Abstract
Introduction and hypothesis
Numerous analytic observational studies assess family history as a risk factor for POP and report a wide range of associations. This review aims to systematically evaluate the role of family history of POP in relation to POP risk and its recurrence.
Methods
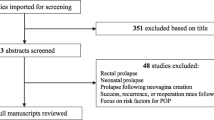
A review was performed of the PubMed/MEDLINE database with search criteria specifying family history, risk factors, POP, and their synonyms as title/abstract keywords, as well as MESH terms, up to March 2020. We aggregated evidence across studies with fixed effects (FE) and random effects (RE) meta-analysis.
Results
Forty-three articles underwent full-text review. Eighteen independent studies evaluating the relationship between family history of POP and POP risk in 3639 POP cases and 10,912 controls were eligible for meta-analysis. Four studies evaluating family history and POP recurrence in 224 recurrent cases and 400 non-recurrent cases were eligible for inclusion into another meta-analyses. A positive family history of POP is on average associated with 2.3- to 2.7-fold increased risk for POP (RE OR = 2.64; 95% CI = 2.07, 3.35) as well as a 1.4-fold increased risk for POP recurrence (FE OR = 1.44; 95% CI = 1.00, 2.08). Meta-analysis estimates of POP risk varied by study design, definition of family history, and model adjustment status. We found evidence that publication bias and recall bias are a possibility.
Conclusions
Family history of POP is a risk factor for both POP presence and recurrence. However, reported magnitudes may be overestimates due to confounding, recall bias, and publication bias.





Similar content being viewed by others
References
Weber AM, Richter HE. Pelvic organ prolapse. Obstet Gynecol. 2005;106:615–34. https://doi.org/10.1097/01.AOG.0000175832.13266.bb.
Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027–38. https://doi.org/10.1016/S0140-6736(07)60462-0.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24:1783–90. https://doi.org/10.1007/s00192-013-2169-9.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123:1201–6. https://doi.org/10.1097/AOG.0000000000000286.
Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in US women: 2010 to 2050. Obstet Gynecol. 2009;114:1278–83. https://doi.org/10.1097/AOG.0b013e3181c2ce96.
Vergeldt TFM, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26:1559–73. https://doi.org/10.1007/s00192-015-2695-8.
Giri A, Hartmann KE, Hellwege JN, Velez Edwards DR, Edwards TL. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017;217:11–26.e3. https://doi.org/10.1016/j.ajog.2017.01.039.
Lince SL, van Kempen LC, Vierhout ME, Kluivers KB. A systematic review of clinical studies on hereditary factors in pelvic organ prolapse. Int Urogynecol J. 2012;23:1327–36. https://doi.org/10.1007/s00192-012-1704-4.
Jelovsek JE, Chagin K, Gyhagen M, Hagen S, Wilson D, Kattan MW, et al. Predicting risk of pelvic floor disorders 12 and 20 years after delivery. Am J Obstet Gynecol. 2018;218:222.e1–222.e19. https://doi.org/10.1016/j.ajog.2017.10.014.
Zotero, Corporation for Digital Scholarship. Fairfax, Virginia, USA; n.d.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. https://doi.org/10.1016/j.jbi.2008.08.010.
Luchini C, Stubbs B, Solmi M, Veronese N. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa Scale. World J Meta Anal. 2017;5:80–4. https://doi.org/10.13105/wjma.v5.i4.80.
Stone J, Gurunathan U, Glass K, Munn Z, Tugwell P, Doi SAR. Stratification by quality induced selection bias in a meta-analysis of clinical trials. J Clin Epidemiol. 2019;107:51–9. https://doi.org/10.1016/j.jclinepi.2018.11.015.
Greenland S, O’rourke K. On the bias produced by quality scores in meta-analysis, and a hierarchical view of proposed solutions. Biostatistics. 2001;2:463–71. https://doi.org/10.1093/biostatistics/2.4.463.
Allen-Brady K, Norton PA, Hill AJ, Rowe K, Cannon-Albright LA. Risk of pelvic organ prolapse treatment based on extended family history. Am J Obstet Gynecol. 2020. https://doi.org/10.1016/j.ajog.2019.12.271.
