484215748748239888.pdf. Accessed 25 July 2021.
Garcia Francisco. Homelessness in Britain is about to get much worse. http://www.theguardian.com/commentisfree/2020/aug/22/homelessness-britain-worse-pandemic. Accessed 25 July 2021.
Bowen M, Marwick S, Marshall T, et al. Multimorbidity and emergency department visits by a homeless population: a database study in specialist general practice. Br J Gen Pract. 2019; 69 (685): e515-e525. DOI: https://doi.org/10.3399/bjgp19X704609. Accessed 25 July 2021).
Aldridge RW, Story A, Hwang SW, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. The Lancet. 2017;391(10117):241–50.
Office for National Statistics. Deaths of homeless people in England and Wales: 2019 https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsofhomelesspeopleinenglandandwales/2019registrations. Accessed 25 July 2021.
Queen AB, Lowrie R, Richardson J, et al. Multimorbidity, disadvantage, and patient engagement within a specialist homeless health service in the UK: an in-depth study of general practice data. BJGP Open. 2017 Oct 1;1(3).
Crane M, Cetrano G, Joly L, et al. Mapping of specialist primary health care services in England for people who are homeless. (King’s College London, London) https://www.kcl.ac.uk/sspp/policy-institute/scwru/res/hrp/hrp-studies/HEARTH/HEARTH-study-Mapping-FullReport-2018.pdf. Accessed 25 July 2021.
Kaushal R, Jagpal P, Khanal S, et al. Representation of homeless persons and coding of homelessness in mainstream general practices: a descriptive evaluation using healthcare utilisation data. BJGP (Open).2021.0050. DOI: https://doi.org/10.3399/BJGPO.2021.0050.
Lowrie R, Williamson A, Spencer R, et al. Collaborative engagement for long term conditions by clinical pharmacists for people who are homeless in Glasgow, Scotland. http://www.feantsa.org/download/march-2017-health-and-homelessness-newsletter2959399951318964653.pdf. Accessed 04/02/21.
Lowrie F, Gibson L, Lowrie R, et al. A descriptive study of a novel pharmacist led health outreach service for those experiencing homelessness. Int J Pharm Pract. 2019;27(4):355–61.
OpenPrescribing.net. EBM. DataLab. University of Oxford. https://openprescribing.net/. Accessed 25 July 2021.
Ministry of Housing. Communities & Local Government. File 13: clinical commissioning group summaries. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019. Accessed 25 July 2021.
Office for National Statistics. Clinical commissioning group population estimates (National Statistics). https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/clinicalcommissioninggroupmidyearpopulationestimates. Accessed 25 July 2021.
NHS Digital. Quality and Outcomes Framework. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/general-practice-data-hub/quality-outcomes-framework-qof. Accessed 21 July 2021.
NHS Digital. Patients Registered at a GP Practice October. 2020. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice/october-2020. Accessed 25 July 2021.
Homeless Link. (2014) Search homelessness services in England. (Homeless Link. London) https://www.homeless.org.uk/search-homelessness-services. Accessed 25 July 2021.
Inclusion healthcare. Homeless GP service. https://inclusionhealthcare.co.uk/our-work/homeless-gp-service/. Accessed 25 July 2021.
Southampton Directory. Homeless Health Care Team. https://sid.southampton.gov.uk/kb5/southampton/directory/service.page?id=BbhUjt3eysg&newadultchannel=1. Accessed 25 July 2021.
Oxford Health NHS Foundation Trust. Luther Street Medical Centre. https://www.oxfordhealth.nhs.uk/service_description/luther-street-medical-centre/. Accessed 25 July 2021.
Northgate Medical Centre. St Werburgh’s Practice for the Homeless. https://www.northgatemedicalcentre.nhs.uk/st-werburghs-practice-for-the-homeless/. Accessed 25 July 2021.
Devon Doctors. Clock Tower Surgery takes residence in exciting new wellbeing hub. https://www.devondoctors.co.uk/news/clock-tower-surgery-takes-residence-exciting-new-wellbeing-hub. Accessed 25 July 2021.
North Central London Clinical Commissioning Group. CHIP – Camden Health Improvement Practice. https://gps.northcentrallondonccg.nhs.uk/service/chip-camden-health-improvement-practice. Accessed 25 July 2021.
East London NHS Foundation Trust. Newham Transitional Practice - Main Site. https://elft.nhs.uk/service/200/Newham-Transitional-Practice---Main-Site. Accessed 25 July 2021.
Health E1 Homeless Medical Centre. Health E1 Homeless Medical Centre. http://www.healthe1practice.nhs.uk/#. Accessed 25 July 2021.
Great Chapel Street Medical Centre. Great Chapel Street Medical Centre. https://greatchapelst.org.uk/#. Accessed 25 July 2021.
