Abstract
Rationale
Although driving simulators (DS) are receiving increasing attention due to concern over traffic accidents under the influences of drugs, few DS are recognized for their reliability and validity. Therefore, the development of an evaluation system using DS for driving performance is urgently needed.
Objectives
To investigate whether the standard deviation of lateral position (SDLP) increases with blood alcohol concentration (BAC) using a DS with reliability and calculate the SDLP threshold from the difference between BAC levels of 0 and 0.05%.
Methods
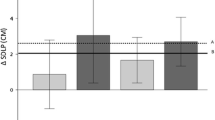
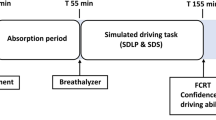
Twenty healthy Japanese men performed the DS tasks up to 60 min in Study 1 and DS tasks twice at 1-week intervals in Study 2. Twenty-six healthy men conducted the same DS tasks under BAC level (0, 0.025, 0.05, and 0.09%) in double-blind, randomized, crossover trial in Study 3. The primary outcome was SDLP in a road-tracking test. The test–retest reliability of DS data was assessed, and the estimated difference in SDLP between BAC levels of 0 and 0.05% was calculated using a linear regression model.
Results
The cumulative SDLP values at 5-min intervals were stable, and the intraclass correlation coefficient for its values was 0.93. SDLP increased with BAC in a concentration-dependent manner. The predicted ΔSDLP value for the difference between BAC levels of 0 and 0.05% was 9.23 cm. No participants dropped out because of simulator sickness.
Conclusions
The new DS used in these studies has reliability, validity, and tolerability and is considered suitable for evaluating the influence of drugs on driving performance.



Similar content being viewed by others
References
Akerstedt T, Gillberg M (1990) Subjective and objective sleepiness in the active individual. Int J Neurosci 52:29–37
Arnedt JT, Wilde GJ, Munt PW, MacLean AW (2000) Simulated driving performance following prolonged wakefulness and alcohol consumption: separate and combined contributions to impairment. J Sleep Res 9:233–241
Bioulac S, Micoulaud-Franchi JA, Arnaud M, Sagaspe P, Moore N, Salvo F, Philip P (2017) Risk of motor vehicle accidents related to sleepiness at the wheel: a systematic review and meta-analysis. Sleep 40:zsx134
Borkenstein RF, Crowther R, Shumate R (1974) The role of the drinking driver in traffic accidents (the Grand Rapids study). Blutalkohol 11:1–131
Brookhuis K, de Waard D, Mulder B (1994) Measuring driving performance by car-following in traffic. Ergonomics 37:427–434
Brooks JO, Goodenough RR, Crisler MC, Klein ND, Alley RL, Koon BL, Logan WC Jr, Ogle JH, Tyrrell RA, Wills RF (2010) Simulator sickness during driving simulation studies. Accid Anal Prev 42:788–796
Chen S, Kuhn M, Prettner K, Bloom DE (2019) The global macroeconomic burden of road injuries: estimates and projections for 166 countries. Lancet Planet Health 3:e390–e398
Drake C, Gumenyuk V, Roth T, Howard R (2014) Effects of armodafinil on simulated driving and alertness in shift work disorder. Sleep 37:1987–1994
Fleiss JL (1986) The design and analysis of clinical experiments. John Wiley & Sons Inc., New York
Governors Highway Safety Association (2018) Drug-impaired driving: marijuana and opioids raise critical issues for states. Governors Highway Safety Association, Washington D.C
Hampson E (1990) Variations in sex-related cognitive abilities across the menstrual cycle. Brain Cogn 14:26–43
Harada S (1995) Disperal of the ALDH2 mutant in Mongoroid population. In: Akazawa T (ed) Prehistoric dispersal of Mongoroid. Oxford University Press, London, pp 165–171
