Abstract
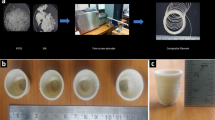
A solvent cast 3D printing (SC-3DP) technique was explored comprehensively to fabricate bioresorbable polymer matrix composite stent in the present study. The developed methodology was assessed by printing the customized shape stent on the rotating mandrel. The polymeric composite was developed by blending bioresorbable carbonyl iron powder (CIP) and polycaprolactone (PCL). The process parameter’s effect on percentage shrinkage in strut width and strut thickness, radial compression load and flexibility of stents was evaluated. Response surface methodology (RSM) was used for designing the experiments utilizing the process parameters like material compositions, printing speed and layer thickness. Analysis of variance was used to find out the significant parameters. The regression analysis was performed to obtain statistical equations with significant terms. It was noted that the reinforcement of CIP improved the fluidity of the material for better deposition as compared to pure PCL. The printing speed and layer thickness were observed to have a significant effect on the process. The significant interaction between layer thickness and printing speed parameters was also observed for shrinkage in width and thickness, compression and flexibility properties. Moreover, multi-objective optimization was performed using a genetic algorithm technique to minimize the percentage shrinkage of strut width and thickness, and load for bending to evaluate flexibility and maximize radial compression load. The method opens a unique way to fabricate patient-specific bioresorbable composite stents with customized properties.


















Similar content being viewed by others
Data availability
Not applicable
Code availability
Not applicable
References
Gao P, Wang D, Zhao Z, Cai Y, Li T, Shi H, Wu W, He W, Yin L, Huang S, Zhu F, Jiao L, Ji X, Qureshi AI, Ling F (2016) Multicenter prospective trial of stent placement in patients with symptomatic high-grade intracranial stenosis. Am J Neuroradiol 37:1275–1280. https://doi.org/10.3174/ajnr.A4698
Nikoubashman O, Heringer S, Feher K, et al (2018) Development of a polymer-based biodegradable neurovascular stent prototype: a preliminary in vitro and in vivo study. Macromol Biosci 18:1–6. https://doi.org/10.1002/mabi.201700292
Omar WA, Kumbhani DJ (2019) The current literature on bioabsorbable stents: a review. Curr Atheroscler Rep 21:1–9
Zhao D, Zhou R, Sun J, Li H, Jin Y (2019) Experimental study of polymeric stent fabrication using homemade 3D printing system. Polym Eng Sci 59:1122–1131. https://doi.org/10.1002/pen.25091
Ni L, Chen H, Luo Z, Yu Y (2020) Bioresorbable vascular stents and drug-eluting stents in treatment of coronary heart disease: a meta-analysis. J Cardiothorac Surg 15:1–7. https://doi.org/10.1186/s13019-020-1041-5
Vroman I, Tighzert L, Vroman I, Tighzert L (2009) Biodegradable polymers. Materials (Basel) 2:307–344. https://doi.org/10.3390/ma2020307
Sivalingam G, Madras G (2003) Thermal degradation of poly (ε-caprolactone). Polym Degrad Stab 80:11–16. https://doi.org/10.1016/S0141-3910(02)00376-2
Gupta KK, Kundan A, Mishra PK, Srivastava P, Mohanty S, Singh NK, Mishra A, Maiti P (2012) Polycaprolactone composites with TiO2 for potential nanobiomaterials: tunable properties using different phases. Phys Chem Chem Phys 14:12844–12853. https://doi.org/10.1039/c2cp41789h
Xu J, Zhang Y, Feng YB, Qiu T, Wang G, Liu R (2018) Electromagnetic and mechanical properties of carbonyl iron powder-filled methyl vinyl silicone rubber during thermal aging. Polym Compos 39:2897–2903. https://doi.org/10.1002/pc.24286
Teresa R, Antonio G, Vincenzo D’A et al (2010) Poly(ε-caprolactone) reinforced with sol-gel synthesized organic-inorganic hybrid fillers as composite substrates for tissue engineering. J Appl Biomater Biomech 8:146–152. https://doi.org/10.5301/JABB.2010.6094
