Abstract
Introduction and hypothesis
Despite exercise being the standard approach to diastasis recti abdominis (DRA) rehabilitation, there is no consensus on the most effective exercise routine and adjunct modalities for reducing DRA and improving functional parameters. The present study is aimed at investigating evidence for DRA rehabilitation in postpartum women, as well as knowledge gaps and areas for future research.
Methods
For this scoping review a systematic search was conducted in MEDLINE, AMED, CINAHL, Embase, ScienceDirect, Scopus, and PEDro up to November 2022. Selection criteria included studies investigating exercise therapy interventions both with and without adjunct modalities for postpartum DRA. Sample characteristics, diagnostic criteria, program design, and outcome measures were recorded. Critical appraisal of clinical trials was performed using PEDro classification.
Results
Twenty-eight studies were included: 14 clinical trials, 3 case series, and 11 observational studies. DRA exercises that focused on deep and superficial muscles, pelvic floor muscles, respiratory maneuvers, functional exercises, or alternative interventions (yoga, suspension training, hypopressive exercise) and adjunct modalities showed promising results in reducing the inter-recti distance and related dysfunction. However, there was great variability in diagnostic criteria and methods, DRA severity, time post-birth, and exercise program design.
Conclusions
Reviewed studies provide valuable insights into exercise therapy, but it is important to recognize their limitations, as variability in diagnostic criteria, sample characteristics, and exercise program design hinder the generalizability of the findings. Further high-quality research is needed to strengthen the evidence in this area and provide reliable recommendations for clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diastasis recti abdominis (DRA) is a connective tissue condition characterized by a separation of the two rectus abdominis (RA) muscles along the linea alba (LA) due to stretching and thinning. Separation is visible during an abdominal contraction, appearing either like a bulge or invagination through the midline of the anterior abdominal wall [1]. DRA primarily affects women antenatally and postpartum; prevalence varies between 66 and 100% in the final trimester of pregnancy and up to 53% within 24 h of delivery [2, 3]. Natural resolution is reported during the first 8 weeks postpartum, after which time spontaneous resolution plateaus [2, 4, 5]. However, some researchers suggest that recovery might still be ongoing at 6 months postpartum [6], and, despite limited research, DRA is found to be present in 36% of women at 12 months postnatally [2, 3, 7].
Assessment and diagnosis of DRA are performed via inter-recti distance (IRD) [5] measurement. Ultrasound and calipers are recommended as the most reliable IRD assessment methods [8, 9]. Currently, there is no consensus about cut-off points for diagnosis, although some researchers consider ultrasound measurements of 2.2–2.3 cm at the umbilicus level to be clinically important [5, 10]. Beer et al. [1], utilizing healthy nulliparous women, classified ultrasound-measured IRDs during rest with DRA if >1.5 cm at the xiphoid, >2.2 cm at 3 cm above the umbilicus, and >1.6 cm at 2 cm below the umbilicus.
The abdominal wall plays a significant role in maintaining posture, trunk and pelvic mobility and stability, adequate breathing quality, and abdominal viscera support. Stretching and thinning of the LA during gestation is a result of connective tissue laxity and mechanical strain from hormonal changes and greater intra-abdominal pressure [2, 11]. Abdominal bulging results from visceral protrusion between rectus bellies, whereas abdominal invagination results from linea alba posterior distortion. Both clinical signs, evident in DRA, can cause significant aesthetic concerns for postpartum women. Additionally, modifications in muscle pull angles may alter body mechanics and impair the ability of the abdominal muscle to generate force and the ability of the fascia to transfer loads across the midline [12]. Although there is weak evidence on the effects of DRA on trunk and pelvic dysfunctions or imbalances, some researchers claim that DRA-associated muscle changes may impair abdominal muscle strength, modify breathing patterns, and lead to low back or pelvic girdle pain, or other pelvic floor disorders [10, 13,14,15,16].
According to the latest guidelines, DRA management should be primarily conservative, and physiotherapy is the gold standard approach [17]. Surgical intervention, involving the reduction of the IRD through plication of the linea alba and anterior rectus sheath with or without a mesh, is typically reserved for severe cases where conservative treatment fails, no further reduction is achieved, or a concomitant symptomatic hernia is present [17, 18]. However, owing to surgical complications and the potential recurrence of DRA with subsequent pregnancies, a conservative approach is generally recommended for at least 6 months [17]. However, although rehabilitation focusing on various exercises, including pelvic floor muscle (PFM) exercises, transversus abdominis (TrA) exercises, hypopressive abdominal training [19,20,21,22], etc., is promising [21, 23], most studies are of low methodological quality [24] and present great heterogeneity regarding DRA severity, IRD measurement methods, cut-off points, etc., thus indicating no consensus on a standardized rehabilitation protocol [24, 25]. Given the above limitations, a scoping review was conducted to systematically map research on therapeutic exercise and adjunct modalities for DRA postpartum, with the objective of qualitatively synthesizing their findings and comparing their designs. The scoping review was aimed at addressing the following research questions:
-
1.
What are the current exercise interventions and adjunct modalities utilized for DRA rehabilitation in postpartum women?
-
2.
What is the impact of exercise therapy and adjunct modalities on IRD reduction and related functional outcomes in postpartum women with DRA?
-
3.
What are the existing knowledge gaps and limitations in the current literature on DRA rehabilitation practices for postpartum women?
Materials and Methods
This scoping review was designed according to the Joanna Briggs Institute Updated Guidelines of 2020 [26] and also follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses–Scoping Review (PRISMA-ScR) reporting guidelines [27, 28] (http://www.prisma-statement.org/Extensions/ScopingReviews). The study protocol was registered with OSF-Standard Pre-Data Collection Registration on Open Science Framework (OSF) (https://osf.io/hm2t4/?view_only=6f11dfcdf0ee4e42852081a6e49f9616). An electronic search was conducted between March and November 2022 on databases such as MEDLINE, CINAHL, Embase, ScienceDirect, Scopus, and PEDro, for studies that satisfied the inclusion criteria. Keywords were based on the Population, Concept, and Context (PCC) framework and included the terms "DRA" or "diastasis recti" or "rectus abdominis diastasis" or "recti divarication" and "postpartum women" or "parous women" and "physiotherapy" or "physical therapy" or "exercise" or "training" or "rehabilitation." Boolean logic (AND, OR, and NOT) was employed to generate combinations of search strings. The final search strategy for MEDLINE can be found in Appendix 1.
Eligibility criteria included experimental studies (randomized controlled trials [RCTs], controlled clinical trials [CCTs], case series) or observational/descriptive studies (cohorts, case–control, cross-sectional, longitudinal, prospective studies) containing the above terms, articles published in English and in full-text, without any limitations regarding publication date. Exclusion criteria were single-case studies, reviews, and clinical commentaries, studies in which none of the study groups entailed exercise interventions, observational studies restricted solely to healthy nulliparous subjects, and studies proposing finger-widths or tape measures as IRD outcomes. Results were scanned manually, and articles not complying with the above criteria were excluded.
To increase consistency, all three reviewers participating in the study selection and data extraction studied the PRISMA-ScR guidelines, agreed to the aforementioned screening and data extraction method, and reviewed the articles. Disagreements regarding study selection and data extraction were resolved by consensus and subsequent discussion amongst reviewers. Two reviewers developed a data-charting form and independently charted data, discussed results, and modified data-charting accordingly. Data were charted according to study design, and sample characteristics, interventions, and outcomes were tabulated. Summarized data are presented in Appendix 2. Data were interpreted and summarized by the three reviewers.
Critical appraisal of RCTs was attained by PEDro classification for clinical trials. The two assigned reviewers independently assessed and scored each scale’s item, considering that total PEDro scores of 0–3 are considered “poor,” 4–5 “fair,” 6–8 “good,” and 9–10 “excellent.” Disagreements between the reviewers were settled with the help of a third reviewer when necessary.
