Abstract
Objectives
The objective was to evaluate pain and dyspareunia in women undergoing minimally invasive total hysterectomy and sacrocolpopexy (TLH + SCP) with a light-weight polypropylene mesh 1 year after surgery.
Methods
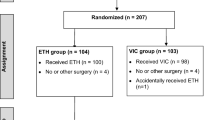
This is a planned secondary analysis of a randomized trial comparing permanent (Gore-Tex) versus absorbable suture (PDS) for vaginal attachment of a y-mesh (Upsylon™) during TLH + SCP in women with stage ≥II prolapse. Patient data were collected at baseline and 1 year after surgery. Our primary outcome was patient-reported pain or dyspareunia at 1 year.
Results
Two hundred subjects (Gore-Tex n = 99, PDS n = 101) were randomized and underwent surgery. Overall, the mean age ± SD was 60 ± 10 years, and BMI was 27 ± 5 kg/m2. The majority were white (89%), menopausal (77%), and had stage III/IV (63%) prolapse. 93% completed a 1-year follow-up and are included in this analysis (Gor-Tex n = 95, PDS n = 90). The overall rate of participants who reported pain at 1 year was 20%. Of those who did not report any pain at baseline, 23% reported de novo dyspareunia, 4% reported de novo pain, and 3% reported both at 1 year. Of participants who reported pain or dyspareunia at baseline prior to surgery, 66% reported resolution of their symptoms at 1 year. There were no differences in most characteristics, including mesh/suture exposure (7% vs 5%, p = 0.56) between patients who did and did not report any pain at 1 year. On multiple logistic regression controlling for age, baseline dyspareunia, and baseline pain, baseline dyspareunia was associated with a nearly 4-fold increased odds of reporting any pain at 1 year (OR 3.8, 95%CI 1.7–8.9).
Conclusions
The majority of women report resolution of pain 1 year following TLH + SCP with a low rate of de novo pain.
Similar content being viewed by others
References
Wu JM, Kawasaki A, Hundley AF, Dieter AA, Myers ER, Sung VW. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol. 2011;205(3):230.e1–5. https://doi.org/10.1016/j.ajog.2011.03.046.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90. https://doi.org/10.1007/s00192-013-2169-9.
Meister MR, Sutcliffe S, Badu A, Ghetti C, Lowder JL. Pelvic floor myofascial pain severity and pelvic floor disorder symptom bother: is there a correlation? Am J Obstet Gynecol. 2019;221(3):235.e1–15. https://doi.org/10.1016/j.ajog.2019.07.020.
Bradley CS. Prolapse, pain, and pelvic floor muscle dysfunction. Am J Obstet Gynecol. 2019;221(3):177–8. https://doi.org/10.1016/j.ajog.2019.07.038.
Anger JT, Mueller ER, Tarnay C, et al. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014;123(1):5–12. https://doi.org/10.1097/aog.0000000000000006.
Paraiso MF, Jelovsek JE, Frick A, Chen CC, Barber MD. Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse: a randomized controlled trial. Obstet Gynecol. 2011;118(5):1005–13. https://doi.org/10.1097/AOG.0b013e318231537c.
Kenton K, Mueller ER, Tarney C, Bresee C, Anger JT. One-year outcomes after minimally invasive sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22(5):382–4. https://doi.org/10.1097/spv.0000000000000300.
Barber MD, Brubaker L, Nygaard I, et al. Pain and activity after vaginal reconstructive surgery for pelvic organ prolapse and stress urinary incontinence. Am J Obstet Gynecol. 2019;221(3):233.e1–e16. https://doi.org/10.1016/j.ajog.2019.06.004.
Handa VL, Zyczynski HM, Brubaker L, et al. Sexual function before and after sacrocolpopexy for pelvic organ prolapse. Am J Obstet Gynecol. 2007;197(6):629.e1–6. https://doi.org/10.1016/j.ajog.2007.08.016.
Matthews CA, Geller EJ, Henley BR, et al. Permanent compared with absorbable suture for vaginal mesh fixation during total hysterectomy and sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2020;136(2):355–64. https://doi.org/10.1097/AOG.0000000000003884.
Culligan PJ, Gurshumov E, Lewis C, et al. Subjective and objective results 1 year after robotic sacrocolpopexy using a lightweight Y-mesh. Int Urogynecol J. 2014;25(6):731–5. https://doi.org/10.1007/s00192-013-2265-x.
Buechel M, Tarr ME, Walters MD. Vaginal apical pain after Sacrocolpopexy in absence of vaginal mesh erosion: a case series. Female Pelvic Med Reconstr Surg. 2016;22(1):e8–10. https://doi.org/10.1097/spv.0000000000000218.
Coolen AWM, van Oudheusden AMJ, Mol BWJ, van Eijndhoven HWF, Roovers JWR, Bongers MY. Laparoscopic sacrocolpopexy compared with open abdominal sacrocolpopexy for vault prolapse repair: a randomised controlled trial. Int Urogynecol J. 2017;28(10):1469–79. https://doi.org/10.1007/s00192-017-3296-5.
Jelovsek JE, Barber MD, Brubaker L, et al. Effect of uterosacral ligament suspension vs sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL randomized clinical trial. JAMA. 2018;319(15):1554–65. https://doi.org/10.1001/jama.2018.2827.
Author information
Authors and Affiliations
Contributions
C.E. Bretschneider: project development, manuscript writing; K. Kenton: project development, data collection, manuscript writing; E.J. Geller: data collection, manuscript writing; J.M. Wu: data collection, manuscript writing; C.A. Matthews: project development, data collection, manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
Catherine A. Matthews and Kimberly Kenton are consultants for Boston Scientific Corporation and expert witnesses for defense, Johnson & Johnson. The other authors did not report any potential conflicts of interest. “Permanent versus delayed absorbable monofilament suture for vaginal graft attachment during minimally invasive total hysterectomy and sacrocolpopexy: a randomized control trial” (PACT trial) was sponsored by Boston Scientific Corporation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bretschneider, C.E., Kenton, K., Geller, E.J. et al. Pain after permanent versus delayed absorbable monofilament suture for vaginal graft attachment during minimally invasive total hysterectomy and sacrocolpopexy. Int Urogynecol J 31, 2035–2041 (2020). https://doi.org/10.1007/s00192-020-04471-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04471-6