Andrada Hamer M, Persson J. Familial predisposition to pelvic floor dysfunction: prolapse and incontinence surgery among family members and its relationship with age or parity in a Swedish population. Eur J Obstet Gynecol Reprod Biol. 2013;170:559–62. https://doi.org/10.1016/j.ejogrb.2013.07.025.
STATA/MP. College Station: StataCorp; n.d.
Chiaffarino F, Chatenoud L, Dindelli M, Meschia M, Buonaguidi A, Amicarelli F, et al. Reproductive factors, family history, occupation and risk of urogenital prolapse. Eur J Obstet Gynecol Reprod Biol. 1999;82:63–7.
Altman D, Zetterstrom J, Schultz I, Nordenstam J, Hjern F, Lopez A, et al. Pelvic organ prolapse and urinary incontinence in women with surgically managed rectal prolapse: a population-based case-control study. Dis Colon Rectum. 2006;49:28–35. https://doi.org/10.1007/s10350-005-0217-3.
DeLancey JOL, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109:295–302. https://doi.org/10.1097/01.AOG.0000250901.57095.ba.
McLennan MT, Harris JK, Kariuki B, Meyer S. Family history as a risk factor for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1063–9. https://doi.org/10.1007/s00192-008-0591-1.
Rodrigues AM, Girao MJBC, da Silva IDCG, Sartori MGF, de Falco Martins K, de Aquino Castro R. COL1A1 Sp1-binding site polymorphism as a risk factor for genital prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1471–5. https://doi.org/10.1007/s00192-008-0662-3.
Forsgren C, Zetterstrom J, Lopez A, Altman D. Risk factors for vaginal vault prolapse surgery in postmenopausal hysterectomized women. Menopause. 2008;15:1115–9. https://doi.org/10.1097/gme.0b013e31817062a5.
Slieker-ten Hove MCP, Pool-Goudzwaard AL, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME. Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol. 2009;200:184.e1–7. https://doi.org/10.1016/j.ajog.2008.08.070.
Slieker-ten Hove MCP, Pool-Goudzwaard AL, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:1037–45. https://doi.org/10.1007/s00192-009-0902-1.
Miedel A, Tegerstedt G, Maehle-Schmidt M, Nyren O, Hammarstrom M. Nonobstetric risk factors for symptomatic pelvic organ prolapse. Obstet Gynecol. 2009;113:1089–97. https://doi.org/10.1097/AOG.0b013e3181a11a85.
Braekken IH, Majida M, Ellstrom Engh M, Holme IM, Bo K. Pelvic floor function is independently associated with pelvic organ prolapse. BJOG. 2009;116:1706–14. https://doi.org/10.1111/j.1471-0528.2009.02379.x.
Lukanovic A, Drazic K. Risk factors for vaginal prolapse after hysterectomy. Int J Gynaecol Obstet. 2010;110:27–30. https://doi.org/10.1016/j.ijgo.2010.01.025.
Levin PJ, Visco AG, Shah SH, Fulton RG, Wu JM. Characterizing the phenotype of advanced pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2012;18:299–302. https://doi.org/10.1097/SPV.0b013e31826a53de.
Rodriguez-Mias NL, Martinez-Franco E, Aguado J, Sanchez E, Amat-Tardiu L. Pelvic organ prolapse and stress urinary incontinence, do they share the same risk factors? Eur J Obstet Gynecol Reprod Biol. 2015;190:52–7. https://doi.org/10.1016/j.ejogrb.2015.04.015.
Mothes AR, Radosa MP, Altendorf-Hofmann A, Runnebaum IB. Risk index for pelvic organ prolapse based on established individual risk factors. Arch Gynecol Obstet. 2016;293:617–24. https://doi.org/10.1007/s00404-015-3863-2.
Wang H, Zhang Z-Q, Wang S-Z, Lu J-L, Wang X-L, Zhang Z-Y. Association of matrix metalloproteinase-10 polymorphisms with susceptibility to pelvic organ prolapse. J Obstet Gynaecol Res. 2015;41:1972–81. https://doi.org/10.1111/jog.12809.
