Abstract
Introduction and hypothesis
This pilot study aimed to investigate the effectiveness of pelvic floor muscle training (PFMT) for the treatment of pelvic organ prolapse.
Methods
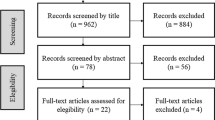
Thirty-seven women with stage II prolapse were randomized to either the intervention group (n = 21) or the control group (n = 16). The evaluation included assessments of pelvic floor muscle function and surface electromyography at baseline and post 14 weeks of treatment. The severity of prolapse was quantified by the POP-Q method and symptoms by P-QoL questionnaire.
Results
The intervention group showed significantly greater anatomic improvements in the anterior and posterior vaginal wall prolapses than did the control group (P < 0.001 and 0.025, respectively) and a decrease of symptoms. In addition, the intervention group had greater improvements in muscle strength (P < 0.001), endurance (P < 0.001), and electromyography parameters (P = 0.008) compared to the control group.
Conclusions
PFMT is effective in the treatment of pelvic organ prolapse.
Similar content being viewed by others
Abbreviations
- POP:
-
Pelvic organ prolapse
- PFMT:
-
Pelvic floor muscle training
- PFM:
-
Pelvic floor muscle
- RCT:
-
Randomized controlled trial
- MVC:
-
Maximal voluntary contraction
- sEMG:
-
Surface electromyography
References
Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Dietz HP (2008) The aetiology of prolapse. Int Urogynecol J 19:1323–1329. doi:10.1007/s00192-008-0695-7
Bump R, Norton P (1998) Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 25:723–46
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al (2002) The standardization of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178
Samuelsson E, Victor A, Tibblin G, Svaerdsudd K (1999) Signs of genital prolapse in a Swedish population of women 20–59 years of age and possible related factors. Am J Obstet Gynecol 180:299–305
Bo K (2006) Can pelvic floor muscle training prevent and treat pelvic organ prolapse? Acta Obstet Gynecol 85:263–268
Hay-Smith EJC, Dumoulin C (2006) Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. The Cochrane Data Base of Systematic Reviews, 1st issue. The Cochrane collaboration. Wiley, UK
Hagen S, Stark D, Cattermole D (2004) A United Kingdom-wide survey of physiotherapy practice in the treatment of pelvic organ prolapse. Physiotherapy 90:19–26
Brown C (2001) Pelvic floor re-education: a practical approach. In: Corcos J, Schick E (eds) The urinary sphincter. Marcel Decker, New York, pp 459–473
Miller JM, Ashton-Miller JA, DeLancey J (1998) A pelvic muscle precontraction can reduce cough-related urine loss in selected women with mild SUI. J Am Geriatr Soc 46:870–4
Pollock ML, Gaesser GA, Butcher JD, Despres JP, Dishman RK, Franklin BA (1998) The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc 30:975–91
Bump RC, Mattiasson A, Bø K, Brubaker LP, DeLancey JO, Klarskov P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Bo K, Fickenhagen HB (2001) Vaginal palpation of pelvic floor muscle strength: inter-test reproducibility and the comparison between palpation and vaginal squeeze pressure. Acta Obstet Gynecol Scand 80:883–7
Laycock J, Jerwood D (2001) Pelvic floor muscle assessment: the perfect scheme. Physiotherapy 87:631–642
Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S (2005) P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J 16:176–181
Oliveira MS, Tamanini JTN, Cavalcanti GA (2009) Validation of the Prolapse Quality-of-Life Questionnaire (P-QoL) in Portuguese version in Brazilian women. Int Urogynecol J. doi:10.1007/s00192-009-0934-6
Bø K (2004) Pelvic floor muscle training is effective in treatment of stress urinary incontinence, but how does it work? Int Urogynecol J Pelvic Floor Dysfunct 15:76–84
Balmforth J, Bidmead J, Cardozo L (2004) Raising the tone: a prospective observational study evaluating the effect of PFMT on bladder neck mobility and associated improvement in stress urinary incontinence. Neurourol Urodyn 23:553–554
Piya-Anant M, Therasakvichya S, Leelaphatanadit C, Techatrisak K (2003) Integrated health research program for the Thai elderly: prevalence of genital prolapse and effectiveness of pelvic floor exercise to prevent worsening of genital prolapse in elderly women. J Med Assoc Thai 86:509–515
Ghroubi S, Kharrat O, Chaari M, Ben Ayed B, Guermazi M, Elleuch MH (2008) Effect of conservative treatment in the management of low-degree urogenital prolapse. Ann Réadapt Méd Phys 51:96–102
Hagen S, Stark D, Glazener C, Sinclair L, Ramsay I (2009) A randomized controlled trial of pelvic floor muscle training for stages I and II pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 20(1):45–51
Brækken IH, Majida M, Ellström Engh M et al (2010) Can pelvic floor muscle training reverse pelvic organ prolapse and reduce prolapse symptoms? An assessor-blinded, randomized, controlled trial. Am J Obstet Gynecol 203:170.e1–7
Hall AF, Theofrastous JP, Cundiff GW et al (1996) Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol 175:1467–71
Moen MD, Noone MB, Vassallo BJ, Elser DM (2009) Pelvic floor muscle function in women presenting with pelvic floor disorders. Int Urogynecol J 20:843–846
Grape HH, Dedering A, Jonasson AF (2009) Retest reliability of surface electromyography on the pelvic floor muscles. Neurourol Urodyn. doi:10.1002/nau
De Luca CJ (1997) The use of surface electromyography in biomechanics. J Appl Biomech 13:135–63
Acknowledgments
This study was funded through the State of São Paulo Research Foundation—FAPESP, São Paulo, Brazil.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stüpp, L., Resende, A.P.M., Oliveira, E. et al. Pelvic floor muscle training for treatment of pelvic organ prolapse: an assessor-blinded randomized controlled trial. Int Urogynecol J 22, 1233–1239 (2011). https://doi.org/10.1007/s00192-011-1428-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1428-x