Abstract
Summary
Semi-automatic morphometry is highly reproducible and not time intensive; however, no study has evaluated agreement between semi-automated morphometric methods and the Genant semi-quantitative method performed as a rule by radiologists. Our study shows substantial agreement between both methods; however, semi-automatic morphometry upgrades mild deformities and overestimates the prevalence of fractures.
Introduction
The aim of this study was to evaluate the agreement between radiologists using the Genant semi-quantitative (SQ) method and semi-automated morphometry in the diagnosis of vertebral fractures in post-menopausal women.
Methods
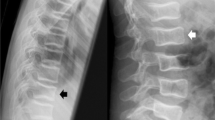
Cross-sectional study was conducted in 2006–2007 in an age-stratified population-based sample of 824 post-menopausal women over the age of 50. From this population two sets of 95 and 50 X-ray were randomly extracted to test inter-rater agreement and agreement between SQ and semi-automated morphometry, and vertebral fractures were classified according to both methods. The Genant method was used to homogenise the diagnosis of fractures. Agreement was evaluated with weighted kappa. We evaluated each vertebral body independently and also the whole vertebral column (T4–L4) classifying women into the worst grade of fracture. For the qualitative interpretation of the agreement, we used the criteria described by Landis and Koch (Biometrics 33:159–174, 1977).
Results
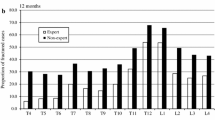
The radiologists' agreement was 98.4% (Kappa, 0.75; 95% CI, 0.42–0.89). Agreement between semi-automated morphometry and SQ reached 97.6% and Kappa was 0.86 (95% CI, 0.66–0.94). In the whole evaluation of the spine semi-automated morphometry overestimates, the prevalence of fractures compared with the radiologists were 15.8% of women with fractures and 7.4% of women with moderate–severe fractures by semi-automated morphometry vs. 8.4% and 3.2% by the SQ method. The negative predictive value for MorphoXpress was 99% while the positive was 40%.
Conclusions
Semi-automated morphometry shows high reliability and a substantial agreement with the SQ approach but overestimates the prevalence of fractures. Its role in routine clinical practice is limited because positive results should be reassessed by qualitative or semi-quantitative methods.

Similar content being viewed by others
References
Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A et al (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20:557–563
Kim N, Rowe BH, Raymond G, Jen H, Colman I, Jackson SA et al (2004) Underreporting of vertebral fractures on routine chest radiography. Am J Roentgenol 182:297–300
Genant HK, Jergas M, van Kuijk C (2005) Radiological assessment of vertebral fractures. In: Radiology vertebral fracture initiative resource document (part 2). International Osteoporosis Foundation, Switzerland. Available at http://www.iofbonehealth.org/vfi/assets/resources/Resource-Document.pdf Accessed 12 May 2009
Grados F, Fechtenbaum J, Flipon E, Kolta S, Roux C, Fardellone P (2009) Radiographic methods for evaluating osteoporotic vertebral fractures. Joint Bone Spine 76:241–247
Guglielmi G, Diacinti D, van Kuijk C, Aparisi F, Krestan C, Adams JE et al (2008) Vertebral morphometry: current methods and recent advances. Eur Radiol 18:1484–1496
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semi-quantitative technique. J Bone Miner Res 8:1137–1148
Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ 3rd (1991) Classification of vertebral fractures. J Bone Miner Res 6:207–215
McCloskey EV, Spector TD, Eyres KS, Fern ED, O'Rourke N, Vasikaran S et al (1993) The assessment of vertebral deformity: a method for use in population studies and clinical trials. Osteoporos Int 3:138–147
Guglielmi G, Stoppino LP, Placentino MG, D'Errico F, Palmieri F (2009) Reproducibility of a semi-automatic method for 6-point vertebral morphometry in a multi-centre trial. Eur J Radiol 69:173–178
