Abstract
Summary
Robust data on osteoporosis in the Asia Pacific region could improve healthcare decision-making. Osteoporosis affects 10–30% of women aged 40 + , and up to 10% of men in 7 developed economies in Asia Pacific. Fractures affect 500–1000 adults aged 50 + per 100,000 person-years. Policymakers and clinicians must address this problem.
Purpose
Osteoporosis and associated fractures result in considerable morbidity, loss of productivity, early mortality, and increased healthcare expenses. Many countries in the Asia Pacific (AP) region, especially middle- and higher-income economies, are faced with aging and increasingly sedentary populations. It is critical to consolidate and analyze the available information on the prevalence and incidence of the disease in these countries.
Methods
We systematically reviewed articles and gray literature for Australia, China, Hong Kong, Japan, Singapore, South Korea, and Taiwan. We searched PubMed, ScienceDirect, JSTOR, Cochrane, Google Scholar, and other databases for data published 2009–2018. We included articles with prevalence or incidence estimates for adults with osteoporosis or related fractures.
Results
All locations had data available, but of widely varying quantity and quality. Most estimates for osteoporosis prevalence ranged from 10 to 30% for women ages 40 and older, and up to 10% for men. Osteoporotic fracture incidence typically ranged between 500 and 1000 per 100,000 person-years among adults aged 50 and older. Both outcomes typically increased with age and were more common among women.
Conclusion
Osteoporosis and associated fractures affect significant portions of the adult population in developed economies in the AP region. Governments and healthcare systems must consider how best to prevent and diagnose osteoporosis, and manage affected individuals, to reduce healthcare costs and mortality associated with fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis and associated fractures cause significant morbidity and mortality and represent a major source of non-communicable disease burden and healthcare resource utilization around the world.
The Asia Pacific (AP) region is comprised of South Asia, South-East Asia, East Asia, and Oceania. An audit conducted in 2013 by the International Osteoporosis Foundation (IOF) encompassing 16 countries revealed a dearth of epidemiological information on osteoporosis and related fractures in the AP region [1]. In addition, only about one-fourth of the countries in the audit considered osteoporosis a national health priority, despite the burden of the disease and related fractures placed on healthcare institutions, reimbursement services, and patients. The number of people affected by osteoporosis and related fractures in this region is expected to rise significantly in the coming decades, largely due to the region’s aging population, increasing urbanization, and its associated sedentary lifestyles. By 2050, more than 50% of the world’s osteoporotic fractures are expected to occur in Asia, which will strain healthcare and government resources, especially considering the significant shortcomings in the quality and availability of health services for osteoporosis and related fractures currently present in many AP nations [1].
Since many individuals with poor bone health are still of working age and actively contributing to these countries’ economies, lost productivity and increased healthcare expenditures caused by preventable disease, fractures, and even deaths may become a heavy economic and societal burden. About one in four individuals suffering a hip fracture dies within a year, and other fragility fractures are also associated with premature mortality. Osteoporosis is more common in women, but its impact on health and survival is more marked in men than in women [2, 3].
Professional and health service organizations in the region are increasingly taking note of the importance of addressing osteoporosis and related fractures on a large scale. Organizations such as the Asia Pacific Consortium on Osteoporosis (APCO) and the IOF are working to highlight the economic, social, and health impact of osteoporosis and related fractures in the AP region. The knowledge and support of these organizations are available to provide governments the information and guidance they may need to craft action plans, data acquisition efforts, healthcare reimbursement policies, and more.
Though the governments of some of the more developed economies in the region have begun to recognize osteoporosis as a healthcare priority, a lack of in-depth understanding of the impact that osteoporosis and related fractures have on populations, healthcare systems, and the economy still exists. It is therefore crucial to gather data on the epidemiology of the disease in these locations to mitigate this gap in knowledge.
The objective of this systematic literature review was to obtain location-specific, epidemiological estimates of the prevalence and incidence of osteoporosis and related fractures in seven upper-middle- and high-income economies in the AP region: Australia, China, Hong Kong, Japan, Singapore, South Korea, and Taiwan. Estimates from any age, sex, or ethnicity group were of interest, provided the studies included at least one study arm considered reasonably representative of the broader population from which they were selected. The findings can be used by the governments of these countries and regions to inform policies or strategies for addressing poor bone health and its related societal burden.
Methods
This study was conducted according to the Cochrane review methodology for systematic literature reviews (version 5.1.0) [4] with some adaptations to allow for the emphasis on observational/epidemiological studies and the inclusion of non-academic gray literature, foreign-language database searches, secondary data, and general Internet searches. The PRISMA Checklist for systematic reviews guided protocol creation [5].
Study eligibility
Studies were included based on predetermined criteria using the PICOS design (see Table 1), in order to obtain estimates that may reasonably reflect the prevalence or incidence of osteoporosis and related fractures from the broader populations from which the study participants were drawn.
Search terms and database selection
Data sources selected included PubMed, ScienceDirect, the Cochrane Database of Systematic Reviews, JSTOR, and Google Scholar. To capture data and reports of osteoporosis and fractures from public health agencies or organizations that may have published on prevalence and incidence outside of formal academic literature, such as in government reports, we also conducted a review of gray literature via country-specific Google search pages and special-interest websites from a preselected list of regional health organizations, journals, and advocacy groups.
The guiding Boolean search string for each database, customized according to the country/location and as needed for database search limitations, was as follows:
(osteoporo* OR bone density OR bone loss OR fragility OR low-trauma) AND (inciden* OR prevalen* OR fracture* OR annual OR rate OR epidemiol*) AND COUNTRY
Study selection and data abstraction
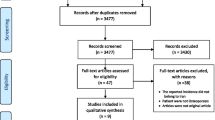
Studies were reviewed and selected in two phases (see Fig. 1).
Study selection flowchart. *Due to volume of results and budget limitations, the results were restricted to 2009 onward (2016 onward for posters) for full-text review. †Because this review was part of a broader study of 27 locations in the AP region, some articles were initially obtained and filed in folders for other locations; full-text review revealed 37 articles originally connected with other locations that included data relevant to the seven locations of interest for this manuscript
In phase one, two reviewers separately reviewed titles/abstracts divided by locations and applied inclusion/exclusion criteria. If a reviewer was uncertain, the two reviewers consulted each other and, if needed, discussed the article with the lead data reviewer (author KB) for a final decision on inclusion. In phase two, two reviewers independently reviewed all full-text articles, compared their decisions to align on any articles with mismatched selection status, and consulted the lead reviewer as needed for questions or final decisions. Translations were not obtained for the small number of non-English resources.
One reviewer extracted all data from the papers selected for inclusion and subsequently scored each included article for quality according to the criteria in the National Heart Lung and Blood Institute’s (NHLBI) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [6]. NHLBI quality scores were recorded for each article and considered in interpretation of the findings. Quality assessment checks of the data and study quality categorizations were made by the lead data reviewer (author KB) at least once at each step.
Data sought included location/country, sex, age, and other pertinent population details; year(s) in which the research was conducted; densitometry technology used for diagnosis of osteoporosis, criteria, and anatomical location of screening (heel, spine, hip, etc.); study type (longitudinal, review, cross-sectional, etc.); and estimates provided for prevalence of osteoporosis or incidence of related fracture, by body site. Summary tables were developed to provide location-specific ranges of osteoporosis prevalence and hip and vertebral fracture incidence by age group and sex.
Results
Full-paper distribution by country
All seven locations had results for both osteoporosis and related fractures. The final full-text article count was 316; some papers covered more than one place or provided data for both disease prevalence and fracture incidence. Table 2 shows the final distribution of articles covering each type of data for each location.