Harada S (1991) Genetic polymorphism of alcohol metabolizing enzumes and its implication to human ecology. J Anthrop Soc Nippon 99:123–139
Helland A, Jenssen GD, Lervag LE, Westin AA, Moen T, Sakshaug K, Lydersen S, Morland J, Slordal L (2013) Comparison of driving simulator performance with real driving after alcohol intake: a randomised, single blind, placebo-controlled, cross-over trial. Accid Anal Prev 53:9–16
Hindmarch I, Trick L, Ridout F (2005) A double-blind, placebo- and positive-internal-controlled (alprazolam) investigation of the cognitive and psychomotor profile of pregabalin in healthy volunteers. Psychopharmacology 183:133–143
Horne JA, Reyner LA, Barrett PR (2003) Driving impairment due to sleepiness is exacerbated by low alcohol intake. Occup Environ Med 60:689–692
Huizinga CR, Zuiker RG, de Kam ML, Ziagkos D, Kuipers J, Mejia Y, van Gerven JM, Cohen AF (2019) Evaluation of simulated driving in comparison to laboratory-based tests to assess the pharmacodynamics of alprazolam and alcohol. J Psychopharmacol 33:791–800
Iwamoto K, Takahashi M, Nakamura Y, Kawamura Y, Ishihara R, Uchiyama Y, Ebe K, Noda A, Noda Y, Yoshida K, Iidaka T, Ozaki N (2008) The effects of acute treatment with paroxetine, amitriptyline, and placebo on driving performance and cognitive function in healthy Japanese subjects: a double-blind crossover trial. Hum Psychopharmacol 23:399–407
Iwata M, Iwamoto K, Kambe D, Tachibana N, Ando M, Ozaki N (2020) Development and validation of a driving simulator for evaluating the residual effects of drugs on driving performance - sensitivity analysis using zopiclone as a positive control: study protocol clinical trial (SPIRIT compliant). Medicine (Baltimore) 99:e19395
Iwata M, Iwamoto K, Kawano N, Kawaue T, Ozaki N (2018) Evaluation method regarding the effect of psychotropic drugs on driving performance: a literature review. Psychiatry Clin Neurosci 72:747–773
Iwata M, Iwamoto K, Omura T, Ando M, Ozaki N (2019) Protocol for the development and validation of a driving simulator for evaluating the influence of drugs on driving performance. Medicine (Baltimore) 98:e14613
Jones AW (2011) Pharmacokinetics of ethanol - issues of forensic importance. Forensic Sci Rev 23:91–136
Jongen S, Vermeeren A, van der Sluiszen NN, Schumacher MB, Theunissen EL, Kuypers KP, Vuurman EF, Ramaekers JG (2017) A pooled analysis of on-the-road highway driving studies in actual traffic measuring standard deviation of lateral position (i.e., "weaving") while driving at a blood alcohol concentration of 0.5 g/L. Psychopharmacology 234:837–844
Jongen S, Vuurman EF, Ramaekers JG, Vermeeren A (2016) The sensitivity of laboratory tests assessing driving related skills to dose-related impairment of alcohol: a literature review. Accid Anal Prev 89:31–48
Kay G, Ahmad O, Brown T, Veit A (2013) Comparison of the Minisim and Stisim driving simulators for the detection of impairment: an alcohol validation study, pp 191–197
Kay G, Hochadel T, Sicard E, Natarajan KK, Kim NN (2017) Next-day residual effects of flibanserin on simulated driving performance in premenopausal women. Hum Psychopharmacol 32:e2603
Kay G, Logan BK (2011) In: Transport Do (ed) Drugged driving expert panel report: a consensus protocol for assessing the potential of drugs to impair driving. National Higway Traffic Safety Administration, Washington, DC
Kenntner-Mabiala R, Kaussner Y, Jagiellowicz-Kaufmann M, Hoffmann S, Kruger HP (2015) Driving performance under alcohol in simulated representative driving tasks: an alcohol calibration study for impairments related to medicinal drugs. J Clin Psychopharmacol 35:134–142