This scoping review was exempt from institutional review board approval as it did not involve primary data collection or human subjects. This study is part of a broader research project approved by the Research Ethics Committee of the University of Patras, with internal code 16192.
Results
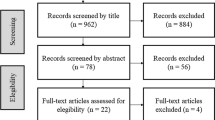
The database search identified 454 records. After removing duplicates, 330 articles were eligible for screening. Title and abstract screening removed another 255 records, leaving 75 articles for full-text review. Four reports were unavailable in full-text, and of the remaining 71, a total of 43 were excluded (Fig. 1). Finally, 28 full-text articles met the inclusion criteria: 14 clinical trials (13 RCTs, 1 CCT), 3 case series, and 11 observational/descriptive studies (cohorts, case–control, cross-sectional, longitudinal, and prospective studies).
Flow diagram demonstrating the scoping review of literature for diastasis recti abdominis rehabilitation according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [28]
The reviewed studies had varying sample sizes (3–129) and used different cut-off points for DRA diagnosis, such as 2.0 cm [29,30,31,32], 2.2 cm [12], or 2.5 cm [33,34,35,36,37] above the umbilicus during rest, and 1.5–3.0 cm above the umbilicus during a head-lift or curl-up [38,39,40]. Three studies proposed cut-offs of two finger-widths at the umbilicus [21] or anywhere in the midline [23, 41] during a head-lift and subsequently assessed with ultrasound, whereas 12 studies did not use any cut-off points [22, 37, 42,43,44,45,46,47,48,49,50,51]. Additionally, IRDs varied broadly across studies (Fig. 2). Although most samples had ultrasound-measured [12, 21,22,23, 30,31,32,33,34, 36, 37, 41, 43, 46,47,48,49,50,51] or caliper-measured [29, 35, 38,39,40, 42,43,44,45, 52] IRDs between 2.5 and 5 cm, two studies [43, 47] encompassed IRDs <2.5 cm, whereas one case series [52] included women with IRDs >7 cm. However, 7 studies [21, 23, 32, 34, 37, 45, 48] included postpartum women with combined normal and borderline IRD, according to established classification systems [1].
Range of inter-recti distance (IRD; mm) found within the participant population of each study. Notably, there is substantial variability across studies, with some including women with severe diastasis recti abdominis (DRA; IRD >50 mm) and others including women with smaller IRDs, which could be categorized as nonpathological or borderline DRA (6-22 mm). Certain studies featured a more diverse IRD range (6-50 mm), also encompassing women with moderate DRA. The bold, vertical line in the figure denotes the threshold for classifying DRA according to the criteria established by Beer et al. [1], with an IRD greater than 22 mm considered indicative of DRA
In clinical trials, the IRD was assessed under various conditions, including rest [23, 33, 37, 47, 48], head-lift [35, 38, 52], curl-up maneuver [29, 39, 40, 42,43,44], or combinations [21, 45, 46]. Observational studies also utilized combinations of rest and head-lift/curl-up maneuvers [30, 32, 49] with additional conditions, such as TrA [12, 50, 51] and PFM contractions [31, 36], sit-ups [38], leg raise or side planks [41], and abdominal hypopressive exercises (AHEs) [22]. One study [34] provided no information about the position/condition of patients during the assessment.
Time postpartum varied broadly (Fig. 3), including women who were between 6 h and 6 months postpartum [21, 23, 29, 33, 39, 40, 42, 48], less than 2 days postpartum [40, 42], less than 4 months postpartum [23, 33], between 1 week and 6 months postpartum [21, 29, 39, 48], between 2 and 8 months postpartum [34, 44, 46], over 6 months postpartum [45, 47, 52], whereas two studies [32, 43] enrolled women at 3 months to 3 years postpartum.
Range of time postpartum per study (months) for participants in each study, at the time of participant enrollment, indicating the initiation of rehabilitation. Interestingly, most of the studies included women who were within the first 6 months post-birth, a period during which a spontaneous reduction of the inter-recti distance may overlap with the intervention effect. Only three studies exclusively enrolled women who were at least 6 months postpartum, whereas for some studies the maximum time post-birth was 3 years
Exercise program duration varied in most studies between 6 and 12 weeks, except for one study [40], which applied two exercise sessions during the first 24 h postpartum (Appendix 2). Exercise frequency ranged from once [34, 35, 37, 48], twice [22, 47], or three times weekly [29, 33, 39, 42,43,44,45,46, 52]. Twelve studies utilized home exercise programs; 8 recommending daily exercise sessions [23, 32,33,34,35, 37, 42, 44], 2 [22, 43] recommending two or three times per week, and 2 [46, 47] recommending regular exercise (as often as possible), without additional specifications. Six studies [21, 29, 39, 45, 48, 52] provided no information about home exercises. Exercise progression was mentioned in 13 studies, including progression in repetitions and sets [33, 34, 40, 43, 46], exercise complexity [23, 37, 39, 45, 48], multi-parameter progression [32, 47], and 1 study [32] reported modifications according to patients’ ability and performance, without providing exercise progression details.
Quality of Included Studies
Among 14 RCTs/CCTs (Table 1), 9 were rated as good quality [21, 23, 33, 34, 39, 44,45,46,47], 4 as fair [29, 42, 43, 48], and 1 as poor [40], scoring 6–8 points, 4–5 points, and 3 points on the PEDro scale respectively. All RCTs/CCTs stated their purpose clearly, adequately described eligibility/selection criteria, and provided appropriate outcomes. Participant samples varied and in all but 2 RCTs [34, 46] sample size calculations were not provided. Case series and observational studies were charted separately.
Contribution of Individual Exercises On IRD Reduction
Abdominal Muscle Training
Abdominal muscle training was performed in 16 studies, with 10 utilizing exercises for RA muscles (crunches/curl-ups [29, 39, 43, 47], sit-ups [33, 34], and posterior pelvic tilts [33, 34, 42,43,44, 47]), and 7 [33,34,35, 40, 42,43,44] including exercises for oblique abdominals (trunk/Russian twists, twisted curl-ups, etc.; Appendix 2). Six studies included eccentric contractions [23, 33, 34, 43, 44, 47] (i.e., reverse sit-ups and reverse trunk twists). Eleven studies [21,22,23, 32, 33, 37, 39, 40, 42, 44, 47] included exercises activating TrA muscles, such as abdominal drawing-in maneuvers/static abdominal contractions. Exercise progressions included a combination of abdominal muscle control and distal extremity movements [23, 29, 32, 39, 45, 46].
Rectus Abdominis Training
Several studies (observational [22, 30, 41, 50] and case–controls [49]) observed an immediate DRA closure (above and below the umbilicus) during abdominal crunch/curl-up maneuvers [30, 51] (Fig. 4). A fair-quality RCT [43] reported statistically significant improvements in IRD closure with “traditional” curl-ups compared with plank exercises (Table 2). Another fair-quality RCT [29] found abdominal crunches to be more effective than a double straight leg raise exercise protocol for reducing IRD. In an observational study [36], a head-lift maneuver seemed to have a similar effect to a twisted curl-up exercise on IRD reduction. Djivoh and De Jaeger [38], however, observed a significant IRD decrease during curl-ups and sit-ups compared with head-lifts. DRA reduction during curl-up in women with vaginal deliveries and in those with cesarean sections was found to be similar [50].
