Abstract
Purpose
To analyze the association between change in knee joint line obliquity (KJLO) and patient-reported outcome, radiological progression of osteoarthritis, and surgical survival after lateral closing-wedge high tibial osteotomy (HTO).
Methods
A cohort of 180 patients treated in one single hospital with lateral closing-wedge HTO was examined. KJLO was defined by the medial proximal tibial angle (MPTA). To assess the association between KJLO and patient-reported outcome, radiological progression of osteoarthritis, and surgical survival, patient groups were defined: I, postoperative MPTA < 95.0°; II, postoperative MPTA ≥ 95.0°; A, MPTA change < 8.0°; B, MPTA change ≥ 8.0°. Propensity score matching was used for between-groups (I and II, A and B) covariates matching, including age, gender, preoperative lower limb alignment, preoperative medial joint space width (mJSW), preoperative Western Ontario and McMaster Universities osteoarthritis Index (WOMAC) score, wedge size, and postoperative follow-up time. Patient-reported outcome was assessed by the WOMAC questionnaire, radiological progression of osteoarthritis by mJSW and Kellgren–Lawrence (KL) grade progression (≥ 1) preoperatively and at follow-ups (> 2 years). Failure was defined as revision HTO or conversion to knee arthroplasty.
Results
After propensity score matching, groups I and II contained 58 pairs of patients and groups A and B contained 50 pairs. There were no significant differences in postoperative WOMAC score or surgical failure rate between groups I and II or between groups A and B (p > 0.05). However, the postoperative mJSW was significantly lower in group I than group II (3.2 ± 1.6 mm vs 3.9 ± 1.8 mm; p = 0.018) and in group A than group B (3.0 ± 1.7 mm vs 3.7 ± 1.5 mm; p = 0.040). KL grade progression rate was significantly higher in group I than group II (53.4% vs 29.3%; p = 0.008) and in group A than group B (56.0% vs 28.0%; p = 0.005).
Conclusion
Increased KJLO (postoperative MPTA ≥ 95.0°) or MPTA change ≥ 8.0° after lateral closing-wedge HTO does not adversely affect patient-reported outcome, radiological progression of osteoarthritis, or surgical survival at an average 5-year follow-up.
Level of evidence
III, retrospective cohort study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High tibial osteotomy (HTO) realigns the weight-bearing axis in the lower limb, providing a treatment option for medial knee osteoarthritis associated with varus alignment [31]. Two essential techniques are typically used: medial opening-wedge and lateral closing-wedge HTO [42]. However, every HTO creates a change in knee joint line obliquity (KJLO), and the medial proximal tibial angle (MPTA) can be used to describe the KJLO [11, 20, 37].
There is controversial evidence on the association between postoperative KJLO and patient-reported outcomes following medial opening-wedge HTO. Some studies suggest inferior postoperative patient-reported outcomes with an excessive postoperative KJLO [2, 20, 38], and other studies have found no significant difference in postoperative patient-reported outcomes between excessive and normal postoperative KJLO [10, 37, 40]. Additionally, limited research has explored this relationship after a lateral closing-wedge HTO.
Understanding the link between the change in KJLO and patient-reported outcome, radiological progression of osteoarthritis, and surgical survival is necessary when selecting the appropriate knee osteotomy to treat varus medial knee osteoarthritis. Some studies suggest a double-level osteotomy when a valgus-producing HTO is predicted to result in a postoperative MPTA exceeding 95° [20, 28]. However, this recommendation may not be warranted given the current controversy surrounding the association between postoperative KJLO and patient-reported outcomes. There is limited evidence on the associations between postoperative KJLO and radiological progression of osteoarthritis and surgical survival after HTO, highlighting the need for further research in this area.
The purpose of this study is to analyze the associations between change in KJLO and patient-reported outcome, radiological progression of osteoarthritis, and surgical survival after lateral closing-wedge HTO. Our hypothesis is that patients with excessive postoperative KJLO after lateral closing-wedge HTO will present poorer patient-reported outcomes and higher rates of radiological osteoarthritis progression and surgical failure compared to those with normal postoperative KJLO.
Materials and methods
Study design
A secondary analysis of patient data from another paper was conducted [13], screening 298 patients undergoing lateral closing-wedge HTO to treat symptomatic medial knee osteoarthritis with varus alignment. Patients were excluded if they (1) did not complete the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire at postoperative follow-ups (> 2 years), (2) did not have preoperative or postoperative anteroposterior long-standing radiographs, or (3) had a postoperative anteroposterior long-standing radiograph filmed, but the film time was not within 6–18 months after HTO. After applying these exclusion criteria, a total of 180 patients were included in the analyses.