Figures 2,3, 4, 5, 6, 7, and 8 display graphical summaries of osteoporosis prevalence and fracture incidence in each location. Study characteristics, quality assessments, and summary results for studies reporting osteoporosis prevalence can be found together in location-specific tables (Tables 3, 4,5, 6,7,8, and 9, Appendix). Tables 10, 11, 12, 13, 14, 15, and 16 in the Appendix provide location-specific study characteristics, quality assessments, and reported results for studies reporting osteoporotic fracture incidence. The complete citation list for the 316 articles that underwent data extraction can be found in the Appendix.
a Australia osteoporosis prevalence. b Australia fracture incidence per 100,000 person-years. Connected lines represent “estimated” data reflecting findings for broad age ranges (e.g. 60–75, 50 +); these data were noted as linked data points for all age categories included in the reported range. Each color represents a single study. “All adults” represents generalized data describing broad populations without specified age groups (e.g. “Five percent of Australian men have osteoporosis”). Full citations for articles not cited in-text can be found in the Appendix. Circle = female; square = male; triangle = total/not available. F, femoral neck/hip; V, vertebrae/spine; W, wrist/forearm; H, humerus; M, multiple; O, other; N, not specified/general fragility fractures
a China osteoporosis prevalence. b China fracture incidence. Connected lines represent “estimated” data reflecting findings for broad age ranges (e.g. 60–75, 50 +); these data were noted as linked data points for all age categories included in the reported range. Each color represents a single study. “All adults” represents generalized data describing broad populations without specified age groups (e.g. “Five percent of Australian men have osteoporosis”). Full citations for studies not cited in-text can be found in the Appendix. Circle = female; square = male; triangle = total/not available. F, femoral neck/hip; V, vertebrae/spine; W, wrist/forearm; H, humerus; M, multiple; O, other; N, not specified/general fragility fractures
a Hong Kong osteoporosis prevalence. b Hong Kong fracture incidence. Connected lines represent “estimated” data reflecting findings for broad age ranges (e.g. 60–75, 50 +); these data were noted as linked data points for all age categories included in the reported range. Each color represents a single study. “All adults” represents generalized data describing broad populations without specified age groups (e.g. “Five percent of Australian men have osteoporosis”). Full citations for studies not cited in-text can be found in the Appendix. Circle = female; square = male; triangle = total/not available. F, femoral neck/hip; V, vertebrae/spine; W, wrist/forearm; H, humerus; M, multiple; O, other; N, not specified/general fragility fractures
a Japan osteoporosis prevalence. b Japan fracture incidence. Connected lines represent “estimated” data reflecting findings for broad age ranges (e.g. 60–75, 50 +); these data were noted as linked data points for all age categories included in the reported range. Each color represents a single study. “All adults” represents generalized data describing broad populations without specified age groups (e.g. “Five percent of Australian men have osteoporosis”). Full citations for studies not cited in-text can be found in the Appendix. Circle = female; square = male; triangle = total/not available. F, femoral neck/hip; V, vertebrae/spine; W, wrist/forearm; H, humerus; M, multiple; O, other; N, not specified/general fragility fractures
a Singapore osteoporosis prevalence. b Singapore fracture incidence. Connected lines represent “estimated” data reflecting findings for broad age ranges (e.g. 60–75, 50 +); these data were noted as linked data points for all age categories included in the reported range. Each color represents a single study. “All adults” represents generalized data describing broad populations without specified age groups (e.g. “Five percent of Australian men have osteoporosis”). Full citations for studies not cited in-text can be found in the Appendix. Circle = female; square = male; triangle = total/not available. F, femoral neck/hip; V, vertebrae/spine; W, wrist/forearm; H, humerus; M, multiple; O, other; N, not specified/general fragility fractures
a South Korea osteoporosis prevalence. b South Korea fracture incidence. Connected lines represent “estimated” data reflecting findings for broad age ranges (e.g. 60–75, 50 +); these data were noted as linked data points for all age categories included in the reported range. Each color represents a single study. “All adults” represents generalized data describing broad populations without specified age groups (e.g. “Five percent of Australian men have osteoporosis”). Full citations for studies not cited in-text can be found in the Appendix. Circle = female; square = male; triangle = total/not available. F, femoral neck/hip; V, vertebrae/spine; W, wrist/forearm; H, humerus; M, multiple; O, other; N, not specified/general fragility fractures
a Taiwan osteoporosis prevalence. b Taiwan fracture incidence. Connected lines represent “estimated” data reflecting findings for broad age ranges (e.g. 60–75, 50 +); these data were noted as linked data points for all age categories included in the reported range. Each color represents a single study. “All adults” represents generalized data describing broad populations without specified age groups (e.g. “Five percent of Australian men have osteoporosis”). Full citations for studies not cited in-text can be found in the Appendix. Circle = female; square = male; triangle = total/not available. F, femoral neck/hip; V, vertebrae/spine; W, wrist/forearm; H, humerus; M, multiple; O, other; N, not specified/general fragility fractures
Australia
Total population estimates suggested that 3.5% of all Australians have osteoporosis [7], with the number rising to 8.8–10% among those aged 50 + [8, 9]. In women aged 50 + , prevalence of osteoporosis ranged from about 15–23% [9, 10], with estimates of more than 40% among the female population aged 60 + [11, 12]. There were few estimates for men and younger adults. Fracture incidence also appeared to rise with age; hip fracture incidence was frequently in the 100 s-500 s per 100,000 person-years for most adults aged 50 + [13,14,15,16], with estimates topping 1,000 and 2,400 among adults in their 70 s and 80 s, respectively [16, 17]. Estimates for general osteoporotic fractures suggested an annual incidence of 1000–6500 per 100,000 person-years [11, 18, 19].
China
True prevalence of osteoporosis was difficult to discern due to a wide range of estimates, many of which covered large age ranges. Among young women (< 40 years), the rate appeared to be less than 10% [20,21,22]. Estimates rose with age [20, 23, 24]; among women aged 70 + , no estimate was lower than 10%, and the majority were 20% or higher (with some approaching 80%) [25,26,27,28,29]. Most prevalence estimates among men were below 15% [20, 23, 26, 30, 31], although numerous estimates placed prevalence above 20% among men aged 40 + [25, 32,33,34]. Studies with narrow age ranges for fracture incidence demonstrated a clear rising trend for fragility fractures with advancing age [23, 35,36,37]. Most estimates placed incidence of fragility fractures of the hip at less than 500 per 100,000 person-years [35,36,37,38,39], although one study suggested the rate surpasses 1500 and 2400 per 100,000 for men and women aged 50 + , respectively [40].
Hong Kong
Hong Kong literature offered very few data on adults younger than 50 years [41, 42], and data on older individuals showed a wide range of osteoporosis prevalence, even among the oldest adults [43, 44]. However, point estimates for narrow age ranges suggested rising prevalence with age [45]. Otherwise, most prevalence estimates were below 15% for men and below 35% for women [43, 46, 47]. Fracture incidence data showed a more obvious trend for increases with age, with numerous estimates between 1000 and 3000 per 100,000 for hip fractures among adults aged 65 + [37, 49,50,51]. However, most estimates for vertebral, hip, or other fragility fractures in Hong Kong adults aged 50 + were less than 1000 per 100,000 person-years per fracture type [14, 38, 51,52,53].
Japan
Osteoporosis prevalence appeared to be low among men across most age groups, with most estimates at or lower than 5% until ages 70 + [54,55,56,57], at which point most estimates still suggested prevalence lower than 15% [54, 55, 58]. Prevalence among women trended higher than among men in every age group and also appeared to increase with age [54, 55, 58, 59], although few estimates were found for women under 50. Broad age group estimates of 40 + or 50 + had a wide prevalence range as well, from 5.8% to more than 40% [60, 61]. Narrower age group prevalence estimates suggested that after the age of 50, prevalence (starting below 10% in ages 50–59) grew 10–20% with each decade of life [54, 55]. Femoral neck fracture incidence also varied considerably (with several estimates below 500 per 100,000 person-years for both men and women aged 50 +) [62,63,64] but appeared to increase with age, surpassing 1300 per 100,000 person-years in women by age 80 + [37, 49]. Vertebral fractures may be similarly frequent among women and lower than 500 per 100,000 person-years for men [65, 66].