Abdominal muscle exercises (rectus abdominis focused) A. Crunch exercise. The patient is positioned in supine with legs bent and arms supporting the head. Then they are asked to dynamically elevate their head and upper torso until their shoulder blades lift off the surface. B. Curl-up exercise. Positioned in supine with bent legs and arms extended beside the hips, parallel to the bed, the patient is instructed to curl their upper back and shoulders in a controlled way, until their shoulder blades are off the bed while maintaining their lower back in contact with the bed. The arms remain parallel to the ground, reaching towards the feet
Transversus Abdominis Training
The TrA is the main component of most DRA protocols. These contractions are guided by an abdominal drawing-in maneuver (ADIM) following deep exhalation (Fig. 5). Researchers investigating TrA contractions via ultrasound, using the ADIM on DRA patients, found an immediate IRD increase, attributed to the muscle’s transverse fibers and pull angle [31, 36, 49,50,51] (Fig. 6), and tension of the LA minimizing distortion [12]. In a good-quality RCT [21], however, TrA exercises from various positions in DRA women showed a significant IRD decrease after 12 weeks, compared with only the taping or the control group (maintaining normal activity).
Activation of the transversus abdominis (TrA) muscle. A. The patient is instructed to take a deep breath keeping the abdomen relaxed and then to fully exhale slowly. At the end of expiration, the patient is asked to perform an abdominal drawing-in maneuver (ADIM); to pull the belly button towards the spine and upwards towards the thorax. The ADIM is considered to activate the deeper abdominal muscles (transversus abdominis and internal oblique), thus stabilizing the trunk. The physiotherapist can palpate deeper abdominal muscle activation on the lower abdominal wall, just medially of the anterior superior iliac spine. As the patient gains better control of the deeper abdominal muscles, they can be instructed to self-palpate muscle activation using two fingers. They are encouraged to sustain the contraction while breathing and audibly counting up to 10 (10 seconds). In clinical practice, transversus abdominis (TrA) activation is commonly integrated with pelvic floor muscle activation, as these muscle groups demonstrate a close collaborative relationship. B. TrA activation with distal extremity movement is a progression of the TrA activation exercise. After achieving a stable TrA contraction for at least 10 seconds while breathing, the exercise can be advanced by introducing movement in either the upper or lower extremities. As the patient gains sufficient control, both upper and lower extremities can be moved simultaneously, either in a parallel or crossed manner
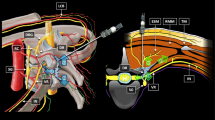
Anatomy of the abdominal wall. A. Anatomy of the abdominal wall (external oblique, internal oblique, linea alba and rectus sheath formed by the aponeuroses of the oblique and transversus abdominis muscles). Rectus abdominis muscle is also illustrated within the rectus sheath. B. cross-section of the abdominal muscles on i) upper three-quarters of the rectus sheath (above the arcuate line) where the anterior rectus sheath is formed by the aponeurosis of the external oblique and the anterior lamina of the aponeurosis of the internal oblique, while the posterior rectus sheath is formed by the posterior lamina of the aponeurosis of the internal oblique and the aponeurosis of the transversus abdominis muscle ii) lower quadrant of the rectus sheath (below the arcuate line) where the anterior rectus sheath is formed by the aponeurosis of the external oblique, the anterior and posterior lamina of the aponeurosis of the internal oblique and the aponeurosis of the transversus abdominis muscle. Adapted from Gray's Basic Anatomy, 3rd edition, Drake RL, Vogl W, Mitchell AW, Abdomen, Pages 151–152, Copyright 2023, with permission from Elsevier [License Number 5664341396354] [53].
Co-Activation of Deep and Superficial Abdominal Muscles
In observational studies, researchers observed an IRD increase with TrA pre-activation during curl-up compared with no pre-activation [12, 49,50,51]. Lee and Hodges [12] observed an IRD increase during ADIM compared with curl-up and also noted LA distortion (anteriorly or posteriorly) during curl-up, which was reduced with deep and superficial abdominal co-contractions.
Eccentric Abdominal Muscle Training
Six studies [23, 33, 34, 42, 44, 47] proposed eccentric abdominal contractions in their rehabilitation protocols. Four of them [33, 34, 42, 44] included reverse sit-ups and trunk twists, along with other concentric exercises. Α good-quality RCT [23] included a modified eccentric-based sit-up from an upright seated position, which improved muscle strength and reduced abdominal bulging. Α fair-quality RCT [42] showed an IRD decrease in the group practicing eccentric exercises, whereas other good-quality RCTs [33, 34, 44, 47] applied eccentric exercises in both intervention and control groups.
Pelvic Floor Muscle Training
Pelvic floor muscle training (Fig. 7) was applied in ten studies [22, 29, 32, 34, 39, 40, 42, 44, 45, 47]. Theodorsen et al. [31] found that both TrA and PFM increased IRDs, whereas TrA and PFM co-contracting resulted in the largest IRD increases. Gluppe et al. [36] found similar results infraumbilically. A good-quality RCT [34] applied electromyographic biofeedback-assisted pelvic floor muscle training (BAPFMT) along with abdominal exercises and neuromuscular electrical stimulation (NMES) of the RA and found decreased IRDs after 6 weeks compared with abdominal exercises and NMES only (control group).
Activation of the pelvic floor muscles (PFMs). A. The patient is lying in a relaxed supine position with the legs bent, outwardly rotated and supported at the knees. They are then instructed to take a deep breath while relaxing the abdomen and the pelvic floor muscles and then to fully exhale while they contract the PFM. The physiotherapist uses instructions like “ tighten the muscles around the vagina and anus” or “tighten the muscles around the anus as if to stop passing wind and then gently draw the anus up towards the back of the pubic bone”. Palpation of PFM activation is performed using two fingers over the labia majora, laterally to the vaginal opening. A towel is commonly utilized for patient comfort during this procedure. B. The patient is guided to self-palpate the contraction of the PFM and maintain a contraction for 10 seconds (while breathing and audibly counting to 10)
Respiratory Maneuvers/Controlled Breathing
Eight studies [21, 32,33,34, 39, 44, 45, 52] utilized a respiratory maneuver at the beginning of abdominal exercises (such as drawing-in) or PFM exercises, to facilitate TrA and PFM contractions.
Functional Exercises
Eight studies included functional exercises such as planks [32, 39, 43,44,45,46,47], side planks [23, 37, 39], bridges [32, 37, 39, 45, 47], and squats [37, 39, 47]. IRD decreased significantly across groups performing such exercises. A good-quality RCT [44] found an exercise protocol containing planks to be superior to “traditional” abdominal exercises in decreasing IRD.
Alternative Exercise Therapy Interventions
Six studies proposed alternative exercises, such as electromyographic-biofeedback PFM exercises [34], suspension training [39], yoga [48], AHEs [22, 35], and low-impact aerobic and resistance training [32]. A fair-quality RCT [48] found that a yoga exercise program significantly reduced IRD postpartum, compared with a control group practicing no exercise. A good-quality RCT [39] proposed suspension training (suspension training system [STS]) with exercises from various positions against an isometric–isotonic core stabilization protocol proposed by Litos [54] and a non-active control group. STS reduced IRD but without significant differences between exercise groups. In an observational study [22] AHEs from a supine position narrowed IRD infraumbilically but tended to increase IRD supraumbilically. In a case series [35], a protocol containing AHEs, oblique, and RA exercises was successful in significantly reducing IRD after 9 weeks.
Other Interventions/Modalities
Nine studies used special modalities or equipment in their exercise protocols, proposing abdominal binding with garments [23, 42,43,44, 46] or bandages/scarves [33, 52] during exercise. In three RCTs [42, 43, 46] abdominal binding alone [42] or combined with stabilization exercises [43, 46] effectively reduced IRD in DRA women. Thabet and Alshehri [44] found that a core stabilization-focused exercise program combined with traditional abdominal exercises and abdominal binding was more effective than traditional abdominal exercises alone in reducing IRD and improving physical function. Similar effects were described in Keshwani et al.’s RCT [23], where trunk flexion strength was clinically meaningful at 12 weeks of intervention for the abdominal binding and combination therapy (exercise and abdominal binding) groups, for women starting the program at 3 weeks postpartum. In an observational study [41], abdominal binding reduced IRD during rest, but not during contractions (curl-ups and drawing-in maneuvers). In a good-quality RCT [21] adding elastic tape to the protocol did not improve exercise results, whereas abdominal binding was more effective in supporting the abdominal wall and decreasing IRD during rest in an observational study [41]. In two good-quality RCTs [33, 34], NMES was applied to promote maximal abdominal contractions and in combination with exercise reduced IRD and proved effective.