This study design followed the statement of STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) for cohort studies [46] and was approved by the ethics committee of our hospital (MEC no. 2022–005).
Lateral closing-wedge HTO
The lateral closing-wedge HTO was performed by a single experienced knee surgeon (RWB), in accordance with the procedure described by Huizinga et al. [13] and van Raaij et al. [44]. The procedure involved making an incision from the tibial tuberosity to the posterior aspect of the fibular head, exposing and snaring the common peroneal nerve, resecting the anterior part of the proximal fibular head, and removing the tibial wedge using a calibrated saw guide (Allopro instrument; Zimmer, Winterthur, Switzerland). Lower limb alignment was then corrected, and the osteotomy was fixated with two staples, accompanied by an anterior compartment fasciotomy. The preoperative planning only focused on the hip–knee–ankle angle (HKA) with the goal of achieving a 4-degree valgus alignment [7]. The mechanical lateral distal femoral angle (mLDFA) and MPTA were not considered in the surgical planning for determining the osteotomy type.
Patient-reported outcome
Patient-reported outcome was evaluated by the WOMAC score including three subscales (pain, stiffness, physical function) [3]. The WOMAC is a disease-specific questionnaire, commonly used to assess pain, stiffness, and physical function in knee osteoarthritis patients and in patients after knee surgery [9, 22]. The WOMAC score was completed preoperatively and at postoperative follow-ups (> 2 years).
Radiological measurements
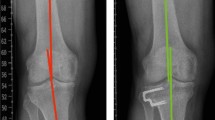
Radiological measurements are illustrated in Fig. 1. The KJLO was defined by the medial proximal tibial angle (MPTA), which is the medial angle between the line tangential to the tibial plateau surface and the tibial mechanical axis [37]. Medial joint space width (mJSW) was measured by the minimum interbone distance between the medial tibial plateau and the medial femoral condyle [39]. HKA was measured by the angle between the femoral mechanical axis and the tibial mechanical axis [6]. The mLDFA was measured by the lateral angle between the tangential line of the femoral condyles and the femoral mechanical axis [32]. Joint line convergence angle (JLCA) was measured by the angle between the tangential line of the femoral condyles and the tangential line of the tibial plateau [32]. Wedge size was obtained by targeting the lower limb mechanical axis at one-third of the lateral knee compartment (4° valgus HKA). The Kellgren and Lawrence (KL) classification was used to grade knee osteoarthritis severity, with four ordinal grades: 1 (doubtful), 2 (mild), 3 (moderate), 4 (severe) [18, 23]. The mJSW and the KL grade progression (≥ 1) were used to evaluate radiological progression of medial knee osteoarthritis [8].
Anteroposterior double-leg standing radiographs were used to assess MPTA, HKA, mLDFA, JLCA, and wedge size, and anteroposterior short knee standing radiographs were used to assess mJSW and KL grade. Patients were positioned with full knee extension and patellar forward during filming. Preoperative and postoperative MPTA, preoperative and postoperative mLDFA, preoperative and postoperative JLCA, and postoperative HKA were measured (TX), and their reliabilities were assessed by two observers (TX, RWB) in 40 patient cases from that patient database, with a three-week interval. The intra-observer and the inter-observer intra-class correlation coefficients of MPTA, mLDFA, JLCA, and HKA were at least good (> 0.75) [24, 48]. Preoperative HKA and wedge size were obtained during planning of lateral closing-wedge HTO (MH). The preoperative and the postoperative mJSW and KL grade were obtained by two orthopedic surgeons who were blinded to the patient’s clinical status using paired reading and sequence-known method [13]. The picture archiving and communication system (Philips Vue, N.V.) was used for radiological measurement, with a minimal determination of 0.01° angle and 0.1 mm distance.
Surgical failure
Surgical failure was defined as the need for revision HTO or conversion to knee arthroplasty by the time of postoperative follow-up.