Kuypers KP, Samyn N, Ramaekers JG (2006) MDMA and alcohol effects, combined and alone, on objective and subjective measures of actual driving performance and psychomotor function. Psychopharmacology 187:467–475
Lee J, Fiorentino D, Reyes ML, Brown TL, Ahmad O, Fell J, Ward N, Dufour R (2010) Assessing the feasibility of vehicle-based sensors to detect alcohol impairment. Administration NHTS, Washington, DC
Leufkens TR, Ramaekers JG, de Weerd AW, Riedel WJ, Vermeeren A (2014) Residual effects of zopiclone 7.5 mg on highway driving performance in insomnia patients and healthy controls: a placebo controlled crossover study. Psychopharmacology 231:2785–2798
Louwerens JW, Gloerich ABM, de Vries G, Brookhuis KA, O’Hanlon JF (1987) The relationship between drivers, blood alcohol concentration (BAC) and actual driving performance during high speed travel. In: Noordzij PC, Roszbach R (eds) Alcohol Drugs Traffic Safety, vol T86, pp 183–192
McNair DM, Lorr M, Droppeleman LF (1971) Manual for profile of mood states. Education and Industrial Testing Service, San Diego
Mets MA, Kuipers E, de Senerpont Domis LM, Leenders M, Olivier B, Verster JC (2011) Effects of alcohol on highway driving in the STISIM driving simulator. Hum Psychopharmacol 26:434–439
Mizoi Y, Kogame M, Fukunaga T, Ueno Y, Adachi J, Fujiwara S (1985) Polymorphism of aldehyde dehydrogenase and ethanol elimination. Alcohol 2:393–396
Mumenthaler MS, Taylor JL, O'Hara R, Yesavage JA (1999) Gender differences in moderate drinking effects. Alcohol Res Health 23:55–64
National Highway Traffic Safety Administration (2019) Traffic safety facts 2017. National Highway Traffic Safety Administration, Washington, DC
National Police Agency (2018) Statistics about road traffic annual report 2018. National Public Safety Commision and National Police Agency, Tokyo
O'Hanlon JF (1984) Driving performance under the influence of drugs: rationale for, and application of, a new test. Br J Clin Pharmacol 18(Suppl 1):121S–129S
O'Hanlon JF, Vermeeren A, Uiterwijk MM, van Veggel LM, Swijgman HF (1995) Anxiolytics’ effects on the actual driving performance of patients and healthy volunteers in a standardized test. An integration of three studies. Neuropsychobiology 31:81–88
Organisation for Economic Co-operation and Development (2020) Road fatalities by age - extract from the IRTAD database. International Transport Forum
Phillips SM, Sherwin BB (1992) Variations in memory function and sex steroid hormones across the menstrual cycle. Psychoneuroendocrinology 17:497–506
Ramaekers JG, Lamers J, Verhey F, Muntjewerff D, Mobbs E, Sanders N, Lewis M, Lockton A (2002) A comparative study of the effects of carbamazepine and the NMDA receptor antagonist remacemide on road tracking and car-following performance in actual traffic. Psychopharmacology 159:203–210
Ramaekers JG, Robbe HW, O'Hanlon JF (2000) Marijuana, alcohol and actual driving performance. Hum Psychopharmacol 15:551–558
Ravera S, Monteiro SP, de Gier JJ, van der Linden T, Gomez-Talegon T, Alvarez FJ, Partners DPW (2012) A European approach to categorizing medicines for fitness to drive: outcomes of the DRUID project. Br J Clin Pharmacol 74:920–931
Ridout F, Hindmarch I (2001) Effects of tianeptine and mianserin on car driving skills. Psychopharmacology 154:356–361
Simen AA, Gargano C, Cha JH, Drexel M, Bautmans A, Heirman I, Laethem T, Hochadel T, Gheyle L, Bleys K, Beals C, Stoch A, Kay GG, Struyk A (2015) A randomized, crossover, placebo-controlled clinical trial to assess the sensitivity of the CRCDS mini-Sim to the next-day residual effects of zopiclone. Ther Adv Drug Saf 6:86–97