Gunner E, Chandan SK, Marwick S, Saunders K, Burwood S, Yahyouche A, Paudyal V. Perspectives of homeless individuals on the provision and accessibility of primary healthcare services: A qualitative study. Br J Gen Pract. 2019;69:e526–36.
Paudyal V, MacLure K, Buchanan C, et al. When you are homeless, you are not thinking about your medication, but your food, shelter or heat for the night’: behavioural determinants of the homeless population adherence to prescribed medicines. Public Health. 2017;148:1–8.
Gibson Smith K, Paudyal V, MacLure K, et al. Relocating patients from a specialist homeless healthcare centre to general practices: a multi-perspective study. Br J Gen Pract 2018 68(667):e105-e113.
Paudyal V, Ghani A, Shafi T, et al. Clinical characteristics, attendance outcomes and deaths of homeless persons in the emergency department: implications for primary healthcare and community prevention programmes. Public Health. 2021. 196:117–23.
Johnson G, Chamberlain C. Homelessness and substance abuse: which comes first? Australian Social Work. 2008;61(4):342–56.
Homeless Link. The unhealthy state of homelessness. Health audit results 2014 (Homeless Link, London) https://www.homeless.org.uk/sites/default/files/site-attachments/The%20unhealthy%20state%20of%20homelessness%20FINAL.pdf. Accessed 25 July 2021.
Al-Shakarchi N, Evans H, Luchenski S, et al. Cardiovascular disease in the homeless: a systematic review of observational and interventional studies. The Lancet. 2019;394:16.
Hwang SW, Wilkins R, Tjepkema M, et al. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ 2009; 27;339:b4036.
Baggett TP, Liauw SS, Hwang SW. Cardiovascular disease and homelessness. J Am College Cardiol. 2018;5(22):2585–97. 71(.
Kushel M, Vittinghoff E, Haas J. Factors Associated With the Health Care Utilization of Homeless Persons. JAMA. 2001; 285(2):200-206.
Paudyal V, Maclure K, Forbes-McKay K, et al. If I die, I die, I don’t care about my health’: perspectives on self-care of people experiencing homelessness. Health Soc Care Community. 2020;28:160–72.
Alenezi A, Yahyouche A, Paudyal V. Current status of opioid epidemic in the United Kingdom and strategies for treatment optimisation in chronic pain chronic non-malignant pain: A systematic review. Int J Clin Pharm. 2021;43(2):318–22. https://doi.org/10.1007/s11096-020-01205-y.
Lowrie R, Stock K, Lucey S, et al. Pharmacist led Homeless Outreach Engagement and Non-Medical Independent 1 prescribing (Rx) (PHOENIx) intervention for people experiencing homelessness: a non- 2 randomised feasibility study. Int J Equity Health. 2021; 20:19. https://doi.org/10.1186/s12939-020-01337-7.
Jagpal P, Barnes N, Lowrie R, et al. Clinical pharmacy intervention for persons experiencing homelessness: evaluation of patient perspectives in service design and development. Pharmacy; 2019:7:153. doi:https://doi.org/10.3390/pharmacy7040153.
Dhada S, Stewart D, Cheema E, et al. Cancer Services During the COVID-19 Pandemic: Systematic Review of Patient’s and Caregiver’s Experiences. Cancer Manage Res. 2021;13:5875–87. https://doi.org/10.2147/CMAR.S318115.
Paudyal V, Cadogan C, Fialova D, et al. Provision of clinical pharmacy services during the COVID-19 pandemic: experiences of pharmacists from 16 European countries. Res Social Administrative Pharm. 2021;17(8):1507–17.
Kaur S, Jagpal P, Paudyal V. Provision of services to persons experiencing homelessness during the COVID-19 pandemic: a qualitative study on the perspectives of homelessness service providers. Health and Social Care in the Community. 2021. doi: https://doi.org/10.1111/hsc.13609.
Alsuhaibani R, Smith DC, Lowrie R, et al. Scope, quality and inclusivity of international clinical guidelines on mental health and substance misuse in relation to dual diagnosis, social and community outcomes: a systematic review. BMC Psychiatry 2021; 21, 209; 2021. https://doi.org/10.1186/s12888-021-03188-0.
NHS Digital. Practice level prescribing. Available: https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/general-practice-data-hub/practice-level-prescribing. Accessed 03 Feb 2022.
Acknowledgements
None.
Funding
This study received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khan, A., Kurmi, O., Lowrie, R. et al. Medicines prescribing for homeless persons: analysis of prescription data from specialist homelessness general practices. Int J Clin Pharm 44, 717–724 (2022). https://doi.org/10.1007/s11096-022-01399-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-022-01399-3