Singapore
Data on osteoporosis prevalence were limited and differed in their estimates, with one suggesting 8.5% prevalence among all adult men [67], one reporting 6.8% prevalence among women aged 45–69 [68], and two others of 35.7% and 59% among all adults aged 60 + [69, 70]. Nearly all femoral neck fracture incidence articles reported rates of 611 or fewer per 100,000 person-years for men and women aged 45 + [38, 63, 71,72,73], although a few estimates for women aged 75 + were much higher (up to 1369 per 100,000 person-years) [14, 37].
South Korea
Prevalence of osteoporosis appeared to rise with age among Korean women [74,75,76,77], with numerous estimates higher than 50% in age groups 60 + [77,78,79]. Wider age group estimates largely ranged between 20 and 45% for women aged 40 + and 50 + [80,81,82,83,84]. Most estimates for men suggested a prevalence of 15% or lower [80, 85,86,87], although some ranged from 20% to more than 40% for men aged 70 + [75, 77, 88]. The vast majority of fragility fracture incidence data suggested site-specific and combined rates below 500 per 100,000 person-years [37, 38, 89,90,91], although numerous estimates between 500 and 1000 per 100,000 and even higher were also found, especially for individuals aged 80 + [92,93,94,95,96,97].
Taiwan
The osteoporosis data for Taiwan were many and varied, but the majority of “all adult” estimates suggested a general population prevalence of 16% or lower [98,99,100,101]. Prevalence rose with age, especially among women [102,103,104,105], with numerous estimates suggesting 45% or more of all women aged 60 + or 65 + had osteoporosis [105,106,107,108]. The majority of the femoral neck fracture incidence estimates encompassed a wide age range (50 +) and suggested a rate of about 500 or fewer per 100,000 person-years [63, 109,110,111]. However, several estimates, particularly for those aged 70 + or 80 + , suggested an incidence closer to 1,500 or more per 100,000 person-years, even for men [37, 49, 112]. The data also suggested a general fragility fracture incidence of 1500 or more per 100,000 person-years among Taiwanese adults aged 50 + [99, 113].
Discussion
In total, 316 papers were obtained discussing at least one of the two primary outcomes of interest, providing a detailed overview of the prevalence and incidence of osteoporosis and related fractures in Australia, China, Hong Kong, Japan, Singapore, South Korea, and Taiwan. The preponderance of evidence from this study suggests that 5–10% or more of all adults in these seven developed economies suffer from osteoporosis. This is likely an underestimate due to a lack of formal or frequent testing, the silent nature of the disease prior to fractures, and the tendency not to medically treat the condition, which may leave many people unaware of their status (even after low-trauma fractures), and result in a lack of data in treatment-based databases. This study reflects a higher osteoporosis prevalence in many populations aged 50 + (20–40% and sometimes much higher), especially among women. High-end estimates of osteoporosis exceeded 50% in elderly female populations in many locations.
In most of the locations, estimates for hip fracture ranged between 500 and 1000 cases per 100,000 person-years, although estimates two or three times that rate became more common with increased age. Vertebral fracture incidence was most often reported between 200 and 600 cases per 100,000 person-years. Estimates of non-specified or general fragility fractures, or data reporting multiple types of fractures as a combined incidence, suggest that these locations have an overall fracture incidence of up to 2000 per 100,000 person-years, with some much higher and many (likely not all-inclusive fracture estimates) slightly below 1000 per 100,000.
Studies published after the period of this review offer further data supporting the substantial prevalence of osteoporosis and related fractures in these locations. A recent Australian study reported secondary data suggesting that 20% of men and women aged 50 + will experience a vertebral fragility fracture and that this risk increases with age [114]. Recent literature in China supported osteoporosis prevalence estimates of 20–40% for women and near or less than 10% among men [115,116,117,118,119,120,121], with related fracture incidence in the low hundreds per 100,000 person-years for adults aged 50 + [122]. Recent literature suggested a general osteoporotic fracture incidence of 971 per 100,000 person-years among women in Japan [123]. In Singapore, recent estimates range from 9.3 to 19.4% [124, 125] for the prevalence of osteoporosis among postmenopausal women and 0.7% among men aged 50 + [124]. One large Singaporean fracture database study reported that 7% of women ages 50 + had a history of fragility fracture [126], and a study examining hip fracture incidence in adults ages 50 + reported age-adjusted incidence of 253 per 100,000 among women and 125 among men [127]. Another study from Singapore reported estimated vertebral fracture rates of 300 and 130 per 100,000 for women and men, respectively, and other osteoporotic fracture rates of 465 and 205 per 100,000 for women and men, respectively [128]. In South Korea, osteoporosis prevalence was recently reported to be 22.4% among adults aged 50 + [129]. Another South Korean study found a prevalence of 3.97% and 6.93% among all Koreans taking part in its National Health Insurance and Medical Aid programs, respectively, with an incidence of osteoporotic vertebral fractures of 389–408 per 100,000 person-years in Medical Aid recipients [130]; another study found that 17.9% of patients with a fragility fracture experienced a subsequent fracture, usually in less than 1 year [131]. In Taiwan, a large study reported osteoporosis prevalence of 18.13% in women and 17.95% in men aged 40 + [132]. Another Taiwanese study reported the combined incidence of developing osteoporosis or suffering a fragility fracture to be 23.8 per 1,000 person-years [133].
It is clear that osteoporosis and associated fractures are a health issue of significant import for these AP countries and regions. In our review, the most robust data were available for adults in middle to late age, and osteoporosis and related fractures were generally more common among women than men. Due to the large and growing elderly populations in the AP region, the reported rates of osteoporosis can be expected to produce growing numbers of annual hip and other osteoporotic fractures in many nations, with significant mortality and consequences for economic, societal, and population health.
Policy and economic implications
A systematic review in 2017 suggested that the economic burden of hip fracture in Asia may exceed one-third of gross domestic product per capita once indirect and intangible costs are considered [134]. In Singapore alone, it is estimated that increased treatment of osteoporosis could avoid nearly 30,000 fractures from 2017–2035, and result in a cost savings of more than SGD330 million in that time period [128]. As osteoporosis and related fractures can result in significant health expenditures, lost work time and productivity, reduced quality of life, and reduced relative survival [135, 136], it behooves governments and healthcare systems in the AP region to consider how best to implement policies and processes for preventing osteoporosis, identifying it and its risk factors in adult men and women, and managing affected populations, in order to reduce the risk of initial and subsequent fractures.
The data obtained and reviewed for this study can potentially inform additional research on osteoporosis, related fractures, and their impact in the AP region, as well as subpopulation research to better understand osteoporosis incidence and prevalence among adults with common comorbidities. This can then translate into public education, awareness, and screening campaigns and pave the way for policy and healthcare funding agency decision-making about osteoporosis treatment and fracture prevention.
Recommendations
Based on the data reviewed in this study and related data available on the known impact of osteoporosis and related fractures, we recommend stage-based opportunities for improvement to healthcare policy decision-makers and ministries of health in the AP region.
Screening, diagnosis, and fracture risk prediction
-
Implement broad screening efforts via public health programs or government health services to identify individuals with low bone density requiring treatment, starting at sex-specific ages appropriate for each nation’s population and using country-specific screening thresholds.
-
Promote innovative, targeted population awareness and risk assessment efforts via targeted and accessible resources, such as web-based health screening campaigns (e.g., the Know Your Bones™ online tool).