Takahashi M, Iwamoto K, Kawamura Y, Nakamura Y, Ishihara R, Uchiyama Y, Ebe K, Noda A, Noda Y, Yoshida K, Iidaka T, Ozaki N (2010) The effects of acute treatment with tandospirone, diazepam, and placebo on driving performance and cognitive function in healthy volunteers. Hum Psychopharmacol 25:260–267
US Food and Drug Administration (2013) FDA drug safety communication: risk of next-morning impairment after use of insomnia drugs; FDA requires lower recommended doses for certain drugs containing zolpidem (Ambien, Ambien CR, Edluar, and Zolpimist)
US Food and Drug Administration (2017) Evaluating drug effects on the ability to operate a motor vehicle guidance for industry, Silver Spring, MD
Vermeeren A, Riedel WJ, van Boxtel MP, Darwish M, Paty I, Patat A (2002) Differential residual effects of zaleplon and zopiclone on actual driving: a comparison with a low dose of alcohol. Sleep 25:224–231
Vermeeren A, Sun H, Vuurman EF, Jongen S, Van Leeuwen CJ, Van Oers AC, Palcza J, Li X, Laethem T, Heirman I, Bautmans A, Troyer MD, Wrishko R, McCrea J (2015) On-the-road driving performance the morning after bedtime use of Suvorexant 20 and 40 mg: a study in non-elderly healthy volunteers. Sleep 38:1803–1813
Verster JC, Roth T (2011) Standard operation procedures for conducting the on-the-road driving test, and measurement of the standard deviation of lateral position (SDLP). Int J Gen Med 4:359–371
Verster JC, Roth T (2014) Effects of central nervous system drugs on driving: speed variability versus standard deviation of lateral position as outcome measure of the on-the-road driving test. Hum Psychopharmacol 29:19–24
Walsh JM, Verstraete AG, Huestis MA, Morland J (2008) Guidelines for research on drugged driving. Addiction 103:1258–1268
Wingen M, Bothmer J, Langer S, Ramaekers JG (2005) Actual driving performance and psychomotor function in healthy subjects after acute and subchronic treatment with escitalopram, mirtazapine, and placebo: a crossover trial. J Clin Psychiatry 66:436–443
World Health Organization (2016) Drug use and road safety : a policy brief. Switzerland, Geneva
Acknowledgments
This trial was supported by Taisho Pharmaceutical Company, Ltd.; Research on Regulatory Science of Pharmaceuticals and Medical Devices from the Japan Agency for Medical Research and Development (JP20mk0101137h0002); research grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Ministry of Health, Labour and Welfare of Japan; and a Grant-in-Aid from the “Center of Innovation for Personalized and Diverse Society” carried out under the Center of Innovation Program from the Japan Science and Technology Agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MI has no conflicts of interest to declare. KI has received speakers’ honoraria from or has served as a consultant to Dainippon Sumitomo, Janssen, Meiji Seika Pharma, Mochida, Otsuka, Taisho, Towa, and Pfizer. IK, TN, KO, YK and IN are employees of Taisho Pharmaceutical Co., Ltd., Japan. MA has received subsidies from Kyowa Kirin. NO has received research support or speakers’ honoraria from or has served as a consultant to Abbvie, Asahi Kasei Pharma, Astellas, Dainippon Sumitomo, Eisai, Eli Lilly, GlaxoSmithKline, Janssen, Meiji Seika Pharma, Mochida, MSD, Novartis Pharma, Ono, Otsuka, Pfizer, Shionogi, Takeda, Tanabe Mitsubishi, Sanofi, and Yoshitomi.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kunihiro Iwamoto Joint first authorship
Rights and permissions
About this article
Cite this article
Iwata, M., Iwamoto, K., Kitajima, I. et al. Validity and reliability of a driving simulator for evaluating the influence of medicinal drugs on driving performance. Psychopharmacology 238, 775–786 (2021). https://doi.org/10.1007/s00213-020-05730-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-020-05730-6