Singh H, Sodhi GPS, Singh M, Chelliah NM, Singh H (2019) Study: wear and superhydrophobic behaviour of PTFE-ceria composite. Surf Eng 35:550–556. https://doi.org/10.1080/02670844.2018.1499176
Vella JB, Trombetta RP, Hoffman MD, Inzana J, Awad H, Benoit DSW (2018) Three dimensional printed calcium phosphate and poly(caprolactone) composites with improved mechanical properties and preserved microstructure. J Biomed Mater Res Part A 106:663–672. https://doi.org/10.1002/jbm.a.36270
Zhang J, Feng Y, Qiu T, Tang C (2014) Preparation and characterization of carbonyl iron powder/millable polyurethane elastomer microwave absorbing patch. Polym Compos 35:1318–1324. https://doi.org/10.1002/pc.22782
Liu B, Zheng YF (2011) Effects of alloying elements (Mn, Co, Al, W, Sn, B, C and S) on biodegradability and in vitro biocompatibility of pure iron. Acta Biomater 7:1407–1420. https://doi.org/10.1016/j.actbio.2010.11.001
Peuster M, Wohlsein P, Brügmann M, Ehlerding M, Seidler K, Fink C, Brauer H, Fischer A, Hausdorf G (2001) A novel approach to temporary stenting: degradable cardiovascular stents produced from corrodible metal-results 6-18 months after implantation into New Zealand white rabbits. Heart 86:563–569. https://doi.org/10.1136/heart.86.5.563
Singh J, Pandey PM, Kaur T, Singh N (2021) A comparative analysis of solvent cast 3D printed carbonyl iron powder reinforced polycaprolactone polymeric stents for intravascular applications. J Biomed Mater Res - Part B Appl Biomater 1–16. doi:https://doi.org/10.1002/jbm.b.34795
Devasthali SD, Gordeuk VR, Brittenham GM et al (1991) Bioavailability of carbonyl iron: a randomized, double-blind study. Eur J Haematol 46:272–278
Cvek M, Mrlik M, Ilcikova M, Plachy T, Sedlacik M, Mosnacek J, Pavlinek V (2015) A facile controllable coating of carbonyl iron particles with poly(glycidyl methacrylate): a tool for adjusting MR response and stability properties. J Mater Chem C 3:4646–4656. https://doi.org/10.1039/c5tc00319a
Singh J, Kaur T, Singh N, Pandey PM (2020) Biological and mechanical characterization of biodegradable carbonyl iron powder/polycaprolactone composite material fabricated using three-dimensional printing for cardiovascular stent application. Proc Inst Mech Eng Part H J Eng Med 234:975–987. https://doi.org/10.1177/0954411920936055
Guerra AJ, Ciurana J (2018) Stent’s manufacturing field: past, present, and future prospects. In: Angiography. IntechOpen, pp 1–20. https://doi.org/10.5772/intecopen.81668
Stepak B, Antończak AJ, Bartkowiak-Jowsa M et al (2014) Fabrication of a polymer-based biodegradable stent using a CO2 laser. Arch Civ Mech Eng 14:317–326. https://doi.org/10.1016/j.acme.2013.08.005
Puppi D, Pirosa A, Lupi G, Erba PA, Giachi G, Chiellini F (2017) Design and fabrication of novel polymeric biodegradable stents for small caliber blood vessels by computer-aided wet-spinning. Biomed Mater 12:12. https://doi.org/10.1088/1748-605X/aa6a28
Singh S, Singh G, Prakash C, Ramakrishna S (2020) Current status and future directions of fused filament fabrication. J Manuf Process 55:288–306. https://doi.org/10.1016/j.jmapro.2020.04.049
Singh G, Pandey PM (2020) Role of imaging data in additive manufacturing for biomedical applications. In: 3D printing in biomedical engineering. pp 69–94
van Lith R, Baker E, Ware H, Yang J, Farsheed AC, Sun C, Ameer G (2016) 3D-printing strong high-resolution antioxidant bioresorbable vascular stents. Adv Mater Technol 1:1–7. https://doi.org/10.1002/admt.201600138
Flege C, Vogt F, Höges S, Jauer L, Borinski M, Schulte VA, Hoffmann R, Poprawe R, Meiners W, Jobmann M, Wissenbach K, Blindt R (2013) Development and characterization of a coronary polylactic acid stent prototype generated by selective laser melting. J Mater Sci Mater Med 24:241–255. https://doi.org/10.1007/s10856-012-4779-z