Contribution of Rehabilitation Interventions to Other Outcome Measures
Apart from IRD reduction, DRA rehabilitation programs also decreased the waist/hip ratio and increased abdominal muscle efficiency (peak torque, maximum repetition total work, and average power) [23, 42], especially when they were combined with NMES [33] or abdominal binding [23]. In several RCTs, progressive and functional exercise programs have been shown to increase physical function [44], improve running speed for recreational runners with DRA [37], increase abdominal muscle thickness (RA, TrA, external and internal oblique), improve trunk endurance, reduce low back pain severity and disability [29], and health and functional areas of the maternal quality-of-life questionnaire [47]. PFM training using BAPFMT combined with abdominal exercises and NMES of the RA also improved physical functioning and quality of life (QoL) [34]. Progressive and functional exercise programs [32, 39] improved lumbopelvic control and proprioception impairment [39], low back pain intensity and disability [32, 39], static and dynamic balance [39], and stress urinary incontinence [32].
Discussion
Overall, based on this scoping review, there is evidence that current rehabilitation practice is beneficial in several DRA-related and functional parameters for women postpartum. However, although researchers propose various exercises and adjunct modalities, there is no agreement on what constitutes the best approach.
Evidence on Exercise Prescription
Observational studies support the notion that deep trunk muscle contractions are important in generating LA tension for supporting abdominal viscera and transferring forces across the midline of the abdomen. Researchers now agree that the ability to generate tension in the LA is crucial for abdominal wall function and is more important than complete DRA closure [12, 55, 56], whereas patient functionality, neuromuscular control, and muscle capacity to achieve force and form closure may be of greater clinical value [21]. Systematic reviews [24, 25] support encompassing TrA contractions in DRA rehabilitation programs, combined with upper and lower extremity exercises, trunk rotations, and functional training in various loading positions. Expert-based recommendations [56] report that optimal isolated and synergistic contractions of inner unit muscles and tension-free diaphragmatic breathing should be prioritized during the immediate postpartum period for DRA. Additionally, LA tension through TrA contraction is suggested to generate a connective tissue remodeling process, promoting DRA closure [23]. However, more research in this area is required.
Furthermore, a combination of deep and superficial abdominal contractions proved to be safe and effective in tensing the LA without further separating the rectus muscles [12]. Introducing trunk flexion exercises early postpartum is necessary, as most women perform RA-dominant tasks that increase abdominal pressure during daily activities and infant care. Retraining patients in generating and maintaining LA tension in static tasks with inner-unit and then combining them with outer-unit contractions in more dynamic exercises (such as trunk flexion and rotation) would be desirable. However, exercise progression should be individualized according to the patient’s needs, function, and progress. Interestingly, many protocols [29, 33,34,35, 42,43,44, 47, 52] introduce outer-unit targeting exercises (curl-ups, sit-ups, and trunk twists) early postpartum, without providing information about patients’ ability to generate tension in the LA. Moreover, in several protocols [21, 22, 29, 42, 44] no information is provided about exercise progression or adequate loading capacity. Future studies could include specific clinical/functional tests for assessing patients’ function and readiness to progress (maintain and transfer load) to more difficult exercises.
According to Dufour et al. [56] inner unit muscle retraining should also include PFM exercises, which are the gold standard approach to urinary incontinence [57] and are also proposed for DRA rehabilitation programs [58]. However, there is conflicting evidence regarding their effect on IRD [24, 34]. Observational studies [31, 36] have found PFM contractions almost as effective as TrA contractions for tensing the LA, whereas a co-contraction between them was found to be the most effective. Gluppe et al. [58], studying PFM training, found no significant differences in IRD reduction compared with control at 6 months post-intervention; however, the IRD reduction of the control group could have been due to spontaneous DRA resolution during early postpartum and not necessarily due to PFM ineffectiveness (as rehabilitation was initiated early). Nevertheless, adding electromyographic BAPFMT to abdominal exercises and NMES for RA was superior in decreasing IRD than abdominal exercises and NMES alone in an RCT [34], and it may be that muscle adaptations could be the result of sufficient PFM loading through electromyographic-biofeedback.
Various researchers have proposed eccentric abdominal contractions [23, 33, 34, 42, 44, 47]. Unfortunately, most protocols encompass eccentric exercises in both intervention and control [33, 34, 44, 47] groups; thus, no clear conclusions can be drawn. Eccentric muscle contractions are superior to concentric or isometric ones regarding muscular adaptations, such as strength [59], muscle mass [60], and structural arrangement [61] (muscle bundles’ length and pennation angles). Moreover, eccentric exercise can activate type II muscle fibers [59] and produce greater forces than concentric, resulting in easier load transfers [62]. Thus, eccentric contractions may be more suitable for the early postpartum period when abdominal muscles may be less effective at generating force. Although eccentric training has generally been extensively studied, its effect on the RA muscle or the DRA is as yet unknown. Indeed, researchers hypothesize that eccentric RA contractions might improve strength and muscle alignment, promote connective tissue remodeling, and reduce IRD [23, 47].
Several rehabilitation protocols encompass respiratory exercises, where diaphragmatic breathing or respiratory maneuvers are performed to facilitate a co-contraction of deep trunk muscles. Researchers suggest that the diaphragm contributes to spinal stability, working synergistically with TrA and PFMs to increase intra-abdominal pressure where necessary [63,64,65]. Several studies utilizing diaphragmatic exercises in patient populations and trunk dysfunctions reveal alterations in diaphragm morphology and function [66,67,68,69,70], correlations between diaphragm thickness and walking pace [71] or balance deficits [72, 73]; thus, supporting its trunk-stabilizing and functional role. Diaphragm parameters (thickness, excursion, etc.) have never been studied postpartum, and their role in DRA rehabilitation remains unknown, despite the strong recommendations for diaphragmatic rehabilitation for deeper abdominal muscle contractions [21, 32,33,34, 39, 44, 45, 52].
Alternative types of exercise, despite a scarcity of research, also appear effective. Suspension training was equally as effective as isometric–isotonic exercises for reducing IRD, improving lumbopelvic control and proprioception, static and dynamic balance, back pain, and disability [39]. Yoga was also effective in decreasing IRD in mild DRA [48]. AHEs were found to have a similar effect to a TrA contraction, increasing IRD and tensing the LA [22]. AHEs are believed to facilitate deeper abdominal and PFM contractions while reducing intra-abdominal pressure, relaxing the diaphragm, and elevating the pelvic viscera [22]. Two case series [35, 74] also reported promising results regarding IRD closure. However, it is suggested that AHEs should be prescribed with caution [75, 76] as TrA activation through AHEs may in fact increase intra-abdominal pressure, putting more strain on the PFM.
Evidence on Adjunct Modalities
Several complementary interventions and modalities have also shown encouraging effects. Combined NMES with exercise significantly reduced IRD and increased abdominal muscle strength (peak torque, maximum repetition total work, and average power) compared with exercise alone [33].