Patient grouping and propensity score matching
Included patients were categorized into two groups based on MPTA cut-off points of postoperative 95° and change of 8°, respectively. These cut-off points were determined from previous biomechanical research, indicating significant shear stress increase and contact stress redistribution beyond these values [28, 47]. Group I: postoperative MPTA < 95.0°; II: postoperative MPTA ≥ 95.0°. Group A: MPTA change < 8.0°; B: MPTA change ≥ 8.0°. The propensity score matching (PSM) method was used to match the covariates between groups I and II and between groups A and B. The present study defined covariates as patient age at surgery, gender, preoperative HKA, preoperative mJSW, preoperative WOMAC (pain, stiffness, and physical function subscores, and total score), wedge size, and postoperative follow-up time [12, 17, 43, 45].
Sample size calculation
The minimal clinically important difference of WOMAC (a total score difference of 16.1 points) was used to calculate the required sample size [22]. Forty-four patients were needed in each patient group to obtain an effect size of 0.80, an alpha of 0.05, and a power of 0.95 as determined by the Mann–Whitney U test (G*Power software version 3.1.9.7).
Statistical analysis
SPSS software (version 25) was used for statistical analysis. Distribution of continuous data was checked using the Shapiro–Wilk test and Q–Q plot. PSM was performed with a match tolerance of 0.02. Pearson chi-square tests were used for between-groups comparison of gender and KL grade progression (≥ 1). Fisher’s exact test was used for between-groups comparison of surgical failure rates. Independent t-tests were used for between-groups comparison of parametric continuous data (preoperative and postoperative mJSW, and mJSW change), and Mann–Whitney U tests for between-group comparison of non-parametric continuous data (age at surgery, preoperative and postoperative HKA, preoperative and postoperative MPTA, MPTA change, preoperative and postoperative mLDFA, preoperative and postoperative JLCA, preoperative and postoperative WOMAC scores, wedge size, and postoperative follow-up time) and ordinal data (preoperative and postoperative KL grade). The WOMAC score was transformed to a 0–100-point scale where 0 indicates the best possible outcome. A p < 0.05 was considered statistically significant.
Results
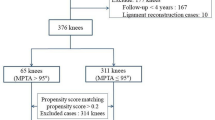
Patient selection process is depicted in Fig. 2. The baseline characteristic of included patients is presented in Table 1. Of the 180 patients included, postoperative MPTA ranges from 86.1° to 103.1° and MPTA change ranges from 1.4° to 15.3°.
After PSM, 58 pairs of patients were in groups I (postoperative MPTA < 95.0°) and II (postoperative MPTA ≥ 95.0°), and 50 pairs were in groups A (MPTA change < 8.0°) and B (MPTA change ≥ 8.0°). The covariates were matched between groups I and II (Table 2) and between groups A and B (Table 3). Comparisons of patient-reported outcome, radiological progression of osteoarthritis, and surgical failure rate between groups I and II and between groups A and B are presented in Table 4.
There were no significant differences in postoperative WOMAC or surgical failure rate between groups I and II or between groups A and B. Postoperative mJSW was significantly lower in group I than group II, and in group A than group B. Rate of KL grade progression (≥ 1) was significantly higher in group I than group II, and in group A than group B.
Discussion
The most important finding is that an increased KJLO (postoperative MPTA ≥ 95.0°) or MPTA change ≥ 8.0° does not have a negative impact on patient-reported outcome and surgical survival after an average follow-up of 5 years. Furthermore, this increase appears to slow down radiological progression of medial knee osteoarthritis. These findings reject our hypothesis.
It was previously investigated that increased KJLO causes unfavorable biomechanical changes. A finite element analysis study reported that MPTA > 95° can result in a rapid shear stress rise at the tibial plateau surface [28]. According to the result of a 10-case cadaveric study, a significant increase of contact stress at the medial spine and lateral meniscus is observed when there is an 8° KJLO increase in lateral direction (from 1° to 9° laterally) at both 0° and 20° knee flexion [47]. However, these biomechanical changes did not negatively influence the clinical and radiological results in our patient group 5 years after lateral closing-wedge HTO. A possible explanation is that these biomechanical changes may not be the primary determinants of the clinical and radiological outcomes, and the follow-up length we used may not be long enough to fully observe the effects on these outcomes.
Besides MPTA, other angles are used to assess KJLO, such as joint line orientation angles and the Mikulicz joint line angle [2, 26, 37, 41]. In the present study, MPTA was used, as it is independent of factors, such as osteoarthritis grade, single-leg/double-leg standing position, and stance width during radiograph filming, making it the preferred choice over the other angles [48].