Guerra AJ, Cano P, Rabionet M, Puig T, Ciurana J (2018) 3D-printed PCL/PLA composite stents: towards a new solution to cardiovascular problems. Materials (Basel) 11:1–13. https://doi.org/10.3390/ma11091679
Singh G, Missiaen JM, Bouvard D, Chaix JM (2021) Copper extrusion 3D printing using metal injection moulding feedstock: analysis of process parameters for green density and surface roughness optimization. Addit Manuf 38:101778. https://doi.org/10.1016/j.addma.2020.101778
Wang C, Zhang L, Fang Y, Sun W (2020) Design, characterization, and 3d printing of cardiovascular stents with zero Poisson’s ratio in longitudinal deformation. Engineering 1–12. https://doi.org/10.1016/j.eng.2020.02.013
Guo SZ, Gosselin F, Guerin N, Lanouette AM, Heuzey MC, Therriault D (2013) Solvent-cast three-dimensional printing of multifunctional microsystems. Small 9:4118–4122. https://doi.org/10.1002/smll.201300975
Singh J, Pandey PM, Kaur T, Singh N (2020) Surface characterization of polycaprolactone and carbonyl iron powder composite fabricated by solvent cast 3D printing for tissue engineering. Polym Compos 1–7. doi:https://doi.org/10.1002/pc.25871, 42, 865, 871
Qiu T, Jiang W, Yan P, Jiao L, Wang X (2020) Development of 3D-printed sulfated chitosan modified bioresorbable stents for coronary artery disease. Front Bioeng Biotechnol 8:1–12. https://doi.org/10.3389/fbioe.2020.00462
Jia H, Gu S-Y, Chang K (2018) 3D printed self-expandable vascular stents from biodegradable shape memory polymer. Adv Polym Technol 37:3222–3228. https://doi.org/10.1002/adv.22091
Xu Z, Li Z, Shi J et al (2018) 3D printing and characterization of the biodegradable vascular stent. Int J Comput Electr Eng 10:254–264. https://doi.org/10.17706/ijcee.2018.10.4.254-264
Xu C, Bouchemit A, Rance E et al Solvent-cast based metal 3D printing and secondary metallic infiltration. J Mater Chem C 5:10448. https://doi.org/10.1039/c7tc02884a
Singh J, Singh G, Pandey PM (2021) Additive manufacturing of functionalized nanomaterials for the modern health care industry. In: Additive manufacturing with functionalized nanomaterials, 1st Edition. pp 55–85
ASTM F2081 - 06(2017) Standard Guide for Characterization and Presentation of the Dimensional Attributes of Vascular Stents 1. In: ASTM Int
Cabrera MS, Oomens CWJ, Baaijens FPT (2017) Understanding the requirements of self-expandable stents for heart valve replacement: radial force, hoop force and equilibrium. J Mech Behav Biomed Mater 68:252–264. https://doi.org/10.1016/j.jmbbm.2017.02.006
Al Suwaidi J (2000) Coronary artery stents. JAMA 284:1828–1836. https://doi.org/10.1001/jama.284.14.1828
Singh G, Pandey PM (2019) Uniform and graded copper open cell ordered foams fabricated by rapid manufacturing: surface morphology, mechanical properties and energy absorption capacity. Mater Sci Eng A 761:138035. https://doi.org/10.1016/j.msea.2019.138035
Sharma P, Pandey PM (2018) Morphological and mechanical characterization of topologically ordered open cell porous iron foam fabricated using 3D printing and pressureless microwave sintering. Mater Des 160:442–454. https://doi.org/10.1016/j.matdes.2018.09.029
Singh J, Singh G, Pandey PM (2020) Electric discharge machining using rapid manufactured complex shape copper electrode with cryogenic cooling channel. Proc Inst Mech Eng Part B J Eng Manuf 1–13. doi:https://doi.org/10.1177/0954405420949102, 235, 173, 185
Kim D. B, Choi H, Joo SM et al (2013) A comparative reliability and performance study of different stent designs in terms of mechanical properties: foreshortening, recoil, radial force, and flexibility. Artif Organs 37:368–379. https://doi.org/10.1111/aor.12001
