Abstract
Summary
We comprehensively described elderly Medicare women with an outpatient visit in 2011 and fracture within 2 years before. These women were at very high risk for subsequent fracture and high healthcare utilization and cost, especially those with vertebral or multiple fractures. However, rates of fracture prevention treatments were low.
Introduction
Postmenopausal women with osteoporosis are stratified to high and very-high fracture risk categories, and this categorization drives algorithms for osteoporosis management in osteoporosis treatment guidelines. This study comprehensively describes a very-high-risk cohort.
Methods
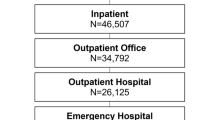
This retrospective cohort study used the Medicare 20% database; elderly women with an outpatient visit in 2011 and fracture within 2 years before the visit were included. Outcomes included fracture risk, all-cause and fracture-related healthcare resource utilization and cost, and osteoporosis medication use in the 5 years after the visit.
Results
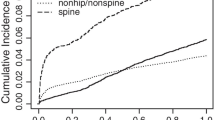
Overall, 43,193 patients were included. The 5-year probability was 0.36 for major fracture and 0.11 and 0.17 for hip fracture and vertebral fracture, respectively, much higher than the guidelines’ 10-year probability thresholds for very-high-risk (0.3 for major fracture, 0.045 for hip fracture). Rates of hospitalizations, emergency department visits or observation stays, and skilled nursing facility stays in year 1 were 53.7, 57.0, and 18.8 per 100 patient-years, respectively, decreasing slightly in subsequent years. Mean healthcare cost was $23,700 in year 1, decreasing to $18,500 in year 5. About 29.1% of patients received osteoporosis medications in year 1, decreasing to 16.9% by year 5. Rates for all outcomes, especially fractures, were much higher among vertebral and multiple fracture cohorts.
Conclusion
Elderly women with a fracture within last 2 years were at very-high-risk for subsequent fracture and high healthcare utilization and cost, especially those with vertebral or multiple fractures. However, rates of fracture prevention treatments were low. More effort is needed to identify and treat patients at very-high-risk for fracture.





Similar content being viewed by others
References
Wade SW, Strader C, Fitzpatrick LA, Anthony MS (2012) Sex- and age-specific incidence of non-traumatic fractures in selected industrialized countries. Arch Osteoporos 7:219–227
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413
United Nations. Department of Economic and Social Affairs, Population Division (2013) World population ageing 2013. ST/ESA/SER.A/348. 2013; Available at: http://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2013.pdf. Accessed June 23, 2020
Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J (2016) Quality of life after hip fracture in the elderly: a systematic literature review. Injury. 47(7):1369–1382
Burge R, Dawson-Hughes B, Solomon DH et al (2007) Incidence and economic burden of osteoporosis-related fractures in the United States 2005-2025. J Bone Miner Res 22:465–475
Weycker D, Li X, Barron R, Bornheimer R, Chandler D (2016) Hospitalizations for osteoporosis-related fractures: economic costs and clinical outcomes. Bone Rep 5:186–191
Singer A, Exuzides A, Spangler L et al (2015) Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 90(1):53–62
Dyer SM, Crotty M, Fairhall N, for the Fragility Fracture Network (FFN) et al (2016) Rehabilitation Research Special Interest Group. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16(1):158
Xiao P, Zhou Y (2020) Factors associated with the burden of family caregivers of elderly patients with femoral neck fracture: a cross-sectional study. J Orthop Surg Res 15:234. Published online 2020 Jun 23. doi: https://doi.org/10.1186/s13018-020-01749-9
Johansson H, Siggeirsdóttir K, Harver NC et al (2017) Imminent risk of fracture after fracture. Osteoporos Int. 28(3):775–780
Banefelt J, Åkesson KE, Spångéus A et al (2019) Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int 30(3):601–609
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297(4):387–394