The present study demonstrates that the increased KJLO does not affect patient-reported outcome. This finding aligns with previous studies that used similar but different questionnaires with varying follow-up lengths post-HTO, finding no significant differences in outcomes when comparing patients with postoperative MPTA < 95° and > 95°: Sohn et al. [40] used WOMAC and the Knee Society Score (KSS) with 1-year follow-up; Kim GW et al. [19] used the WOMAC, KSS, and Hospital for Special Surgery knee-rating score with > 4 years of follow-up. Goshima et al. [10] used the Japanese the orthopedic association score, Oxford knee score, and Knee injury and Osteoarthritis Outcome Score (KOOS) with mean postoperative follow-up of 6.1 years; Rosso et al. [37] used the WOMAC and KSS with mean follow-up of 10 years. By contrast, other studies report inferior outcomes that surpass the minimal clinically important difference of the questionnaire when postoperative MPTA > 95°, including Akamatsu et al. [2] with KSS and KOOS at 2-year follow-up, Kim JS et al. [20] with KSS and Short-Form 36 at a mean follow-up of 5.6 years, and Schuster et al. [38] with the International Knee Document Committee subjective knee score at a mean follow-up of 10 years. The present study distinguishes itself by the use of the PSM method to match covariates one-on-one, with a consideration of various covariates that may affect patient-reported outcome measures. Moreover, these studies all investigate medial opening-wedge HTO, whereas the present study analyzes lateral closing-wedge HTO. There are biomechanical differences between postoperative medial opening-wedge and lateral closing-wedge HTOs, such as knee-loading distribution [30], which might contribute to the reported variations in postoperative patient-reported outcome measures.
Patients with increased KJLO appear to maintain the mJSW at follow-ups. It has been reported that mJSW can continuously increase up to 3 years post-HTO [21]. However, the clinical interpretation of mJSW is still under debate. Some suggest it reflects the thickness of the medial knee cartilage [4, 39] or the status of the medial meniscus [14, 16]. The mJSW narrowing is often used to evaluate medial knee osteoarthritis progression [8, 36], whereas post-HTO changes in mJSW may be linked to the weight-bearing line ratio [15, 27]. A lateral closing-wedge HTO causes lateral defect laxity due to a decrease in the height of the lateral tibial plateau. This defect laxity, along with the postoperative valgus alignment, contributes to the increased KJLO. One possible explanation for our results is that patient with a higher increase in KJLO has a more valgus postoperative HKA, along with more significant tibial bony valgisation and increased lateral defect laxity following a lateral closing-wedge HTO, which in turn results in a larger opening of the medial knee compartment. Limited evidence is published on the association between MPTA and mJSW. One study reported that 1° MPTA decrease can significantly increase the odds of mJSW narrowing by 21% in medial knee osteoarthritis patients with a 2-year follow-up [33]; another reported no significant difference in postoperative MPTA (92.7° vs 91.9°) between patients with increased mJSW and decreased mJSW (0.8 mm vs − 0.5 mm) 3 years following medial opening-wedge HTO [21]. A medial opening-wedge HTO can increase medial collateral ligament strain, potentially affecting mJSW if no release technique is used [1, 5, 34]. By contrast, a lateral closing-wedge HTO has minimal impact on the medial collateral ligament [34]. Future studies should investigate the long-term impact of increased KJLO on lateral cartilage and meniscus status post-HTO.
The absence of mJSW narrowing in patients with increased KJLO, as observed in our study, may explain their lower rate of KL grade progression in the medial knee compartment. However, it is important to note that the evaluation of KL grade and mJSW is based on radiographs, which is not an ideal imaging modality for assessing osteoarthritis progression and cartilage thickness. Hence, future studies using magnetic resonance imaging (MRI) or arthroscopy after a long-term follow-up post-HTO are warranted to confirm these findings.
Another important finding of our study is that KJLO increase does not affect surgical failure rate after HTO. Only one other study compared the rate of revision to knee arthroplasty between postoperative MPTA ≤ 95° and > 95° following medial opening-wedge HTO, finding no significant difference over an average 10-year follow-up [38]. Another study found that a postoperative MPTA ≥ 95° can help prevent recurrent varus malalignment following a valgus-producing HTO, as observed at short-term follow-up of 1 year [35]. Likewise, in the present study, surgical failure in one of the two revised patients with MPTA < 95° was due to the reoccurrence of painful varus malalignment. Future studies may explore the impact of increased KJLO on conversion to total knee arthroplasty following a failed HTO, including surgical complexity and choice of tibial component.