There is some evidence that abdominal binding can reduce IRD and improve muscle function. These effects, however, cannot be attributed solely to abdominal binding, as in several studies patients also performed exercise [33, 43, 44, 46], and in others, patients were only a few days/weeks postpartum [23, 42] (where spontaneous resolution usually occurs). Some researchers speculate that abdominal support garments provide protection for collagen formation during exercise and support optimal muscle position for better performance and tissue remodeling [23]. Others, however, recommend their use with caution, as they may increase intra-abdominal pressure and put a strain on PFMs [57]. Currently, there is not enough evidence to support the use of elastic tape in DRA rehabilitation. Although taping may be helpful as a proprioceptive stimulus for deep abdominal contractions during activities that increase intra-abdominal pressure [21], abdominal binding is considered superior for abdominal wall support and IRD reduction compared with taping [41]. Considering the lack of evidence, we suggest that abdominal support garments are only introduced according to individual needs (i.e., following cesarean section, poor intra-abdominal control, etc.).
Evidence on Other Outcomes
Exercise therapy was also effective in improving other outcomes and parameters. Low back pain severity and disability [29, 39], physical functioning, and QoL were improved in several studies [34, 44, 47]. Comparable results are presented in previous studies, where improvements in function, perceived pain [54], and quality of life were reported [19]. Exercise programs were also effective in improving stress urinary incontinence [32] and increasing running speed in recreational runners [37].
Exercise program efficacy seems to be independent of the rehabilitation setting. Supervised online exercise therapy was equally effective in increasing abdominal muscle thickness (RA, TrA, and obliques) and static trunk endurance as live sessions [47]. Moreover, unsupervised online therapeutic exercise (through videos) was also effective in reducing IRD, low back pain, and stress urinary incontinence [32]. However, unsupervised rehabilitation may prevent therapists’ ability to provide correcting cues and may also prevent compliance tracking.
Limitations of the Studies Included
Methodological quality was relatively moderate across studies, with 8 of them graded as borderline good quality according to PEDro [21, 23, 33, 39, 44,45,46,47], making it challenging to draw definite conclusions. Sample sizes were also relatively low across studies, whereas only 2 undertook a prior power analysis [34, 46]. There was significant variability in inclusion criteria and assessment methods, with no consensus on predefined cut-off points for DRA diagnosis and assessment conditions (resting, head-lift, or curl-up). Researchers included women with variable DRA, ranging from minimal/borderline [21, 34, 37, 43, 45, 47, 48] to mild and severe [23, 35, 39] IRD, according to established classifications [1, 3], thus potentially biasing the effectiveness of rehabilitation. The timing of exercise initiation was variable, with women enrolling immediately after birth [40] to more than 6 months or 1 year postpartum [32, 35, 37, 43]. Early rehabilitation, however, could bias results owing to the natural resolution occurring during the first months postpartum [2, 4, 5], which could perhaps justify the IRD reduction across control groups [21, 40, 48], thus limiting the credibility of the studies. Nevertheless, greater IRD reductions favoring the intervention groups could indicate that focused exercise early postpartum could further enhance this natural effect. Exercise duration and frequency were also variable among studies. Although 2020 Swedish National Guidelines [17] recommend a 6-month rehabilitation training before considering surgery, guidelines on exercise duration for DRA are not well established. According to the American College of Sports Medicine Guidelines [77], strength training for healthy individuals should include at least 2–4 sets of 8–12 repetitions per set of 60–70% of one-repetition maximum (1-RM), for at least 2–3 days per week with progressive exercise intensity over time. Postpartum PFM training protocols also suggest at least 12 weeks’ duration for optimal muscle adaptations to occur [78]. However, several studies do not follow these guidelines [33, 34, 40], and only a third of them [23, 32, 37, 39, 43,44,45,46,47,48] propose progressions of isolated muscular and functional exercises (i.e., planks, bridges, squats, etc.), which are necessary for distinct neuromuscular, functional and fascial adaptations. Also, several studies [21, 22, 29, 35, 42, 44] fail to provide information about exercise prescription, such as training load and progression. Thus, it is reasonable to assume that the inability to reach statistical significance in DRA-related outcomes in some of these studies could be the result of a low training load and/or duration.
Study Limitations
This scoping review was designed with the objective of systematically mapping rehabilitation interventions, applied to treat DRA during the postpartum period; however, it may have some limitations. In particular, the exclusion of non-English-language publications may introduce bias in study selection, whereas variability in diagnostic criteria, exercise program design, and assessment methods among the studies included may limit generalizability. Additionally, the lack of statistical comparison of results and the qualitative synthesis of findings may limit the reviewers’ ability to draw definitive conclusions. The inclusion of observational studies alongside clinical trials may further introduce biases and make it challenging to draw definitive conclusions about the long-term effectiveness of the interventions. Moreover, the review's focus on exercise interventions may overlook other potential approaches for DRA rehabilitation, such as manual therapy techniques or other adjunct therapies applied as a single treatment. The inclusion of observational studies [12, 30, 49, 51] that involve heterogeneous populations, such as pregnant and nulliparous women or men with DRA along with postpartum women, while complying with the predefined eligibility criteria (inclusion and exclusion), is a notable limitation of this scoping review. Although these studies may offer valuable insights for DRA patients from different populations, their inclusion could hinder the generalization of the results. The decision to include these studies was based on their potential contribution to the review's objectives, even though they did not exclusively focus on postpartum women with DRA. However, it is important to recognize this limitation while interpreting the outcomes of the review. Further research focusing specifically on postpartum women with DRA could help to provide more targeted and relevant evidence for clinical practice in this population. Despite these limitations, this scoping review serves as a valuable resource for understanding the current state of research on DRA rehabilitation postpartum and identifying areas for further investigation and evidence-based practice.
Implications for Research
The identified limitations in the included studies lead to important implications for future research in postpartum DRA rehabilitation. Future studies should focus on rigorous designs, adequate sample sizes, and standardized diagnostic tools and criteria to strengthen the evidence. Prioritizing functional outcomes as well as IRD reduction and adhering to muscle-strengthening principles in exercise protocols is essential. Most importantly, aligning with expert recommendations and guidelines will standardize research practices and lead to more robust evidence for clinical decision making.
Additionally, research including women over 6 months postpartum may be essential for advancing our understanding of effective DRA rehabilitation. Interestingly, access to postpartum rehabilitation services varies widely around the world. In some health care systems, women can start rehabilitation after medical clearance, often around 6 weeks postpartum, whereas in other systems, rehabilitation is not standard unless a woman reports a specific issue, leading to delayed access. However, women tend to seek help for persistent dysfunction, especially upon returning to pre-pregnancy activities, which can extend up to 6 or more months postpartum. Understanding DRA recovery beyond 6 months post-birth, a timeframe more realistic in various regions, is crucial. This perspective provides a clearer view of the true effects of exercise and adjunct interventions by eliminating the concurrent impact of spontaneous resolution, thus aiding researchers and clinicians in improving their ability to provide accurate recommendations and guidelines. Specific guidelines and clinical recommendations are vital, particularly in regions with limited access to post-birth rehabilitation. Enhancing communication and collaboration among researchers and health care professionals can expedite women's access to essential women’s health services.
Clinical Implications
This review suggests that exercise therapy, including abdominal strengthening and deep trunk stabilizer exercises, can effectively reduce IRD and improve DRA-related dysfunction postpartum. However, interventions should also be aimed at improving muscle strength and functional ability because full IRD recovery may not always occur. Proper intra-abdominal pressure management is critical, and patients should be taught to engage their deep trunk muscles during exercise and daily activities. Health care professionals should adhere to evidence-based training principles and consider incorporating various modalities such as electromyographic biofeedback, NMES, abdominal binders, or taping to optimize outcomes. Timing of rehabilitation interventions should also be considered, and individualization of rehabilitation programs based on DRA severity, individual goals, and possible coexisting dysfunctions is crucial. Further research is needed to better understand the mechanisms by which exercise may reduce IRD and delineate specific exercise prescription parameters for DRA rehabilitation.