-
Invest in high-quality equipment (e.g., dual-energy x-ray absorptiometry (DXA) scanners) to standardize diagnostic and data collection efforts.
-
Recognize the need for ethnic-specific fracture risk prediction tools and encourage their development.
Treatment
-
Identify osteoporosis and related fracture management as key national priorities to drive recognition and commitment to improved outcomes.
-
Consider applying the APCO Framework of minimum clinical standards to implement standard practices to benchmark care and data monitoring for osteoporosis screening, diagnosis and management, and fracture prevention [137], or use existing national guidelines where available.
-
Implement preventive and therapeutic drug coverage in government health insurance plans. Particularly for generics, drug costs are low and the financial savings compared to treatment of fractures (together with the tangential costs associated with fractures) may be substantial [138,139,140].
-
Identify culturally relevant strategies to improve appropriate drug prescription practice, patient adherence, and lifestyle approaches to disease prevention and management.
Fracture prevention
-
Develop and deploy systematic fracture liaison services; these have been demonstrated to be effective programs for individuals at high risk of second/subsequent fractures. They can reduce future fractures, improve quality of life, and reduce costs associated with further fractures [141,142,143,144].
-
Initiate a fracture registry to track initial (and subsequent) osteoporotic fractures and follow-up clinical care. This data allows national benchmarking and identification of patients eligible for fracture liaison services or osteoporosis treatment.
Research
-
Implement data collection efforts to track the prevalence of osteoporosis and related fractures, as well as the impact of any changes in policies or interventions.
-
Develop regional or population-specific reference data to better define osteoporosis and low bone mineral density cut-offs in terms of bone density for populations in the AP region.
-
Explore, through cost-effectiveness analyses and mortality risk reduction rates, the impact of treatment and prevention efforts targeted at osteoporosis and fragility fractures.
Limitations
There are some limitations to this review. There was substantial variation in the data available and in the probable generalizability of the data. This was expected due to multiple reasons, including differences in resources and variations in reference groups for young BMD comparisons for T-scores. It has been shown that southeast Asians have lower BMD than Caucasians [145], and an overestimation of osteoporosis is likely if Caucasian normative data are used to determine T-scores [146, 147]. It is difficult to draw any conclusive comparisons regarding the rates of osteoporosis and related fractures in the locations of interest, due to the differences in the studies’ reported data age ranges; definitions of the conditions of interest and outcomes reported; highly varied cultural, ethnic, and geographic groups; statistical adjustments to data; measurement sites, bone mineral density measurement device types, and reference data for BMD measurements; inclusion of secondary data and self-reported data; and time periods for original data collection. These variations limit comparisons across, and even within, the selected locations. Without further refining the data to allow direct comparison of more standardized populations, it will be difficult to reliably estimate osteoporosis prevalence and related fractures in the AP region.
The quality of some of the data collected may limit the validity of summary conclusions, even within the included locations. Many of the studies included in this review reported secondary data or small group/sub-population findings, which, together with quality limitations for some studies, reduce the generalizability of the findings. It is also probable that many “all adult” estimates reported as secondary data represented narrower groups in their original studies, which could result in overestimations when reported as a figure for the entire adult population. Potential publication bias or bias stemming from oversampling of the most at-risk populations by virtue of gathering participants from hospitals and adults already engaged in bone health cohort studies, as numerous studies did, could also result in overestimation of the problem.
Variation in osteoporosis definitions and technology, such as DXA versus quantitative ultrasound (QUS), makes some of the data difficult to compare; DXA is not widely available in rural or low-income areas, so this problem is likely to persist in the AP region. This is further complicated by a lack of local population reference BMD T-score values for both technologies. Numerous studies reported sizeable differences in prevalence estimates based on the reference data and scan site. It is possible that studies using Caucasian reference data, or even non-native Asian reference databases, do not provide accurate or appropriate estimates for certain AP populations. Until more localized reference datasets for BMD in young, healthy individuals can be obtained, however, this problem will affect many of the region’s osteoporosis findings.
Finally, this study did not include local language results or papers older than ten years at the time of execution due to the volume of search results eligible for full-text review.
Conclusion
The highly inclusive nature of the review criteria resulted in a robust collection of estimates for each location of interest. Furthermore, the locations included in this study are some of the most economically and medically advanced in the AP region. As such, it is likely that our review may represent some of the best osteoporosis research available in this part of the world. It behooves clinicians and governments in the AP region to address the high occurrence of osteoporosis and related fractures through proactive prevention and treatment programs. Economies that ignore the broad population threat of this disease do so at their peril.
References
Mithal A, Ebeling P (2013) The Asia-Pacific Regional Audit: Epidemiology, costs & burden of osteoporosis in 2013. International Osteoporosis Foundation. Nyon, Switzerland. https://www.osteoporosis.foundation/educational-hub/files/asia-pacific-regional-audit-2013. Accessed 11 Nov 2021
Panula J, Pihlajamäki H, Mattila VM et al (2011) Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord 12:105. https://doi.org/10.1186/1471-2474-12-105
Schnell S, Friedman SM, Mendelson DA, Bingham KW, Kates SL (2010) The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil 1(1):6–14. https://doi.org/10.1177/2151458510378105
Higgins JPT, Green S (eds.) (2011) Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. https://handbook-5-1.cochrane.org. Accessed 11 Nov 2021
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100. https://doi.org/10.1136/bmj.b2700
NHLBI. Quality assessment tool for observational cohort and cross-sectional studies (2013). National Heart, Lung, and Blood Institute. National Institutes of Health. Retrieved from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 27 Aug 2021
Macgregor CB, Meerkin JD, Alley SJ, Vandelanotte C, Reaburn PJ (2018) Osteoporosis and low bone mineral density (osteopenia) in rural and remote Queensland. Aust J Rural Health 26(5):369–374
Waters DL, Hale L, Grant AM, Herbison P, Goulding A (2010) Osteoporosis and gait and balance disturbances in older sarcopenic obese New Zealanders. Osteoporos Int 21(2):351–357