To achieve a targeted alignment and prevent under-correction after a valgus-producing HTO, a large postoperative KJLO may be predicted during surgical planning, but lowering it down to the normal range (MPTA, 85°–90°) can be challenging [32]. Based on the present finding, 95° MPTA may not be a strict cut-off point that indicates a double-level osteotomy, and a MPTA change > 8° post-HTO also appears tolerable. Notably, our results do not imply that the postoperative KJLO can be entirely disregarded during HTO planning, as an increase in KJLO can have other negative impacts on gait pattern and knee kinematics [25, 29].
The strength of this study lies in its contribution toward filling the knowledge gap regarding the influences of KJLO on outcomes after a lateral closing-wedge HTO. We used a reliable KJLO measurement method and utilized the PSM method to minimize the influence of unmatched covariates on comparing outcomes. Besides the postoperative KJLO, we also examined the effects of KJLO change.
As a retrospective study, limitations include insufficient assessment of the effects of increased KJLO on knee cartilage and meniscus status. Since mJSW is an indirect indicator for assessing medial knee cartilage and meniscus status, and given the controversy surrounding what it actually represents, MRI or arthroscopy would be more suitable modalities for this assessment. Also, obesity might have negative effects on outcomes and can lead to early HTO failure; however, the data of patient body mass index at surgery was incomplete and could not be used in the analyses.
Conclusions
Increased KJLO (postoperative MPTA ≥ 95.0°) or MPTA change ≥ 8.0° after lateral closing-wedge HTO does not adversely affect patient-reported outcome, radiological progression of osteoarthritis, or surgical survival at an average 5-year follow-up. The decision to choose a double-level osteotomy over HTO should not be exclusively based on a predicted increase in KJLO (postoperative MPTA ≥ 95.0°) at planning.
Data availability
The datasets generated during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- HKA:
-
Hip-knee-ankle angle
- HTO:
-
High tibial osteotomy
- JLCA:
-
Joint line convergence angle
- KJLO:
-
Knee joint line obliquity
- KL:
-
Kellgren and Lawrence
- KOOS:
-
Knee injury and Osteoarthritis Outcome Score
- KSS:
-
Knee Society Score
- mJSW:
-
Medial joint space width
- mLDFA:
-
Mechanical lateral distal femoral angle
- MPTA:
-
Medial proximal tibial angle
- PSM:
-
Propensity score matching
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
References
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23:852–861
Akamatsu Y, Kumagai K, Kobayashi H, Tsuji M, Saito T (2018) Effect of increased coronal inclination of the tibial plateau after opening-wedge high tibial osteotomy. Arthroscopy 34:2158-2169.e2152
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Buckland-Wright JC, Macfarlane DG, Lynch JA, Jasani MK, Bradshaw CR (1995) Joint space width measures cartilage thickness in osteoarthritis of the knee: high resolution plain film and double contrast macroradiographic investigation. Ann Rheum Dis 54:263–268
Chernchujit B, Gajbhiye K, Wanaprasert N, Artha A (2020) Percutaneous partial outside-in release of medial collateral ligament for arthroscopic medial meniscus surgery with tight medial compartment by finding a “magic point.” Arthrosc Tech 9:e935–e940
Diao N, Yu F, Yang B, Ma L, Yin H, Guo A (2021) Association between changes in hip-knee-ankle angle and hindfoot alignment after total knee arthroplasty for varus knee osteoarthritis. BMC Musculoskelet Disord 22:610
Dugdale TW, Noyes FR, Styer D (1992) Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop Relat Res 274:248–264
Emrani PS, Katz JN, Kessler CL, Reichmann WM, Wright EA, McAlindon TE et al (2008) Joint space narrowing and Kellgren-Lawrence progression in knee osteoarthritis: an analytic literature synthesis. Osteoarthr Cartil 16:873–882
Escobar A, Quintana JM, Bilbao A, Aróstegui I, Lafuente I, Vidaurreta I (2007) Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthr Cartil 15:273–280
Goshima K, Sawaguchi T, Shigemoto K, Iwai S, Fujita K, Yamamuro Y (2019) Comparison of clinical and radiologic outcomes between normal and overcorrected medial proximal tibial angle groups after open-wedge high tibial osteotomy. Arthroscopy 35:2898-2908.e2891