He K, Niu G, Gao J, Liu J-X, Qu H. MicroRNA-92 expression may be associated with reduced estrogen receptor beta1 mRNA levels in cervical portion of uterosacral ligaments in women with pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol. 2016;198:94–9. https://doi.org/10.1016/j.ejogrb.2016.01.007.
Asresie A, Admassu E, Setegn T. Determinants of pelvic organ prolapse among gynecologic patients in Bahir Dar, North West Ethiopia: a case-control study. Int J Women’s Health. 2016;8:713–9. https://doi.org/10.2147/IJWH.S122459.
Forner LB, Beckman EM, Smith MD. Symptoms of pelvic organ prolapse in women who lift heavy weights for exercise: a cross-sectional survey. Int Urogynecol J. 2019. https://doi.org/10.1007/s00192-019-04163-w.
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120:152–60. https://doi.org/10.1111/1471-0528.12020.
MacArthur C, Glazener C, Lancashire R, Herbison P, Wilson D, ProLong study group. Exclusive caesarean section delivery and subsequent urinary and faecal incontinence: a 12-year longitudinal study. BJOG. 2011;118:1001–7. https://doi.org/10.1111/j.1471-0528.2011.02964.x.
Diez-Itza I, Aizpitarte I, Becerro A. Risk factors for the recurrence of pelvic organ prolapse after vaginal surgery: a review at 5 years after surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1317–24. https://doi.org/10.1007/s00192-007-0321-0.
Jeon MJ, Chung SM, Jung HJ, Kim SK, Bai SW. Risk factors for the recurrence of pelvic organ prolapse. Gynecol Obstet Investig. 2008;66:268–73. https://doi.org/10.1159/000149851.
Weemhoff M, Vergeldt TFM, Notten K, Serroyen J, Kampschoer PHNM, Roumen FJME. Avulsion of puborectalis muscle and other risk factors for cystocele recurrence: a 2-year follow-up study. Int Urogynecol J. 2012;23:65–71. https://doi.org/10.1007/s00192-011-1524-y.
Notten KJB, Kluivers KB, Fütterer JJ, Schweitzer KJ, Stoker J, Mulder FE, et al. Translabial three-dimensional ultrasonography compared with magnetic resonance imaging in detecting Levator Ani defects. Obstet Gynecol. 2014;124:1190–7. https://doi.org/10.1097/AOG.0000000000000560.
Altman D, Forsman M, Falconer C, Lichtenstein P. Genetic influence on stress urinary incontinence and pelvic organ prolapse. Eur Urol. 2008;54:918–23. https://doi.org/10.1016/j.eururo.2007.12.004.
Ward RM, Velez Edwards DR, Edwards T, Giri A, Jerome RN, Wu JM. Genetic epidemiology of pelvic organ prolapse: a systematic review. Am J Obstet Gynecol. 2014;211:326–35. https://doi.org/10.1016/j.ajog.2014.04.006.
Allen-Brady K, Cannon-Albright L, Farnham JM, Teerlink C, Vierhout ME, van Kempen LCL, et al. Identification of six loci associated with pelvic organ prolapse using genome-wide association analysis. Obstet Gynecol. 2011;118:1345–53. https://doi.org/10.1097/AOG.0b013e318236f4b5.
Giri A, Wu JM, Ward RM, Hartmann KE, Park AJ, North KE, et al. Genetic determinants of pelvic organ prolapse among African American and Hispanic women in the women’s health initiative. PLoS ONE. 2015;10. https://doi.org/10.1371/journal.pone.0141647.
Acknowledgements
We thank Rebecca Helton for helpful comments.
Funding
Dr. Ayush Giri was a scholar of the Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) program [2K12HD043483 (PI: Katherine Hartmann)] and a recipient of the NIDDK Research Scientist Development Award [1K01DK120631-01A1] when this work was performed.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Samimi, P., Jones, S.H. & Giri, A. Family history and pelvic organ prolapse: a systematic review and meta-analysis. Int Urogynecol J 32, 759–774 (2021). https://doi.org/10.1007/s00192-020-04559-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04559-z