Osteoporosis National Action Plan Working Group. Osteoporosis National Action Plan (2016). Osteoporosis National Action Plan Working Group; Sydney, Australia: 2016. Retrieved from: https://www.anzbms.org.au/downloads/OsteoporosisNationalActionPlan2016.pdf. Accessed November 2021
Modi A, Ebeling PR, Lee MS et al (2015) Medication use patterns, treatment satisfaction, and inadequate control of osteoporosis study in the Asia-Pacific region (MUSIC OS-AP): design of a multinational, prospective, observational study examining the impact of gastrointestinal events on osteoporosis management in postmenopausal women. Bone Rep 3:61–66
Australian Institute of Health and Welfare. Estimating the prevalence of osteoporosis in Australia. (2014) Retrieved from https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/estimating-the-prevalence-of-osteoporosis-in-austr/contents/summary. Accessed November 2021
Watts J, Abimanyi-Ochom J, Sanders K. (2013) Osteoporosis costing all Australians. A new burden of disease analysis – 2012 to 2022. Osteoporosis Australia. Australia. Glebe, NSW, Australia. https://healthybonesaustralia.org.au/wp-content/uploads/2020/11/Burden-of-Disease-Analysis-2012-2022.pdf. Accessed 23 Jan 2023
Brennan SL, Pasco JA, Urqhart DM, Oldenburg B, Hanna FS, Wluka AE (2010) The association between urban or rural locality and hip fracture in community-based adults: a systematic review. J Epidemiol Community Health 64:656–665
Bow CH, Cheung E, Cheung CL et al (2012) Ethnic difference of clinical vertebral fracture risk. Osteoporos Int 23(3):879–885
Dhanwal DK, Cooper C, Dennison EM (2010) Geographic variation in osteoporotic hip fracture incidence: the growing importance of asian influences in coming decades. J Osteoporos 2010:5
Pasco JA, Brennan SL, Henry MJ et al (2011) Changes in hip fracture rates in southeastern Australia spanning the period 1994–2007. J Bone Miner Res 26(7):1648–1654
Fisher A, O’Brien E, Davis M (2009) Trends in hip fracture epidemiology in Australia: possible impact of bisphosphonates and hormone replacement therapy. Bone 45(2):246–253
Brennan SL, Holloway KL, Williams LJ et al (2015) The social gradient of fractures at any skeletal site in men and women: data from the Geelong Osteoporosis Study Fracture Grid. Osteoporos Int 26(4):1351–1359
Sanders KM, Stuart AL, Williamson EJ et al (2010) Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA 303(18):1815–1822
Chen P, Li Z, Hu Y (2016) Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health 16(1):1039
Cui R, Zhou L, Li Z, Li Q, Qi Z, Zhang J (2016) Assessment risk of osteoporosis in Chinese people: relationship among body mass index, serum lipid profiles, blood glucose, and bone mineral density. Clin Interv Aging 11:887–895
Li S, He H, Ding M, He C (2010) The correlation of osteoporosis to clinical features: a study of 4382 female cases of a hospital cohort with musculoskeletal symptoms in Southwest China. BMC Musculoskelet Disord 11:183
Si L, Winzenberg TM, Jiang Q, Chen M, Palmer J (2015) Projection of osteoporosis-related fractures and costs in China: 2010–2050. Osteoporos Int 26(7):1929–1937. https://doi.org/10.1007/s00198-015-3093-2
Zhang ZQ, Ho SC, Chen ZQ, Zhang CX, Chen YM (2014) Reference values of bone mineral density and prevalence of osteoporosis in Chinese adults. Osteoporos Int 25(2):497–507
Mengmeng Z, Yagang L, Ying L, Xuena P, Binbin L, Liu Z (2012) A study of bone mineral density and prevalence of osteoporosis in Chinese people of Han nationality from Changchun. Arch Osteoporos 7:31–36
Mithal A, Kaur P (2012) Osteoporosis in Asia: a call to action. Curr Osteoporos Rep 10(4):245–247
Yang Y, Wang B, Fei Q et al (2013) Validation of an osteoporosis self-assessment tool to identify primary osteoporosis and new osteoporotic vertebral fractures in postmenopausal Chinese women in Beijing. BMC Musculoskelet Disord 14:271
Lian XL, Zhang YP, Li X, Jing LD, Cairang ZM, Gou JQ (2017) Exploration on the relationship between the elderly osteoporosis and cardiovascular disease risk factors. Eur Rev Med Pharmacol Sci 21(19):4386–4390
Li YZ, Zhuang HF, Cai SQ et al (2018) Low grip strength is a strong risk factor of osteoporosis in postmenopausal women. Orthop Surg 10(1):17–22
Yan D-d, Wang J, Hou X-h, Bao Y-q, Zhang Z-l, Hu C et al (2017) Association of serum uric acid levels with osteoporosis and bone turnover markers in a Chinese population. Acta Pharmacol Sin 39(4):626–632
Zhang X, Lin J, Yang Y et al (2018) Comparison of three tools for predicting primary osteoporosis in an elderly male population in Beijing: a cross-sectional study. Clin Interv Aging 13:201–209
Wang Y, Tao Y, Hyman ME, Li J, Chen Y (2009) Osteoporosis in China. Osteoporos Int 20(10):1651–1662
Huang JY, Song WZ, Huang M (2017) Effectiveness of osteoporosis self-assessment tool for Asians in screening for osteoporosis in healthy males over 40 years old in China. J Clin Densitom 20(2):153–159
Lv Y, Wang P, Huang R et al (2017) Cadmium exposure and osteoporosis: a population-based study and benchmark dose estimation in Southern China. J Bone Miner Res 32(10):1990–2000
Wang J, Wang Y, Liu WD, Wang F, Yin ZS (2014) Hip fractures in Hefei, China: the Hefei osteoporosis project. J Bone Miner Metab 32(2):206–214
Tian FM, Sun XX, Liu JY, Liu ZK, Liang CY, Zhang L (2017) Unparallel gender-specific changes in the incidence of hip fractures in Tangshan, China. Arch Osteoporos 12(1):18
Cheung CL, Ang SB, Chadha M et al (2018) An updated hip fracture projection in Asia: the Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia 4(1):16–21
Mithal A, Dhingra V, Lau E (2009) The Asian audit: epidemiology, costs and burden of osteoporosis in Asia 2009. International Osteoporosis Foundation. https://www.osteoporosis.foundation/sites/iofbonehealth/files/2019-06/2009_Asian_Audit_English.pdf. Accessed 23 Jan 2023
Wang XF, Seeman E (2012) Epidemiology and structural basis of racial differences in fragility fractures in Chinese and Caucasians. Osteoporos Int 23:411–422
Yuan L-Q, Lin X, Xiong D et al (2015) Epidemiology and management of osteoporosis in the People’s Republic of China: current perspectives. Clin Interv Aging 10:1017–1033
Cheung EY, Bow CH, Cheung CL et al (2012) Discriminative value of FRAX for fracture prediction in a cohort of Chinese postmenopausal women. Osteoporos Int 23(3):871–878
Chow LWC, Cheung M, Chu J, Li I (2017) A survey of osteoporosis and breast cancer risk perception among menopausal and postmenopausal women in Hong Kong. Menopausal Med 7(23):102–107
Woo J, Leung J, Lau E (2009) Prevalence and correlates of musculoskeletal pain in Chinese elderly and the impact on 4-year physical function and quality of life. Public Health 123(8):549–556
Deng M, Zeng XJ, He L-C et al (2017) Osteoporotic vertebral fracture prevalence in elderly Chinese men and women: a comparison of endplate/cortex fracture–based and morphometrical deformity–based methods. J Clin Densitom 22(3):409–419
Lau EMC, Chung HL, Ha PC, Tang H, Lam D (2015) Bone mineral density, anthropometric indices, and the prevalence of osteoporosis in Northern (Beijing) Chinese and Southern (Hong Kong) Chinese women—the largest comparative study to date. J Clin Densitom 18(4):519–524
Lee C, Lam S, Tsang A, Ng B, Leung J, Chong A (2015) Preliminary investigation on prevalence of osteoporosis and osteopenia: should we tune our focus on healthy adults? Jpn J Nurs Sci 12:232–248
Kwok A, Leung J, Chan A et al (2012) Prevalence of vertebral fracture in Asian men and women: comparison between Hong Kong, Thailand, Indonesia and Japan. Public Health 126(6):523–531