Goto N, Akasaki Y, Okazaki K, Kuwashima U, Iwasaki K, Kawamura H et al (2020) The influence of post-operative knee coronal alignment parameters on long-term patient-reported outcomes after closed-wedge high tibial osteotomy. J Orthop 20:177–180
Howells NR, Salmon L, Waller A, Scanelli J, Pinczewski LA (2014) The outcome at ten years of lateral closing-wedge high tibial osteotomy: determinants of survival and functional outcome. Bone Jt J 96-B:1491–1497
Huizinga MR, Gorter J, Demmer A, Bierma-Zeinstra SMA, Brouwer RW (2017) Progression of medial compartmental osteoarthritis 2–8 years after lateral closing-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 25:3679–3686
Hunter DJ, Zhang YQ, Tu X, Lavalley M, Niu JB, Amin S et al (2006) Change in joint space width: hyaline articular cartilage loss or alteration in meniscus? Arthritis Rheum 54:2488–2495
Jeong HW, Shim SJ, Park SY, Lee YS (2023) Analysis of the determinant factor of the medial joint space width after medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-023-04818-w
Jones MH, Spindler KP (2017) Risk factors for radiographic joint space narrowing and patient reported outcomes of post-traumatic osteoarthritis after ACL reconstruction: data from the MOON cohort. J Orthop Res 35:1366–1374
Keenan OJF, Clement ND, Nutton R, Keating JF (2019) Older age and female gender are independent predictors of early conversion to total knee arthroplasty after high tibial osteotomy. Knee 26:207–212
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kim GW, Kang JK, Song EK, Seon JK (2021) Increased joint obliquity after open-wedge high tibial osteotomy induces pain in the lateral compartment: a comparative analysis of the minimum 4-year follow-up outcomes using propensity score matching. Knee Surg Sports Traumatol Arthrosc 29:3495–3502
Kim JS, Lim JK, Choi HG, Jeong HW, Park SB, Shim SJ et al (2022) Excessively increased joint-line obliquity after medial opening-wedge high tibial osteotomy is associated with inferior radiologic and clinical outcomes: what is permissible joint-line obliquity. Arthroscopy 38:1904–1915
Kim MS, Koh IJ, Choi KY, Kim BS, In Y (2022) Changes in joint space width over time and risk factors for deterioration of joint space width after medial opening-wedge high tibial osteotomy. Arch Orthop Trauma Surg 142:2513–2524
Kim MS, Koh IJ, Choi KY, Sung YG, Park DC, Lee HJ et al (2021) The minimal clinically important difference (MCID) for the WOMAC and factors related to achievement of the MCID after medial opening wedge high tibial osteotomy for knee osteoarthritis. Am J Sports Med 49:2406–2415
Kohn MD, Sassoon AA, Fernando ND (2016) Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res 474:1886–1893
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Kuriyama S, Watanabe M, Nakamura S, Nishitani K, Tanaka Y, Sekiguchi K et al (2020) Large medial proximal tibial angles cause excessively medial tibiofemoral contact forces and abnormal knee kinematics following open-wedge high tibial osteotomy. Clin Biomech (Bristol, Avon) 80:105190
Lee KM, Chang CB, Park MS, Kang SB, Kim TK, Chung CY (2015) Changes of knee joint and ankle joint orientations after high tibial osteotomy. Osteoarthr Cartil 23:232–238
Moon HS, Choi CH, Yoo JH, Jung M, Lee TH, Byun JW et al (2021) An increase in medial joint space width after medial open-wedge high tibial osteotomy is associated with an increase in the postoperative weight-bearing line ratio rather than with cartilage regeneration: comparative analysis of patients who underwent second-look arthroscopic assessment. Arthroscopy 37:657-668.e654
Nakayama H, Schröter S, Yamamoto C, Iseki T, Kanto R, Kurosaka K et al (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26:1873–1878
Niki Y, Nagura T, Nagai K, Kobayashi S, Harato K (2018) Kinematically aligned total knee arthroplasty reduces knee adduction moment more than mechanically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1629–1635
Ogden S, Mukherjee DP, Keating ME, Ogden AL, Albright JA, McCall RE (2009) Changes in load distribution in the knee after opening-wedge or closing-wedge high tibial osteotomy. J Arthroplasty 24:101–109