Additionally, in this review we seek to provide insights to clinicians specializing in women's health regarding available options for the rehabilitation of DRA. Women with DRA are usually underdiagnosed, resulting in many patients being recommended by nonqualified professionals to engage in nonspecific physical exercises that may further strain the abdominal wall. Furthermore, there is a misconception that DRA is primarily a cosmetic issue, underestimating its functional impact or potential associated dysfunctions [79]. A recent study revealed that women who were concerned with their abdominal appearance post-partum are most likely to seek advice on treatment through social media [80]. Improved communication among health care professionals is crucial for providing women with access to evidence-based women's health services. Physicians involved in women’s health, obstetricians, and urogynecologists should be well-informed about evidence-based rehabilitation interventions, suggesting conservative and effective solutions, guiding women to make informed choices and avoid unnecessary invasive procedures when possible.
Conclusions
This scoping review provides valuable insights into postpartum DRA rehabilitation, suggesting that exercise therapy might be an effective approach for treating DRA and improving overall function. However, the study also sheds light on several limitations, including methodological variability, heterogeneous inclusion criteria, and lack of adherence to evidence-based exercise principles. These limitations highlight the need for more standardized and rigorous research on this topic. Additionally, further investigation is required to understand the mechanisms of IRD reduction and establish specific exercise prescription parameters. Health care professionals should consider a more holistic but still individually tailored approach to DRA reduction, including progressive functional exercises, breathing exercises with PFM training, and individualized inner- and outer-unit abdominal training. By addressing these gaps, future research can contribute to evidence-based guidelines that enhance the overall quality of care for postpartum women with DRA.
Abbreviations
- ADIM:
-
Abdominal drawing-in maneuver
- AHE(s):
-
Abdominal hypopressive exercise(s)
- BAPFMT:
-
Biofeedback-assisted pelvic floor muscle training
- DRA:
-
Diastasis recti abdominis
- IRD:
-
Inter-recti distance
- LA:
-
Linea alba
- NMES:
-
Neuromuscular electrical stimulation
- PFM(s):
-
Pelvic floor muscle(s)
- QoL:
-
Quality of life
- RA:
-
Rectus abdominis
- STS:
-
Suspension training system
- TrA:
-
Transversus abdominis
References
Beer GM, Schuster A, Seifert B, et al. The normal width of the linea alba in nulliparous women. Clin Anat. 2009;22(6):706–11. https://doi.org/10.1002/ca.20836.
Boissonnault JS, Blaschak MJ. Incidence of diastasis recti abdominis during the childbearing year. Phys Ther. 1988;68:1082–6. https://doi.org/10.1093/ptj/68.7.1082.
Candido G, Lo T, Janssen P. Risk factors for diastasis of the recti abdominis. J Assoc Chart Physiother Womens Health. 2005;97:49–54.
Hsia M, Jones S. Natural resolution of rectus abdominis diastasis. Two single case studies. Aust J Physiother. 2000;46(4):301–7. https://doi.org/10.1016/s0004-9514(14)60291-9.
Coldron Y, Stokes MJ, Newham DJ, et al. Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther. 2008;13(2):112–21. https://doi.org/10.1016/j.math.2006.10.001.
Fernandes da Mota PG, Pascoal AG, Carita AI, et al. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. 2015;20(1):200–5. https://doi.org/10.1016/j.math.2014.09.002.
Sperstad JB, Tennfjord MK, Hilde G, et al. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50(17):1092–6. https://doi.org/10.1136/bjsports-2016-096065.
Mota P, Pascoal AG, Sancho F, et al. Reliability of the inter-rectus distance measured by palpation. Comparison of palpation and ultrasound measurements. Man Ther. 2013;18(4):294–8. https://doi.org/10.1016/j.math.2012.10.013.
van de Water AT, Benjamin DR. Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): a systematic review of their measurement properties and meta-analytic reliability generalisation. Man Ther. 2016;21:41–53. https://doi.org/10.1016/j.math.2015.09.0137.
Liaw LJ, Hsu MJ, Liao CF, et al. The relationships between inter-recti distance measured by ultrasound imaging and abdominal muscle function in postpartum women: a 6-month follow-up study. J Orthop Sports Phys Ther. 2011;41(6):435–43. https://doi.org/10.2519/jospt.2011.3507.
Lo T, Candido G, Janssen P. Diastasis of recti abdominis in pregnancy: risk factors and treatment. Physiother Can. 1999;51:32–6.
Lee D, Hodges PW. Behavior of the linea alba during a curl-up task in diastasis rectus abdominis: an observational study. J Orthop Sports Phys Ther. 2016;46(7):580–9. https://doi.org/10.2519/jospt.2016.6536.
Lee DG, Lee LJ, McLaughlin L. Stability, continence and breathing: the role of fascia following pregnancy and delivery. J Bodywork Move Ther. 2008;12:333–48. https://doi.org/10.1016/j.jbmt.2008.05.003.
Hills NF, Graham RB, McLean L. Comparison of trunk muscle function between women with and without diastasis recti abdominis at 1 year postpartum. Phys Ther. 2018;98(10):891–901. https://doi.org/10.1093/ptj/pzy083.
Benjamin DR, Frawley HC, Shields N, et al. Relationship between diastasis of the rectus abdominis muscle (DRAM) and musculoskeletal dysfunctions, pain and quality of life: a systematic review. Physiotherapy. 2019;105(1):24–34. https://doi.org/10.1016/j.physio.2018.07.002.
Gluppe S, Engh ME, Bø K. Women with diastasis recti abdominis might have weaker abdominal muscles and more abdominal pain, but no higher prevalence of pelvic floor disorders, low back and pelvic girdle pain than women without diastasis recti abdominis. Physiotherapy. 2021;111:57–65. https://doi.org/10.1016/j.physio.2021.01.008.
Carlstedt A, Bringman S, Egberth M, et al. Management of diastasis of the rectus abdominis muscles: recommendations for Swedish national guidelines. Scand J Surg. 2021;110(3):452–9. https://doi.org/10.1177/1457496920961000.
Hernández-Granados P, Henriksen NA, Berrevoet F, et al. European Hernia Society guidelines on management of rectus diastasis. Br J Surg. 2021;108(10):1189–91. https://doi.org/10.1093/bjs/znab128.
Zappile-Lucis M. Quality of life measurements and physical therapy management of a female diagnosed with diastasis recti abdominis. J Womens Health Phys Ther. 2009;33(1):22. https://doi.org/10.1097/01274882-200933010-00023.
Keeler J, Albrecht M, Eberhardt LA, et al. Diastasis recti abdominis: a survey of women's health specialists for current physical therapy clinical practice for postpartum women. J Health Phys Ther. 2012;36(3):131–42. https://doi.org/10.1097/JWH.0B013E318276F35F.
Tuttle LJ, Fasching J, Keller A, et al. Noninvasive treatment of postpartum diastasis recti abdominis: a pilot study. J Womens Health Phys Ther. 2018;42(2):65–75. https://doi.org/10.1097/JWH.0000000000000101.
Arranz-Martín B, Navarro-Brazález B, Sánchez-Sánchez B, et al. The impact of hypopressive abdominal exercise on linea alba morphology women who are postpartum: a short-term cross-sectional study. Phys Ther. 2022;102(8):pzac086. https://doi.org/10.1093/ptj/pzac086.
Keshwani N, Mathur S, McLean L. The impact of exercise therapy and abdominal binding in the management of diastasis recti abdominis in the early post-partum period: a pilot randomized controlled trial. Physiother Theory Pract. 2021;37(9):1018–33. https://doi.org/10.1080/09593985.2019.1675207.
Gluppe S, Engh ME, Bø K. What is the evidence for abdominal and pelvic floor muscle training to treat diastasis recti abdominis postpartum? A systematic review with meta-analysis. Braz J Phys Ther. 2021;25(6):664−75. https://doi.org/10.1016/j.bjpt.2021.06.006.