Guglielmi G, Palmieri F, Placentino MG, D'Errico F, Stoppino LP (2009) Assessment of osteoporotic vertebral fractures using specialized workflow software for 6-point morphometry. Eur J Radiol 70:142–148
Sanfélix-Genovés J, Reig-Molla B, Sanfélix-Gimeno G, Peiró S, Graells-Ferrer M, Vega-Martínez M, Giner V (2010) The population-based prevalence of osteoporotic vertebral fracture and densitometric osteoporosis in post-menopausal women over 50 in Valencia, Spain (the FRAVO study). Bone 47(3):610–616
Schousboe JT, Vokes T, Broy SB, Ferrar L, McKiernan F, Roux C et al (2008) Vertebral fracture assessment: the 2007 ISCD official positions. J Clin Densitom 11:92–108
Crans GG, Genant HK, Krege JH (2005) Prognostic utility of a semi-quantitative spinal deformity index. Bone 37:175–179
Schousboe JT, Debold CR (2006) Reliability and accuracy of vertebral fracture assessment with densitometry compared to radiography in clinical practice. Osteoporos Int 17:281–289
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Grados F, Roux C, de Vernejoul MC, Utard G, Sebert JL, Fardellone P (2001) Comparison of four morphometric definitions and a semi-quantitative consensus reading for assessing prevalent vertebral fractures. Osteoporos Int 12:716–722
Ferrar L, Jiang G, Barrington NA, Eastell R (2000) Identification of vertebral deformities in women: comparison of radiological assessment and quantitative morphometry using morphometric radiography and morphometric X-ray absorptiometry. J Bone Miner Res 15:575–585
Ferrar L, Jiang G, Adams J, Eastell R (2005) Identification of vertebral fractures: an update. Osteoporos Int 16:717–728
Jiang G, Eastell R, Barrington NA, Ferrar L (2004) Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 15:887–896
Ferrar L, Jiang G, Schousboe JT, DeBold CR, Eastell R (2008) Algorithm-based qualitative and semi-quantitative identification of prevalent vertebral fracture: agreement between different readers, imaging modalities, and diagnostic approaches. J Bone Miner Res 23:417–424
Jiang G, Luo J, Pollintine P, Dolan P, Adams MA, Eastell R (2010) Vertebral fractures in the elderly may not always be “osteoporotic”. Bone 47(1):111–116
Hospers IC, van der Laan JG, Zeebregts CJ, Nieboer P, Wolffenbuttel BH, Dierckx RA et al (2009) Vertebral fracture assessment in supine position: comparison by using conventional semi-quantitative radiography and visual radiography. Radiology 251:822–828
Jiang G, Ferrar L, Barrington NA, Eastell R (2007) Standardised quantitative morphometry: a modified approach for quantitative identification of prevalent vertebral deformities. Osteoporos Int 18:1411–1419
Feinstein AR, Cicchetti DV (1990) High agreement but low kappa: I. The problems of two paradoxes. J Clin Epidemiol 43:543–549
Szulc P, Munoz F, Sornay-Rendu E, Paris E, Souhami E, Zanchetta J et al (2000) Comparison of morphometric assessment of prevalent vertebral deformities in women using different reference data. Bone 27:841–846
Acknowledgments
The FRAVO Study was funded by the General Directorate for Health Organization, Evaluation and Research (Project 0018/2005) and the General Directorate for Public Health of the Ministry of Health of the Autonomous Government of Valencia and a non-conditioned research grant from Sanofi-Aventis.
Conflicts of interest
None of the sponsors played any role in the design of the study, the collection, analysis or interpretation of data, the writing of the manuscript or in the decision to submit it for publication. JSG and SP have received research grants from various pharmaceutical companies and fees for participation in scientific meetings sponsored by pharmaceutical companies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sanfélix-Genovés, J., Arana, E., Sanfélix-Gimeno, G. et al. Agreement between semi-automatic radiographic morphometry and Genant semi-quantitative method in the assessment of vertebral fractures. Osteoporos Int 23, 2129–2134 (2012). https://doi.org/10.1007/s00198-011-1819-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1819-3