Abstract
Purpose
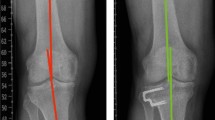
To analyze the effects of increased medial proximal tibial angle (MPTA) on the clinical outcomes and cartilage deterioration in the lateral compartment after a mean follow-up period of 4 years following open-wedge high tibial osteotomy (OWHTO) using propensity score matching (PSM) analysis.
Methods
Among 376 knees treated with OWHTO for medial unicompartmental osteoarthritis with varus deformity, 36 knees with MPTA increase of > 95° and 108 knees with MPTA increase of < 95° at the final follow-up were included. The baseline prognostic factors [age, sex, preoperative hip–knee–ankle (HKA) angle, body mass index, and preoperative knee range of motion] were equalized between the 2 groups using PSM; consequently, 31 pairs of patients were compared. The radiographic and clinical outcomes, including lateral compartment pain, were assessed. For 18 patients in each group, second-look arthroscopy and cartilage status assessment were performed.
Results
The preoperative demographics were similar between the groups. At the final follow-up, the HKA angle and joint line obliquity were significantly higher in the increased MPTA group. No significant differences were observed in the clinical outcomes between the groups. On second-look arthroscopy, significant cartilage deterioration of the lateral compartment was not observed in either group. Pain in the lateral compartment was experienced significantly more frequently in the increased MPTA group (p < 0.01).
Conclusion
Although excessively increased MPTA after HTO had no significant effects on the clinical outcomes and cartilage deterioration in the lateral compartment at the minimum 4-year follow-up, lateral compartment pain was experienced significantly more frequently in the increased MPTA group.



Similar content being viewed by others
Abbreviations
- OWHTO:
-
Open-wedge high tibial osteotomy
- OA:
-
Osteoarthritis
- MPTA:
-
Medial proximal tibial angle
- JLO:
-
Joint line obliquity
- HKA:
-
Hip–knee–ankle
- BMI:
-
Body-mass-index
- PSM:
-
Propensity score matching
- ROM:
-
Range of motion
- SD:
-
Standard deviation
- WOMAC:
-
Western Ontario and McMaster University
- HSS:
-
Hospital for Special Surgery
- ICRS:
-
International Cartilage Repair Society
- TMA:
-
Tibia mechanical angle
- VAR:
-
Varus
- NEU:
-
Neutral
- FMA:
-
Femoral mechanical angle
- VAL:
-
Valgus
- KSS:
-
Knee Society Score
- LFC:
-
Lateral femoral condyle
- LTC:
-
Lateral tibial condyle
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Score
- CONSORT:
-
Consolidated Standards of Reporting Trials
- ADL:
-
Activities of daily living
- MFC:
-
Medial femoral condyle
- MTC:
-
Medial tibial condyle
References
Akamatsu Y, Kumagai K, Kobayashi H, Tsuji M, Saito T (2018) Effect of increased coronal inclination of the tibial plateau after opening-wedge high tibial osteotomy. Arthroscopy 34:2158–2169
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21:197–205
Babis GC, An KN, Chao EY, Rand JA, Sim FH (2002) Double level osteotomy of the knee: a method to retain joint-line obliquity: clinical results. J Bone Jt Surg Am 84:1380–1388
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Jt Surg Am 85(Suppl 2):58–69
El-Azab HM, Morgenstern M, Ahrens P, Schuster T, Imhof AB, Lorenz SG (2011) Limb alignment after open-wedge high tibial osteotomy and its effect on the clinical outcome. Orthopedics 34:e622–e628
Feucht MJ, Winkler PW, Mehl J, Bode G, Forkel P, Imhoff AB, Lutz PM (2020) Isolated high tibial osteotomy is appropriate in less than two-thirds of varus knees if excessive overcorrection of the medial proximal tibial angle should be avoided. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06166-3
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am 10:585–608
Goshima K, Sawaguchi T, Sakagoshi D, Shigemoto K, Hatsuchi Y, Akahane M (2017) Age does not affect the clinical and radiological outcomes after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 25:918–923
Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Fujita K, Yamamuro Y (2019) Comparison of clinical and radiologic outcomes between normal and overcorrected medial proximal tibial angle groups after open-wedge high tibial osteotomy. Arthroscopy 35:2898–2908
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Jt Surg Am 69:332–354
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Kim CW, Seo SS, Lee CR, Gwak HC, Kim JH, Jung SG (2017) Factors affecting articular cartilage repair after open-wedge high tibial osteotomy. Knee 24:1099–1107
Kohn L, Sauerschnig M, Iskansar S, Lorenz S, Meidinger G, Imhoff AB, Hinterwimmer S (2013) Age does not influence the clinical outcome after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21:146–151
Kubota M, Kim Y, Sato T, Yamaguchi J, Ohno R, Kaneko K, Ishijima M (2020) The actual knee function was not influenced by joint line obliquity after open-wedge high tibial osteotomy. SICOT J 6:4
Lee KM, Chang CB, Park MS, Kang SB, Kim TK, Chung CY (2015) Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthr Cartil 23:232–238
Moon HS, Choi CH, Jung M, Park SH, Lee DY, Shin JC, Kim SH (2019) The effect of cartilage lesion in the lateral compartment of the knee on the surgical outcome of medial open-wedge high tibial osteotomy. J Knee Surg. https://doi.org/10.1055/s-0039-1697623
Nakayama H, Schröter S, Yamamoto C et al (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26:1873–1878
Oh KJ, Ko YB, Bae JH, Yoon ST, Kim JG (2016) Analysis of knee joint line obliquity after high tibial osteotomy. J Knee Surg 29:649–657
Sasaki E, Akimoto H, Iio K, Fujita Y, Saruga T, Kakizaki H, Ishibashi Y (2020) Long-term survival rate of closing wedge high tibial osteotomy with high valgus correction: a 15-year follow-up study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06128-9
Schuster P, Gesslein M, Schlumberger M, Mayer P, Mayr R, Oremek D, Frank S, Schulz-Jahrsdorfer M, Richter J (2018) Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med 46(6):1362–1370
Ziegler R, Goebel L, Cucchiarini M, Pape D, Madry H (2014) Effect of open wedge high tibial osteotomy on the lateral tibiofemoral compartment in sheep. Part II: standard and overcorrection do not cause articular cartilage degeneration. Knee Surg Sports Traumatol Arthrosc 22:1666–1677
Acknowledgements
No specific grant was received for this research from funding agencies in the public, commercial, or not-for-profit-sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by GWK, JKK and EKS. Review, editing and supervision by JKS.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The authors declare that there they have non-financial competing interests.
Ethical approval
This retrospective chart review study involving human participants was in accordance with the Ethical Standards of the Institutional and National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Hwasun Chonnam National University Hospital approved this study (CNUHH-2020-195).
Informed consent
Written informed consent for participation in the study was obtained from all patients, including permission to access patient’s records and publish individual clinical details.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, G.W., Kang, J.K., Song, E.K. et al. Increased joint obliquity after open-wedge high tibial osteotomy induces pain in the lateral compartment: a comparative analysis of the minimum 4-year follow-up outcomes using propensity score matching. Knee Surg Sports Traumatol Arthrosc 29, 3495–3502 (2021). https://doi.org/10.1007/s00167-020-06342-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06342-5