Benjamin DR, van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014;100(1):1–8. https://doi.org/10.1016/j.physio.2013.08.005.
Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119–26. https://doi.org/10.11124/JBIES-20-00167.
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Saleem Z, Khan AA, Farooqui SI, et al. Effect of exercise on inter-recti distance and associated low back pain among post-partum females: a randomized controlled trial. J Family Reprod Health. 2021;15(3):202–9. https://doi.org/10.18502/jfrh.v15i3.7139.
Chiarello CM, McAuley JA, Hartigan EH. Immediate effect of active abdominal contraction on inter-recti distance. J Orthop Sports Phys Ther. 2016;46(3):177–83. https://doi.org/10.2519/jospt.2016.6102.
Theodorsen NM, Strand LI, Bø K. Effect of pelvic floor and transversus abdominis muscle contraction on inter-rectus distance in postpartum women: a cross-sectional experimental study. Physiotherapy. 2019;105(3):315–20. https://doi.org/10.1016/j.physio.2018.08.009.
Leopold M, Santiago K, Cheng J, et al. Efficacy of a core strengthening program for diastasis rectus abdominis in postpartum women: a prospective observational study. J Womens Health Phys Ther. 2021;45(4):147–63. https://doi.org/10.1097/JWH.0000000000000214.
Kamel DM, Yousif AM. Neuromuscular electrical stimulation and strength recovery of postnatal diastasis recti abdominis muscles. Ann Rehabil Med. 2017;41(3):465–74. https://doi.org/10.5535/arm.2017.41.3.465.
Liang P, Liang M, Shi S, et al. Rehabilitation programme including EMG-biofeedback-assisted pelvic floor muscle training for rectus diastasis after childbirth: a randomised controlled trial. Physiotherapy. 2022;117:16–21. https://doi.org/10.1016/j.physio.2022.05.001.
León SC, Cuña-Carrera ID, de la Hoz González CA, et al. Effects of an exercise program on diastasis recti in women. Int J Health Sci Res. 2019;9(10):90–9.
Gluppe SB, Engh ME, Bø K. Immediate effect of abdominal and pelvic floor muscle exercises on interrecti distance in women with diastasis recti abdominis who were parous. Phys Ther. 2020;100(8):1372–83. https://doi.org/10.1093/ptj/pzaa070.
Deering RE, Chumanov ES, Stiffler-Joachim MR, et al. Exercise program reduces inter-recti distance in female runners up to 2 years postpartum. J Womens Health Phys Ther. 2020;44(1):9–18. https://doi.org/10.1097/JWH.0000000000000157.
Djivoh YS, De Jaeger D. Acute effect of sit-up versus curl-up on the interrecti distance: a cross-sectional study in parous women. Prog Urol. 2022;32(11):776–83. https://doi.org/10.1016/j.purol.2022.07.140.
Yalfani A, Bigdeli N, Gandomi F. Comparing the effects of suspension and isometric-isotonic training on postural stability, lumbopelvic control, and proprioception in women with diastasis recti abdominis: a randomized, single-blinded, controlled trial. Physiother Theory Pract. 2023;39(12):2596−608. https://doi.org/10.1080/09593985.2022.2100300.
Pompolim G, Santos BR, Verzola IG, et al. Physiotherapy in the reduction of diastasis of the recti abdominis in immediate postpartum. Rev Pesqui Cuid Fundam Online. 2021;13:856–60. https://doi.org/10.9789/2175-5361.rpcfo.v13.9555.
Depledge J, McNair P, Ellis R. Exercises, Tubigrip and taping: can they reduce rectus abdominis diastasis measured three weeks post-partum? Musculoskelet Sci Pract. 2021;53:102381. https://doi.org/10.1016/j.msksp.2021.102381.
El-Mekawy H, Eldeeb A, El-Lythy M, et al. Effect of abdominal exercises versus abdominal supporting belt on post-partum abdominal efficiency and rectus separation. Int J Med. 2013;7(1):75–9.
Walton LM, Costa A, LaVanture D, et al. The effects of a 6 week dynamic core stability plank exercise program compared to a traditional supine core stability strengthening program on diastasis recti abdominis closure, pain, Oswestry Disability Index (ODI) and Pelvic Floor Disability Index scores (PFDI). Phys Ther Rehabil. 2016;3(1):3. https://doi.org/10.7243/2055-2386-3-3.
Thabet AA, Alshehri MA. Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: a randomised controlled trial. J Musculoskelet Neuronal Interact. 2019;19(1):62–8.
Laframboise FC, Schlaff RA, Baruth M. Postpartum exercise intervention targeting diastasis recti abdominis. Int J Exerc Sci. 2021;14(3):400–9.
Awad E, Mobark A, Zidan AA, et al. Effect of progressive prone plank exercise program on diastasis of rectus abdominis muscle in postpartum women: a randomized controlled trial. J Hum Sport Exerc. 2021;16:395–403. https://doi.org/10.14198/jhse.2021.16.Proc2.24.
Kim S, Yi D, Yim J. The effect of core exercise using online videoconferencing platform and offline-based intervention in postpartum woman with diastasis recti abdominis. Int J Environ Res Public Health. 2022;19(12):7031. https://doi.org/10.3390/ijerph19127031.
Li Q, Lei S, Liu Y, et al. Effectiveness of yoga on the interrectus distance in early postpartum women: a high-frequency ultrasound study. Biomed Res Int. 2022;2022:8908095. https://doi.org/10.1155/2022/8908095.
Pascoal A, Dionisio S, Cordeiro F, et al. Inter-rectus distance in postpartum women can be reduced by isometric contraction of the abdominal muscles: A preliminary case-control study. Physiotherapy. 2014;100:344–8. https://doi.org/10.1016/j.physio.2013.11.006.
Sancho MF, Pascoal AG, Mota P, et al. Abdominal exercises affect inter-rectus distance in postpartum women: a two dimensional ultrasound study. Physiotherapy. 2015;101(3):286–91. https://doi.org/10.1016/j.physio.2015.04.004.
Mota P, Pascoal AG, Carita AI, et al. The immediate effects on inter-rectus distance of abdominal crunch and drawing in exercises during pregnancy and the postpartum period. Orthop Sports Phys Ther. 2015;45(10):781–8. https://doi.org/10.1016/j.physio.2013.11.006.
Hanif SM. Therapeutic exercise in the reduction of diastasis recti: case reports. Pak J Med Res. 2017;56(3):104–7.
Drake RL, Vogl W, Mitchell AW. Abdomen. Gray's anatomy for students. 1st edn. Amsterdam: Elsevier Health Sciences TW. 2005. p. 250−1.
Litos K. Progressive therapeutic exercise program for successful treatment of a postpartum woman with a severe diastasis recti abdominis. J Womens Health Phys Ther. 2014;38(2):58–73. https://doi.org/10.1097/JWH.000000000000013.
Beamish N, Green N, Nieuwold E, et al. Differences in linea alba stiffness and linea alba distortion between women with and without diastasis recti abdominis: the impact of measurement site and task. J Orthop Sports Phys Ther. 2019;49(9):656–65. https://doi.org/10.2519/jospt.2019.8543.
Dufour S, Bernard SA, Murray-Davis B, et al. Establishing expert-based recommendations for the conservative management of pregnancy-related diastasis rectus abdominis: a Delphi consensus study. J Womens Health Phys Ther. 2019;43(2):1. https://doi.org/10.1097/JWH.0000000000000130.
Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or in active control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654. https://doi.org/10.1002/14651858.CD005654.pub4.
Gluppe SL, Hilde G, Tennfjord MK, et al. Effect of a postpartum training program on the prevalence of diastasis recti abdominis in postpartum primiparous women: a randomized controlled trial. Phys Ther. 2018;98(4):260–8. https://doi.org/10.1093/ptj/pzy008.