Tsang SW, Kung AW, Kanis JA, Johansson H, Oden A (2009) Ten-year fracture probability in Hong Kong Southern Chinese according to age and BMD femoral neck T-scores. Osteoporos Int 20(11):1939–1945
Cheung EYN, Tan KCB, Cheung CL, Kung AWC (2016) Osteoporosis in East Asia: current issues in assessment and management. Osteoporos and Sarcopenia 2(3):118–133
Ip T, Cheung S, Cheung T et al (2013) The Osteoporosis Society of Hong Kong (OSHK): 2013 OSHK guideline for clinical management of postmenopausal osteoporosis in Hong Kong. Hong Kong Med J 19(Suppl 2):1–40
Chau PH, Wong M, Lee A, Ling M, Woo J (2013) Trends in hip fracture incidence and mortality in Chinese population from Hong Kong 2001–09. Age Ageing 42:229–233
Ballane G, Cauley JA, Luckey MM, El-Hajj FG (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28(5):1531–1542
Kanis JA, Oden A, McCloskey EV et al (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
Yoshimura N, Muraki S, Oka H, Kawaguchi H, Nakamura K, Akune T (2010) Cohort profile: research on Osteoarthritis/Osteoporosis Against Disability study. Int J Epidemiol 39:988–995
Yoshimura N, Muraki S, Nakamura K, Tanaka S (2017) Epidemiology of the locomotive syndrome: the research on osteoarthritis/osteoporosis against disability study 2005–2015. Mod Rheumatol 27(1):1–7
Ikegami S, Kamimura M, Uchiyama S, Mukaiyama K, Kato H (2014) Unilateral vs bilateral hip bone mineral density measurement for the diagnosis of osteoporosis. J Clin Densitom 17(1):84–90
Iki M, Fujita Y, Tamaki J, Kouda K, Yura A, Kadowaki E et al (2009) Design and baseline characteristics of a prospective cohort study for determinants of osteoporotic fracture in community-dwelling elderly Japanese men: the Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) Study. BMC Musculoskelet Disord 10:165
Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O’Malley CD (2014) Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Ostoporos 9(1):182
Tajika T, Yamamoto A, Ohsawa T, Oya N, Iizuka H, Takagishi K (2016) predictors of bone status by quantitative ultrasound measurements in a mountain village in Japan. Open Orthop J 10:559–568
Yamamoto LA, DiBonaventura M, Kawaguchi I (2016) The association between osteoporosis and patient outcomes in Japan. J Med Econ 19(7):702–709
Iki M, Tamaki J, Kadowaki E et al (2014) Japanese women over 10 years independently of bone density and prevalent vertebral deformity: the Japanese Population-Based Osteoporosis (Jpos) cohort study. J Bone Miner Metab 29(2):399–407
Mori T, Tamiya N, Jin X et al (2018) Estimated expenditures for hip fractures using merged healthcare insurance data for individuals aged ≥75 years and long-term care insurance claims data in Japan. Arch Osteoporos 13(1):37
Cheng S, Levy A, Lefaivre K, Guy P, Kuramoto L, Sobolev B (2011) Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int 22:2575–2586
Vijayakumar R, Büsselberg D (2016) Osteoporosis: An under-recognized public health problem: local and global risk factors and its regional and worldwide prevalence. J Local Glob Health Sci 2. https://doi.org/10.5339/jlghs.2016.2
Tsukutani Y, Hagino H, Ito Y, Nagashima H (2015) Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporos Int 26(9):2249–2255
Sakuma M, Endo N, Oinuma T et al (2014) Incidence of osteoporotic fractures in Sado, Japan in 2010. J Bone Miner Metab 32(2):200–205
Goh VHH, Hart WG (2016) Aging, lifestyle factors, hormones and bone health in Singaporean men. Bone Rep 5:110–6
Logan S, Thu WPP, Lay WK, Wang LY, Cauley JA, Yong EL (2017) Chronic joint pain and handgrip strength correlates with osteoporosis in mid-life women: a Singaporean cohort. Osteoporos Int 28(9):2633–2643
Daruwalla ZJ, Huq SS, Wong KL et al (2016) Hip fractures, preceding distal radius fractures and screening for osteoporosis: should we be screening earlier? A minimum 10-year retrospective cohort study at a single centre. Osteoporos Int 27(1):361–366
Chan D, Mamun K (2018) To find out the prevalence of osteoporosis and treatment provided to elderly patients in a community hospital in Singapore. Osteoporos Int 29:P370
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV (2016) A systematic review of intervention thresholds based on FRAX : a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25
Dhanwal DK, Dennison EM, Harvey NC, Cooper C (2011) Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop 45(1):15–22
Xie H, Loh S, Shan CP, Wang J, Peng Y, Fen LQ, Kannusamy P, Lien PC, Parasuram R (2012) Osteoporosis in adults with mental illnesses: a systematic review. JBI Libr Syst Rev 10(56 Suppl):1–20. https://doi.org/10.11124/01938924-201210561-00022
Kung A, Fan T, Xu L et al (2013) Factors influencing diagnosis and treatment of osteoporosis after a fragility fracture among postmenopausal women in Asian countries: a retrospective study. BMC Women’s Health 13:7
Lee S, Choi M-G, Yu J et al (2015) The effects of the Korean reference value on the prevalence of osteoporosis and the prediction of fracture risk. BMC Musculoskelet Disord 16(1):69
Lim YS, Lee SW, Tserendejib Z, Jeong S-Y, Go G, Park H-R (2015) Prevalence of osteoporosis according to nutrient and food group intake levels in Korean postmenopausal women: using the 2010 Korea National Health and Nutrition Examination Survey Data. Nutr Res Pract 9(5):539–546
Kwon Y-J, Park KS, Choi BH, Kim B-S, Ha Y-C (2017) Prevalence of osteoporosis and effectiveness of screening test using ultrasound bone densitometry and education in a community-dwelling population. J Korean Med Sci 32(2):352–356
Kim W, Gong HS, Lee SH, Park JW, Kim K, Baek GH (2017) Low evaluation rate for osteoporosis among patients presenting with a rib fracture. Arch Osteoporos 12(1):61
Jung HJ, Park HY, Kim JS, Yoon JO, Jeon IH (2016) Bone mineral density and prevalence of osteoporosis in postmenopausal Korean women with low-energy distal radius fractures. J Korean Med Sci 31(6):972–975
Baek K, Lin Y, Kang M (2017) Prevalence of osteoporosis and rate of bone loss in Korean adults: the Chungju metabolic disease cohort study. Osteoporos Int 28:P308
Choi HS, Park SY, Kim YM, Kim SH, Kim KM, Chung YS (2016) Medical treatment of severe osteoporosis including new concept of advanced severe osteoporosis. Osteoporos Sarcopenia 2(1):13–19
Kim JW, Jeon YJ, Baek DH, Kim TN, Chang JS (2014) Percentage of the population at high risk of osteoporotic fracture in South Korea: analysis of the 2010 Fifth Korean National Health and Nutrition Examination survey data. Osteoporos Int 25(4):1313–1319
Kim OS, Shin MH, Song IH et al (2016) Digital panoramic radiographs are useful for diagnosis of osteoporosis in Korean postmenopausal women. Gerodontology 33(2):185–192
Park S-J, Jung JH, Kim M-S, Lee H-J (2018) High dairy products intake reduces osteoporosis risk in Korean postmenopausal women: a 4 year follow-up study. Nutr Res Pract 12(5):436–442
Kim J, Lee J, Shin J-Y, Park B-J (2015) Socioeconomic disparities in osteoporosis prevalence: different results in the overall Korean adult population and single-person households. J Prev Med Public Health 48(2):84
Noh JW, Park H, Kim M, Kwon YD (2018) Gender differences and socioeconomic factors related to osteoporosis: a cross-sectional analysis of nationally representative data. J Women’s Health 27(2):196–202
Oh SM, Song BM, Nam BH et al (2016) Development and validation of osteoporosis risk-assessment model for Korean men. Yonsei Med J 57(1):187–196
Lim Y, Kim K, Ko SH et al (2016) Gender- and age-group-specific associations between physical performance and bone mineral density, falls, and osteoporotic fractures in Koreans: the Chungju Metabolic Disease Cohort study. J Bone Miner Metab 34(3):336–346