Camacho PM, Petak SM, Binkley N et al (2020) American Association of Clinical Endocrinologists Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis - 2020 update. Endocr Pract 26(5):564–570. https://doi.org/10.4158/GL-2020-0524
Curtis JR, Mudano AS, Solomon DH, Xi J, Melton ME, Saag KG (2009) Identification and validation of vertebral compression fractures using administrative claims data. Med Care 47(1):69–72
Liu J, Guo H, Rai P, Pinto L, Barron R (2018) Medication persistence and risk of fracture among female Medicare beneficiaries diagnosed with osteoporosis. Osteoporos Int 29(11):2409–2417
Johnell O, Kanis JA, Oden A et al (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int. 15:175–179
Johnell O, Oden A, Caulin F, Kanis JA (2001) Acute and long term increase in fracture risk after hospitalization for vertebral fracture. Osteoporos Int. 12:207–214
Giangregorio LM, Leslie WD (2010) Manitoba Bone Density Program. Time since prior fracture is a risk modifier for 10-year osteoporotic fractures. J Bone Miner Res. 25:1400–1405
Hansen D, Bazell C, Pelizzari P, Pyenson B. Medicare cost of osteoporotic fractures, the clinical and cost burden of an important consequence of osteoporosis. Milliman Research Report, August 2019. http://assets.milliman.com/ektron/Medicare_cost_of_osteoporotic_fractures.pdf. Accessed October 19, 2020.
Lyles KW, Colon-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S, Trial HRF (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 357:1799–1809
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mitlak BH (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 344:1434–1441
Wang C-Y, Shau-Huai F, Yang R-S, Chen L-K, Shen L-J, Hsiao F-Y (2020) Timing of anti-osteoporosis medications initiation after a hip fracture affects the risk of subsequent fracture: a nationwide cohort study. Bone 138:115452
Kim S-M, Kang K-C, Kim JW, Lim S-J, Hahn MH (2017) Current role and application of teriparatide in fracture healing of osteoporotic patients: a systematic review. J Bone Metab 24(1):65–73
Centers for Medicare & Medicaid Services. Medicare utilization and payment section. Hospitalization. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMSProgramStatistics/2015/2015_Utilization#Medicare_Inpatient_Hospital. Accessed June 23, 2020.
Shane E, Burr D (2010) Peter R Ebeling, et al. (2010). Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 25(11):2267–2294
Khosla S, Cauley JA, Compston J, Kiel DP, Rosen C, Saag KG, Shane E (2017) Addressing the crisis in the treatment of osteoporosis: a path forward. J Bone Miner Res. 32(3):424–430
Kaiser Family Foundation. Medicare spending per enrollee by state. 2014. https://www.kff.org/medicare/state-indicator/per-enrollee-spending-by-residence/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed June 23, 2020.
Centers for Medicare & Medicaid Services. Medicare utilization and payment section. Utilization. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMSProgramStatistics/2015/2015_Utilization. Accessed June 23, 2020.
Acknowledgements
The authors thank Chronic Disease Research Group colleague Mary Van Beusekom, MS, ELS, for manuscript editing.
Availability of data and material
The Medicare data used for this study was licensed through the Centers for Medicare & Medicaid Services and cannot be shared outside of that agreement.
Code availability
Proprietary programming code was developed to analyze the Medicare data and not available outside of the study team.
Funding
This study was supported by Amgen Inc., Thousand Oaks, CA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Institutional review board approval was obtained through the Hennepin Healthcare Research Institute, Office for Human Subjects Research.
Conflicts of interest
MO, SRG, and XX are employees of Amgen and stockholders; JL and TG are employees of CDRG and CDRG received research support from Amgen; and KNF is employee of Strategic Healthcare Solutions and contracted with Amgen.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, J., Gong, T., Xu, X. et al. Heavy clinical and economic burden of osteoporotic fracture among elderly female Medicare beneficiaries. Osteoporos Int 33, 413–423 (2022). https://doi.org/10.1007/s00198-021-06084-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06084-1