ASTM F2606 (2018) Standard guide for three-point bending of balloon expandable vascular stents. ASTM Int 08:1–6. https://doi.org/10.1520/F2606-08R14.2.1.4
Jin Y, Zhao D, Huang Y (2018) Study of extrudability and standoff distance effect during nanoclay-enabled direct printing. Bio-Design Manuf 1:123–134. https://doi.org/10.1007/s42242-018-0009-y
Guo SZ, Heuzey MC, Therriault D (2014) Properties of polylactide inks for solvent-cast printing of three-dimensional freeform microstructures. Langmuir 30:1142–1150. https://doi.org/10.1021/la4036425
Farzadi A, Solati-Hashjin M, Asadi-Eydivand M, Osman NAA (2014) Effect of layer thickness and printing orientation on mechanical properties and dimensional accuracy of 3D printed porous samples for bone tissue engineering. PLoS One 9:e108252. https://doi.org/10.1371/journal.pone.0108252
Geng P, Zhao J, Wu W, Ye W, Wang Y, Wang S, Zhang S (2019) Effects of extrusion speed and printing speed on the 3D printing stability of extruded PEEK filament. J Manuf Process 37:266–273. https://doi.org/10.1016/j.jmapro.2018.11.023
Vaezi M, Chua CK (2011) Effects of layer thickness and binder saturation level parameters on 3D printing process. Int J Adv Manuf Technol 53:275–284. https://doi.org/10.1007/s00170-010-2821-1
Christiyan KGJ, Chandrasekhar U, Venkateswarlu K (2016) A study on the influence of process parameters on the mechanical properties of 3D printed ABS composite. IOP Conf Ser Mater Sci Eng 114:012109. https://doi.org/10.1088/1757-899X/114/1/012109
Singh H, Kumar D, Singh H (2021) Development of magnesium-based hybrid metal matrix composite through in situ micro, nano reinforcements. J Compos Mater 55:109–123. https://doi.org/10.1177/0021998320946432
Pandey A, Singh G, Singh S, Jha K, Prakash C (2020) 3D printed biodegradable functional temperature-stimuli shape memory polymer for customized scaffoldings. J Mech Behav Biomed Mater 108:103781. https://doi.org/10.1016/j.jmbbm.2020.103781
Singh G, Pandey PM (2019) Rapid manufacturing of copper components using 3D printing and ultrasonic assisted pressureless sintering: experimental investigations and process optimization. J Manuf Process 43:253–269. https://doi.org/10.1016/j.jmapro.2019.05.010
Singh G, Singh S, Singh J, Pandey PM (2020) Parameters effect on electrical conductivity of copper fabricated by rapid manufacturing. Mater Manuf Process 00:1–12. https://doi.org/10.1080/10426914.2020.1784937
Berrocal DH, González GE, Fernández A, Perez S, Wilensky L, Morales C, Grinfeld L, Gelpi RJ (2008) Effects of overexpansion on stents’ recoil, symmetry/asymmetry, and neointimal hyperplasia in aortas of hypercholesterolemic rabbits. Cardiovasc Pathol 17:289–296. https://doi.org/10.1016/j.carpath.2007.10.005
Azevedo MC, Reis RL, Claase MB, Grijpma DW, Feijen J (2003) Development and properties of polycaprolactone/hydroxyapatite composite biomaterials. J Mater Sci Mater Med 14:103–107. https://doi.org/10.1023/A:1022051326282
Ahmad AF, Abbas Z, Aziz SA, Obaiys SJ, Zainuddin MF (2018) Synthesis and characterisation of nickel oxide reinforced with polycaprolactone composite for dielectric applications by controlling nickel oxide as a filler. Results Phys 11:427–435. https://doi.org/10.1016/J.RINP.2018.08.041
Ren L, Zhou X, Song Z, Zhao C, Liu Q, Xue J, Li X (2017) Process parameter optimization of extrusion-based 3D metal printing utilizing PW-LDPE-SA binder system. Materials (Basel) 10. 10. https://doi.org/10.3390/ma10030305
Ketelaars AAJ, Papantoniou Y, Nakayama K (1997) Analysis of the density and the enthalpy of poly(ϵ-caprolactone)-polycarbonate blends: amorphous phase compatibility and the effect of secondary crystallization. 921–927
Gorodkin SR, James RO, Kordonski WI (2009) Magnetic properties of carbonyl iron particles in magnetorheological fluids. J Phys Conf Ser 149:012051. https://doi.org/10.1088/1742-6596/149/1/012051