Hortobágyi T, Hill JP, Houmard JA, et al. Adaptive responses to muscle lengthening and shortening in humans. J Appl Physiol (1985). 1996;80(3):765–72. https://doi.org/10.1152/jappl.1996.80.3.765.
Roig M, O'Brien K, Kirk G, et al. The effects of eccentric versus concentric resistance training on muscle strength and mass in healthy adults: a systematic review with meta-analysis. Br J Sports Med. 2009;43(8):556–68. https://doi.org/10.1136/bjsm.2008.051417.
Ema R, Akagi R, Wakahara T, et al. Training-induced changes in architecture of human skeletal muscles: current evidence and unresolved issues. J Phys Fit Sports Med. 2016;5(1):37–46. https://doi.org/10.7600/jpfsm.5.37.
Kues JM, Mayhew TP. Concentric and eccentric force-velocity relationships during electrically induced submaximal contractions. Physiother Res Int. 1996;1(3):195–204. https://doi.org/10.1002/pri.58.
Shirley D, Hodges P, Eriksson A, et al. Spinal stiffness changes throughout the respiratory cycle. J Appl Physiol. 2003;95(4):1467–75. https://doi.org/10.1152/japplphysiol.00939.2002.
Hodges PW, Eriksson AM, Shirley D, et al. Intraabdominal pressure increases stiffness of the lumbar spine. J Biomech. 2005;38(9):1873–80. https://doi.org/10.1016/j.jbiomech.2004.08.016.
Hodges P, Kaigle Holm A, Holm S, et al. Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine (Phila Pa 1976). 2003;28(23):2594–601. https://doi.org/10.1097/01.BRS.0000096676.14323.25.
Hodges PW, Gandevia S. Activation of the human diaphragm during a repetitive postural task. J Physiol. 2000;522(1):165–75.
Hodges PW, Heijnen I, Gandevia SC. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J Physiol. 2001;537(3):999–1008. https://doi.org/10.1111/j.1469-7793.2001.00999.x.
Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther. 1997;77(2):132–42. https://doi.org/10.1093/ptj/77.2.132.
Dülger E, Bilgin S, Bulut E, et al. The effect of stabilization exercises on diaphragm muscle thickness and movement in women with low back pain. J Back Musculoskelet Rehabil. 2018;31(2):323–9. https://doi.org/10.3233/BMR-169749.
Kolář P, Šulc J, Kynčl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352–62. https://doi.org/10.2519/jospt.2012.3830.
Jiroumaru T, Wachi M, Noguchi S, et al. Is the diaphragm thickness related to gait speed in patients with hemiplegia caused by cerebrovascular accident? J Phys Ther Sci. 2021;33(6):450–4. https://doi.org/10.1589/jpts.33.450.
Oh D, Kim G, Lee W, et al. Effects of inspiratory muscle training on balance ability and abdominal muscle thickness in chronic stroke patients. J Phys Ther Sci. 2016;28(1):107–11. https://doi.org/10.1589/jpts.28.107.
Kocjan J, Gzik-Zroska B, Nowakowska K, et al. Impact of diaphragm function parameters on balance maintenance. PLoS One. 2018;13(12):e0208697. https://doi.org/10.1371/journal.pone.0208697.
Ramírez-Jiménez M, Alburquerque-Sendín F, Garrido-Castro JL, et al. Effects of hypopressive exercises on post-partum abdominal diastasis, trunk circumference, and mechanical properties of abdominopelvic tissues: a case series. Physiother Theory Pract. 2023;39(1):49–60. https://doi.org/10.1080/09593985.2021.2004630.
Bø K, Sherburn M, Allen T. Transabdominal ultrasound measurement of pelvic floor muscle activity when activated directly or via a transversus abdominis muscle contraction. Neurourol Urodyn. 2003;22:582–8. https://doi.org/10.1002/nau.10139.
Martín-Rodríguez S, Bø K. Is abdominal hypopressive technique effective in the prevention and treatment of pelvic floor dysfunction? Marketing or evidence from high-quality clinical trials? Br J Sports Med. 2019;53(2):135–6. https://doi.org/10.1136/bjsports-2017-098046.
Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59. https://doi.org/10.1249/MSS.0b013e318213fefb.
Cacciari LP, Morin M, Mayrand MH, et al. Pelvic floor morphometrical and functional changes immediately after pelvic floor muscle training and at 1-year follow-up, in older incontinent women. Neurourol Urodyn. 2021;40(1):245–55. https://doi.org/10.1002/nau.24542.
Olsson A, Kiwanuka O, Wilhelmsson S, Sandblom G, Stackelberg O. Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function and quality of life. BJS Open. 2019;3(6):750–8. https://doi.org/10.1002/bjs5.50213.
Gluppe S, Ellström Engh M, Bø K. Primiparous women's knowledge of diastasis recti abdominis, concerns about abdominal appearance, treatments, and perceived abdominal muscle strength 6−8 months postpartum. A cross sectional comparison study. BMC Womens Health. 2022;22(1):428. https://doi.org/10.1186/s12905-022-02009-0.
Acknowledgements
The publication of the article in OA mode was financially supported by HEAL-Link.
Funding
Open access funding provided by HEAL-Link Greece. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
E. Billis: project development, data analysis, manuscript editing; A. Skoura: project development, data collection or management, data analysis, manuscript writing, critical appraisal; D.T. Papanikolaou: data collection or management, data analysis; C. Tsarbou: data collection or management, data analysis; M. Tsekoura: critical appraisal, data analysis; S. Xergia: critical appraisal, data analysis; E. Kortianou: project development, data analysis, manuscript editing; I. Maroulis: project development, data analysis, manuscript editing.
Corresponding author
Ethics declarations
Consent
Written informed consent was obtained from the patient for publication of illustrations in the Electronic Supplementary Material.
Conflicts of interest
None.
Additional information
Handling Editor: Holly E. Richter
Editor in Chief: Kaven Baessler
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Protocol registration
OSF-Standard Pre-Data Collection Registration on Open Science Framework (OSF). Registration DOI: https://doi.org/10.17605/OSF.IO/9KSY6
Supplementary information
ESM 1
(DOCX 10563 kb)
Appendices
Appendix 1: search strategy and results
Search strategy PubMed (MEDLINE)
-
1.
Topic diastasis recti abdominis: "Diastasis, Muscle"[Mesh] OR ("diastasis recti"[Text Word]) OR ("rectus abdominis diastasis"[Text Word]) OR ("abdominal separation "[Text Word]) OR (DRA[Text Word]) OR (DRAM[Text Word]) OR ("diastasis recti") OR ("rectus abdominis diastasis") OR ("abdominal separation ") OR (DRA) OR (DRAM) OR ("inter-recti distance")
-
2.
Topic physiotherapy: "Exercise Therapy"[Mesh:NoExp] OR (physiotherapy[Text Word]) OR ("physical therapy"[Text Word]) OR (exercise*[Text Word]) OR (rehabilitation[Text Word]) OR ("conservative treatment"[Text Word]) OR (physiotherapy) OR ("physical therapy") OR (exercise*) OR (rehabilitation) OR ("conservative treatment") OR (physiotherap*) OR (program*) OR (training) OR (contraction*) OR ("conservative treatment")
-
3.
Topic postpartum: "Postpartum Period"[Mesh:NoExp] OR (postpartum[Text Word]) OR (parous[Text Word]) OR (postpartum[Text Word]) OR (parous[Text Word]) OR (postpartum) OR (parous)
-
4.
#1 AND #2 AND #3
Appendix 2
Table 3
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Skoura, A., Billis, E., Papanikolaou, D.T. et al. Diastasis Recti Abdominis Rehabilitation in the Postpartum Period: A Scoping Review of Current Clinical Practice. Int Urogynecol J 35, 491–520 (2024). https://doi.org/10.1007/s00192-024-05727-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-024-05727-1