Yoon BH, Lee YK, Kim SC, Kim SH, Ha YC, Koo KH (2013) Epidemiology of proximal femoral fractures in South Korea. Arch Osteoporos 8:157
Kang H, Yang K, Kim Y et al (2010) Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health 10:230
Yoo JH, Moon SH, Ha YC et al (2015) Osteoporotic fracture: 2015 position statement of the Korean Society for Bone and Mineral Research. J Bone Metab 22(4):175–181
Kim TI, Choi JH, Kim SH, Oh JH (2016) The adequacy of diagnosis and treatment for osteoporosis in patients with proximal humeral fractures. Clin Orthop Surg 8(3):274–279
Lee YK, Yoon BH, Koo K-H (2013) Epidemiology of osteoporosis and osteoporotic fractures in South Korea. Endocrinol Metab 28(2):90–93
Kim SR, Park YG, Kang SY, Nam K, Park Y, Ha Y (2014) Undertreatment Of osteoporosis following hip fractures in Jeju cohort study. Bone 21(4):263–268
Kim HY, Jang EJ, Park B et al (2016) Development of a Korean Fracture Risk Score (KFRS) for predicting osteoporotic fracture risk: analysis of data from the Korean National Health Insurance Service. PLoS One 11(7):e0158918
Ha Y-C, Park Y-G, Nam KW, Kim S-R (2015) Trend in hip fracture incidence and mortality in Korea: a prospective cohort study from 2002 to 2011. J Korean Med Sci 30(4):483–488
Cauley J (2011) Defining ethnic and racial differences in osteoporosis and fragility fractures. Clin Orthop Relat Res 469:1891–1899
Lin L-P, Hsu S-W, Yao C-H et al (2015) Risk for osteopenia and osteoporosis in institution-dwelling individuals with intellectual and/or developmental disabilities. Res Dev Disabil 36:108–113
Liao C, Lin C, Shih C et al (2014) Increased risk of fracture and postfracture adverse events in patients with diabetes: two nationwide population-based retrospective cohort studies. Diabetes Care 37:2246–2252
Yen C-M, Kuo C-L, Lin M-C et al (2014) Sleep disorders increase the risk of osteoporosis: a nationwide population-based cohort study. Sleep Med 15(11):1339–1344
Lin H, Huang C, Hwang L (2018) Association between metabolic syndrome and osteoporosis in Taiwanese middle-aged and elderly participants. Arch Osteoporos 13(1):48. https://doi.org/10.1007/s11657-018-0467-z
Yen CM, Muo CH, Lin MC, Chang SN, Chang YJ, Kao CH (2014) A nationwide population cohort study: irritable bowel syndrome is a risk factor of osteoporosis. Eur J Intern Med 25(1):87–91
Lin YC, Pan WH (2011) Bone mineral density in adults in Taiwan: results of the Nutrition and Health Survey in Taiwan 2005–2008 (NAHSIT 2005–2008). Asia Pac J Clin Nutr 20(2):283–291
Lu YC, Lin YC, Lin YK et al (2016) Prevalence of osteoporosis and low bone mass in older Chinese population based on bone mineral density at multiple skeletal sites. Sci Rep 6:25206
Li Y-M, Liu S-H (2010) Estimation of the 10-year probability of osteoporotic fracture in postmenopausal Taiwanese women with FRAX. Tzu Chi Med J 22(1):29–35
Wang WJ, Kuo KL, Liaw CK, Wu TY, Chie WC, Chen JM (2017) Bone health among older adults in Taiwan. Arch Gerontol Geriatr 70:155–161
Tung T (2017) Clinical investigation of prevalence and associated metabolic factors of osteoporosis among the female elderly agricultural and fishing population in Taiwan. Osteoporos Int 28:P793
Lin MR, Hwang HF, Lin PS, Chen CY (2014) Relations of osteoporosis and follow-up duration to recurrent falls in older men and women. Osteoporos Int 25(3):863–871
Wu CH, Tung YC, Lin TK et al (2016) Hip fracture in people with erectile dysfunction: a nationwide population-based cohort study. PLoS One 11(4):e0153467
Chen FP, Shyu YC, Fu TS et al (2017) Secular trends in incidence and recurrence rates of hip fracture: a nationwide population-based study. Osteoporos Int 28(3):811–818
Chan D-C, Lee Y-S, Wu Y-J et al (2013) A 12-year ecological study of hip fracture rates among older Taiwanese adults. Calcif Tissue Int 93(5):397–404
Lee SH, Cho EH, Ahn SH et al (2016) Prediction of future osteoporotic fracture occurrence by genetic profiling: a 6-year follow-up observational study. J Clin Endocrinol Metab 101(3):1215–1224
Liao W, Chang T, Chen H, Kao C (2015) Benign paroxysmal positional vertigo is associated with an increased risk of fracture: a population-based cohort study. J Orthop Sports Phys Ther 45(5):406–412
Ferreira ML, March L (2019) Vertebral fragility fractures - how to treat them? Best Pract Res Clin Rheumatol 33(2):227–235. https://doi.org/10.1016/j.berh.2019.03.017
Cui Z, Meng X, Feng H et al (2019) Estimation and projection about the standardized prevalence of osteoporosis in mainland China. Arch Osteoporos 15(1):2. https://doi.org/10.1007/s11657-019-0670-6
Shim JG, Kim DW, Ryu KH et al (2020) Application of machine learning approaches for osteoporosis risk prediction in postmenopausal women. Arch Osteoporos 15(1):169. https://doi.org/10.1007/s11657-020-00802-8
Qiao D, Liu X, Tu R et al (2020) Gender-specific prevalence and influencing factors of osteopenia and osteoporosis in Chinese rural population: the Henan Rural Cohort Study. BMJ Open 10(1):e028593. https://doi.org/10.1136/bmjopen-2018-028593
Zhang Q, Cai W, Wang G, Shen X (2020) Prevalence and contributing factors of osteoporosis in the elderly over 70 years old: an epidemiological study of several community health centers in Shanghai. Ann Palliat Med 9(2):231–238. https://doi.org/10.21037/apm.2020.02.09
Wang Y, Xie D, Li J et al (2019) Association between dietary selenium intake and the prevalence of osteoporosis: a cross-sectional study. BMC Musculoskelet Disord 20(1):585. https://doi.org/10.1186/s12891-019-2958-5
Zeng Q, Li N, Wang Q et al (2019) The prevalence of osteoporosis in China, a nationwide, multicenter DXA survey. J Bone Miner Res 34(10):1789–1797. https://doi.org/10.1002/jbmr.3757
Cheng X, Zhao K, Zha X et al (2021) China Health Big Data (China Biobank) project investigators. Opportunistic screening using low-dose CT and the prevalence of osteoporosis in China: a nationwide, multicenter study. J Bone Miner Res 36(3):427–435.https://doi.org/10.1002/jbmr.4187
Zhu Y, Xing X, Liu S, Chen W, Zhang X, Zhang Y (2020) Epidemiology of low-energy wrist, hip, and spine fractures in Chinese populations 50 years or older: a national population-based survey. Med (Baltimore) 99(5):e18531. https://doi.org/10.1097/MD.0000000000018531
Kojima A, Ikehara S, Kamiya K et al (2020) Natto intake is inversely associated with osteoporotic fracture risk in postmenopausal Japanese women. J Nutr 150(3):599–605. https://doi.org/10.1093/jn/nxz292
Chen KK, Wee SL, Pang BWJ et al (2020) Bone mineral density reference values in Singaporean adults and comparisons for osteoporosis establishment - the Yishun study. BMC Musculoskelet Disord 21(1):633. https://doi.org/10.1186/s12891-020-03646-y
Kalimeri M, Leek F, Wang NX et al (2020) Folate and Vitamin B-12 Status Is Associated With Bone Mineral Density and Hip Strength of Postmenopausal Chinese-Singaporean Women. JBMR Plus 4(10):e10399. https://doi.org/10.1002/jbm4.10399
Kanis JA, Chandran M, Chionh SB et al (2020) Use of age-dependent FRAX-based intervention thresholds for Singapore. Arch Osteoporos 15(1):104. https://doi.org/10.1007/s11657-020-00782-9
Yong EL, Ganesan G, Kramer MS, Logan S, Lau TC, Cauley JA, Tan KB (2019) Hip fractures in Singapore: ethnic differences and temporal trends in the new millennium. Osteoporos Int 30:879–886
Chandran M, Lau TC, Gagnon-Arpin I et al (2019) The health and economic burden of osteoporotic fractures in Singapore and the potential impact of increasing treatment rates through more pharmacological options. Arch Osteoporos 14(1):114
Ahn SH, Park SM, Park SY et al (2020) Osteoporosis and osteoporotic fracture fact sheet in Korea. J Bone Metab 27(4):281–290. https://doi.org/10.11005/jbm.2020.27.4.281