Huang B, Bártolo PJ (2018) Rheological characterization of polymer/ceramic blends for 3D printing of bone scaffolds. Polym Test 68:365–378. https://doi.org/10.1016/j.polymertesting.2018.04.033
Jin Y, Chai W, Huang Y (2017) Printability study of hydrogel solution extrusion in nanoclay yield-stress bath during printing-then-gelation biofabrication. Mater Sci Eng C 80:313–325. https://doi.org/10.1016/j.msec.2017.05.144
Ciurana J De Guerra A, Roca A, Ciurana J De (2017) A novel 3D additive manufacturing machine to biodegradable stents. Procedia Manuf 13:718–723
Lee JM, Yeong WY (2015) A preliminary model of time-pressure dispensing system for bioprinting based on printing and material parameters: this paper reports a method to predict and control the width of hydrogel filament for bioprinting applications. Virtual Phys Prototyp 10:3–8. https://doi.org/10.1080/17452759.2014.979557
Kang X B, Shen C, Qiu T, Feng Y B (2007) Study of mechanical properties of RTV silicone sealant modified by carbonyl iron powder. J Mater Sci Eng 25:99–101
Jing Q, Law JY, Tan LP, Silberschmidt VV, Li L, Dong ZL (2015) Preparation, characterization and properties of polycaprolactone diol-functionalized multi-walled carbon nanotube/thermoplastic polyurethane composite. Compos Part A Appl Sci Manuf 70:8–15. https://doi.org/10.1016/j.compositesa.2014.10.028
Haq Abdul R, Saidin M, Uzir Wahit M (2013) Improvement of mechanical properties of polycaprolactone (PCL) by addition of nano-montmorillonite (MMT) and hydroxyapatite (HA). Appl Mech Mater 315:815–819. https://doi.org/10.4028/ww.scientific.net/AMM.315.815
De Santis R, Gloria A, Russo T et al (2011) A basic approach toward the development of nanocomposite magnetic scaffolds for advanced bone tissue engineering. J Appl Polym Sci 122:3599–3605. https://doi.org/10.1002/app.34771
Uddin MS, Sidek MFR, Faizal MA, Ghomashchi R, Pramanik A (2017) Evaluating mechanical properties and failure mechanisms of fused deposition modeling acrylonitrile butadiene styrene parts. J Manuf Sci Eng Trans ASME 139:139. https://doi.org/10.1115/1.4036713
Wang P, Zou B, Ding S et al (2020) Effects of FDM-3D printing parameters on mechanical properties and microstructure of CF/PEEK and GF/PEEK. Chin J Aeronaut. https://doi.org/10.1016/j.cja.2020.05.040
Konak A, Coit DW, Smith AE (2006) Multi-objective optimization using genetic algorithms: a tutorial. Reliab Eng Syst Saf 91:992–1007. https://doi.org/10.1016/j.ress.2005.11.018
Guerra AJ, Ciurana J (2018) 3D-printed bioabsordable polycaprolactone stent: the effect of process parameters on its physical features. Mater Des 137:430–437. https://doi.org/10.1016/j.matdes.2017.10.045
Ansari M, Golzar M, Baghani M, Taghavimehr M (2020) An experimental investigation on shape memory polymer and metallic stents under bending and radial compression. Eng Res Express 2:1–9
Funding
This work was funded by the Indian Institute of Technology Delhi.
Author information
Authors and Affiliations
Contributions
Jasvinder Singh: Conceptualization, methodology, investigation, software, writing and original draft preparation. Gurminder Singh: Conceptualization, supervision, validation and writing (reviewing and editing). Pulak Mohan Pandey: Supervision, visualization and writing (reviewing and editing).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 23 kb)
Rights and permissions
About this article
Cite this article
Singh, J., Singh, G. & Pandey, P.M. Multi-objective optimization of solvent cast 3D printing process parameters for fabrication of biodegradable composite stents. Int J Adv Manuf Technol 115, 3945–3964 (2021). https://doi.org/10.1007/s00170-021-07423-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00170-021-07423-6