Ollivier B, Berger P, Depuydt C, Vandenneucker H (2021) Good long-term survival and patient-reported outcomes after high tibial osteotomy for medial compartment osteoarthritis. Knee Surg Sports Traumatol Arthrosc 29:3569–3584
Paley D (2002) Principles of deformity correction. Springer, Heidelberg. https://doi.org/10.1007/978-3-642-59373-4
Palmer JS, Jones LD, Monk AP, Nevitt M, Lynch J, Beard DJ et al (2020) Varus alignment of the proximal tibia is associated with structural progression in early to moderate varus osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 28:3279–3286
Park CH, Bae DK, Kim KI, Lee JW, Song SJ (2017) Serial changes in the joint space width and joint line convergence angle after closed-wedge high tibial osteotomy. Am J Sports Med 45:3254–3261
Pornrattanamaneewong C, Narkbunnam R, Chareancholvanich K (2012) Medial proximal tibial angle after medial opening wedge HTO: a retrospective diagnostic test study. Indian J Orthop 46:525–530
Ratzlaff C, Ashbeck EL, Guermazi A, Roemer FW, Duryea J, Kwoh CK (2018) A quantitative metric for knee osteoarthritis: reference values of joint space loss. Osteoarthritis Cartilage 26:1215–1224
Rosso F, Rossi R, Cantivalli A, Pilone C, Bonasia DE (2022) Joint line obliquity does not affect the outcomes of opening wedge high tibial osteotomy at an average 10-year follow-up. Am J Sports Med 50:461–470
Schuster P, Geßlein M, Schlumberger M, Mayer P, Mayr R, Oremek D et al (2018) Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med 46:1362–1370
Sekiya I, Sasaki S, Miura Y, Aoki H, Katano H, Okanouchi N et al (2022) Medial tibial osteophyte width strongly reflects medial meniscus extrusion distance and medial joint space width moderately reflects cartilage thickness in knee radiographs. J Magn Reson Imaging 56:824–834
Sohn S, Koh IJ, Kim MS, In Y (2022) Risk factors and preventive strategy for excessive coronal inclination of tibial plateau following medial opening-wedge high tibial osteotomy. Arch Orthop Trauma Surg 142:561–569
Song JH, Bin SI, Kim JM, Lee BS (2020) What is an acceptable limit of joint-line obliquity after medial open wedge high tibial osteotomy? Analysis based on midterm results. Am J Sports Med 48:3028–3035
Sun H, Zhou L, Li F, Duan J (2017) Comparison between closing-wedge and opening-wedge high tibial osteotomy in patients with medial knee osteoarthritis: a systematic review and meta-analysis. J Knee Surg 30:158–165
Trieb K, Grohs J, Hanslik-Schnabel B, Stulnig T, Panotopoulos J, Wanivenhaus A (2006) Age predicts outcome of high-tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 14:149–152
van Raaij TM, Brouwer RW (2015) Proximal tibial valgus osteotomy: lateral closing wedge. JBJS Essent Surg Tech 5:e26
van Wulfften Palthe AFY, Clement ND, Temmerman OPP, Burger BJ (2018) Survival and functional outcome of high tibial osteotomy for medial knee osteoarthritis: a 10–20-year cohort study. Eur J Orthop Surg Traumatol 28:1381–1389
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 147:573–577
Wang D, Willinger L, Athwal KK, Williams A, Amis AA (2021) Knee joint line obliquity causes tibiofemoral subluxation that alters contact areas and meniscal loading. Am J Sports Med 49:2351–2360
Xie T, van der Veen HC, van den Akker-Scheek I, Brouwer RW (2023) Assessment of joint line obliquity and its related frontal deformity using long-standing radiographs. J Orthop 40:57–64
Acknowledgements
We thank Astrid de Vries for her advice in the study design, as well as Jelle Gorter and Anna Demmer for their contribution in data collection.
Funding
There is no funding.
Author information
Authors and Affiliations
Contributions
RB, HV, IA, and TX contributed to the conception of this study. TX collected data, conducted the statistical analysis, and drafted the manuscript. MH provided the patient database. HV, RB, IA, and MH revised the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Committee of the Martini hospital Groningen, the Netherlands (MEC nr. 2022-005).
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xie, T., Huizinga, M.R., van den Akker-Scheek, I. et al. Joint line obliquity after lateral closing-wedge high tibial osteotomy does not adversely affect clinical and radiological outcome: a 5-year follow-up study. Knee Surg Sports Traumatol Arthrosc 31, 4851–4860 (2023). https://doi.org/10.1007/s00167-023-07532-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07532-7