Park SB, Kim J, Jeong JH et al (2016) Prevalence and incidence of osteoporosis and osteoporotic vertebral fracture in Korea: nationwide epidemiological study focusing on differences in socioeconomic status. Spine (Phila Pa 1976) 41(4):328–36. https://doi.org/10.1097/BRS.0000000000001291
Park JA, Nam JH, Hong SH, Shim YB, Jeong J, Shin JY (2020) Economic burden of subsequent fracture in osteoporosis patients in South Korea. J Med Econ 23(12):1598–1605. https://doi.org/10.1080/13696998.2020.1831517
Erjiang E, Wang T, Yang L et al (2020) machine learning can improve clinical detection of low BMD: the DXA-HIP study. J Clin Densitom S1094–6950(20):30120–30127. https://doi.org/10.1016/j.jocd.2020.10.004
Lin SM, Wang CY, Chen YY, Wang JH, Liang CC, Huang HK (2019) Herpes zoster and the risks of osteoporosis and fracture: a nationwide cohort study. Eur J Clin Microbiol Infect Dis 38(2):365–372. https://doi.org/10.1007/s10096-018-3436-y
Mohd-Tahir NA, Li SC (2017) Economic burden of osteoporosis-related hip fracture in Asia: a systematic review. Osteoporos Int 28(7):2035–2044. https://doi.org/10.1007/s00198-017-3985-4
Fujiwara S, Zhao X, Teoh C, Jaffe DH, Taguchi Y (2019) Disease burden of fractures among patients with osteoporosis in Japan: health-related quality of life, work productivity and activity impairment, healthcare resource utilization, and economic costs. J Bone Miner Metab 37(2):307–318. https://doi.org/10.1007/s00774-018-0916-1
Cheung EYN, Tan KCB, Cheung CL, Kung AWC (2016) Osteoporosis in East Asia: current issues in assessment and management. Osteoporos Sarcopenia 2(3):118–133. https://doi.org/10.1016/j.afos.2016.07.001
Chandran M, Mitchell PJ, Amphansap T et al (2021) Development of the Asia Pacific Consortium on Osteoporosis (APCO) framework: clinical standards of care for the screening, diagnosis, and management of osteoporosis in the Asia-Pacific region [published correction appears in Osteoporos Int 32(7): 1277–1278 10.1007/s00198-021-05953-z]. Osteoporos Int 32(7):1249–1275. https://doi.org/10.1007/s00198-020-05742-0
Chandran M, Ganesan G, Tan KB, Reginster JY, Hiligsmann M (2021) Cost-effectiveness of FRAX®-based intervention thresholds for management of osteoporosis in Singaporean women. Osteoporos Int 32(1):133–144. https://doi.org/10.1007/s00198-020-05536-4
Chan DC, McCloskey EV, Chang CB, Lin KP, Lim LC, Tsai KS, Yang RS (2017) Establishing and evaluating FRAX® probability thresholds in Taiwan. J Formos Med Assoc 116(3):161–168. https://doi.org/10.1016/j.jfma.2016.03.006
You R, Zhang Y, Wu DB et al (2020) Cost-effectiveness of zoledronic acid versus oral alendronate for postmenopausal osteoporotic women in China. Front Pharmacol 11:456. https://doi.org/10.3389/fphar.2020.00456
Eisman JA, Bogoch ER, Dell R et al (2012) ASBMR Task Force on Secondary Fracture Prevention. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27(10):2039–2046. https://doi.org/10.1002/jbmr.1698
Moriwaki K, Noto S (2017) Economic evaluation of osteoporosis liaison service for secondary fracture prevention in postmenopausal osteoporosis patients with previous hip fracture in Japan. Osteoporos Int 28(2):621–632. https://doi.org/10.1007/s00198-016-3777-2
Jones AR, Herath M, Ebeling PR, Teede H, Vincent AJ (2021) Models of care for osteoporosis: a systematic scoping review of efficacy and implementation characteristics. EClinicalMedicine 38:101022. https://doi.org/10.1016/j.eclinm.2021.101022
Inderjeeth CA, Raymond WD, Briggs AM, Geelhoed E, Oldham D, Mountain D (2018) Implementation of the Western Australian Osteoporosis Model of Care: a fracture liaison service utilising emergency department information systems to identify patients with fragility fracture to improve current practice and reduce re-fracture rates: a 12-month analysis. Osteoporos Int 29(8):1759–1770. https://doi.org/10.1007/s00198-018-4526-5
Marquez MA, Melton LJ III, Muhs JM et al (2001) Bone density in an immigrant population from southeast Asia. Osteoporos Int 12:595–604
Ho-Pham LT, Nguyen UDT, Pham HN, Nguyen ND, Nguyen TV (2011) Reference ranges for bone mineral density and prevalence of osteoporosis in Vietnamese men and women. BMC Musculoskelet Disord 12:182. https://doi.org/10.1186/1471-2474-12-182
Lu Y-C, Lin YC, Lin Y-K, Liu Y-J, Chang K-H, Chieng P-U, Chan WP (2016) Prevalence of osteoporosis and low bone mass in older Chinese populations based on bone mineral density at multiple skeletal sites. Sci Rep 6:25206
Acknowledgements
The authors would like to acknowledge Lee-Anne Weston-Ford for her role in data verification and editing the manuscript, and Andre Morte, MD, for his role in conducting the literature search, data abstraction, data verification, and quality assessments.
Funding
Funding for this study was provided by Amgen, and employees of Amgen were involved in protocol development. Amgen had no role in data collection, data analysis, data interpretation, or writing of the report. Authors KB and JT were funded by Amgen to develop the protocol, conduct the literature review and data abstraction, and assist in preparation of this manuscript. The remaining authors were not compensated by Amgen for their role in the research or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
• MC was involved in data interpretation and manuscript writing, review, and editing.
• KB was involved in protocol development, management of the literature review and data abstraction process, data review and verification, data interpretation, and manuscript writing and editing.
• SF was involved in data interpretation and manuscript writing and review.
• YH was involved in data interpretation and manuscript writing and review.
• HT was involved in data interpretation and manuscript writing and review.
• JH was involved in data interpretation and manuscript writing and review.
• JT was involved in protocol development, oversight of the literature review and data abstraction, data verification, and manuscript writing and review.
• JE was involved in protocol development, data interpretation, and manuscript writing and review.
Corresponding author
Ethics declarations
Ethics approval
For this type of study, formal consent is not required.
Conflicts of interest
• MC has received honoraria from DKSH, Amgen, and Kyowa Kirin for chairing advisory boards and for speaking engagements.
• KB received funding from Amgen to lead the protocol development, oversee the systematic review research and data abstraction, and organize and interpret the data for publication. She has research and marketing consulting and medical writing contract relationships with numerous medical communications and consulting agencies, and therefore indirectly receives compensation from many pharmaceutical companies for her work on clinical trial endpoints, clinician education, medical communications, and medical marketing.
• SF, JH, YH, and HT have no interests to declare.
• JT received funding from Amgen to lead the protocol development, oversee the systematic review research and data abstraction, and organize the data for publication.
• JE has received research funding and consulting fees from Amgen, Lilly, MSD, and Theramex, and has served on advisory boards for Amgen and Theramex.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material (Appendix).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chandran, M., Brind’Amour, K., Fujiwara, S. et al. Prevalence of osteoporosis and incidence of related fractures in developed economies in the Asia Pacific region: a systematic review. Osteoporos Int 34, 1037–1053 (2023). https://doi.org/10.1007/s00198-022-06657-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06657-8