Abstract
Purpose
The purpose of the present study was to evaluate the clinical and radiological 3–7 years outcomes of patients who underwent collagen meniscus implantation in stable or stabilized knees. It was the hypothesis that using the collagen meniscus (CMI) good clinical 3–7 years outcomes with low pain levels are achieved.
Methods
Thirty-nine patients (male:female = 30:9, mean age 34 ± 10 years) underwent arthroscopic CMI after subtotal medial (n = 32) or lateral meniscectomy (n = 7). A 7-mm CMI was performed due to prophylactic (n = 25) or therapeutic indication (n = 14). IKDC score, Tegner score preinjury, preoperatively and at follow-up, Lysholm score and visual analogue scale for pain and satisfaction (follow-up rate 90%) were assessed. MRI scans were analyzed according to the Genovese criteria (n = 19). Implant failure was defined as infection or mechanical failure of the device. The minimum follow-up time was 36 months (range 36–84 months).
Results
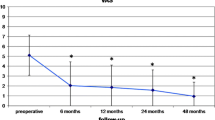
The mean VAS satisfaction preoperatively and at follow-up was 4.0 ± 0 and 1.6 ± 1.0. The mean VAS pain was 4.3 ± 3.2 preoperatively and at last follow-up 2.1 ± 1.7. The median Tegner score preinjury was 7 (range 3–10), it decreased preoperatively to median 3.5 (range 1–8) and nearly reached the preinjury level at last follow-up 6 (range 3–10). The mean Lysholm score before surgery was 66 ± 20 and 91 ± 8 at last follow-up. Seven patients (38.9%) had a normal total IKDC score (A), 10 patients were nearly normal (B) and 1 patient slightly abnormal (C). In MRI the CMI was entirely resorbed in 4 patients (21%) and partially resorbed in 15 (79%). In 4 patients (21%) the CMI was isointense, in 14 (74%) slightly hyperintense and in 1 (5%) highly hyperintense. Ten patients (53%) showed marked signs of bone marrow edema. In 13 patients (68%) an extrusion of the meniscus > 3 mm at last follow-up was found.
Conclusions
Meniscal substitution with the CMI showed good to excellent clinical 3–7 results. The CMI shows an ongoing remodelling with decreased signal intensity and decreased size. However, as meniscus extrusion remained at the same level and bone marrow edema decreased from 1 year to longer term follow-up, it appears that the remodeling comes to an end at about 5 years after CMI.
Level of evidence
IV.

Similar content being viewed by others
References
Aagaard H, Verdonk R (1999) Function of the normal meniscus and consequences of meniscal resection. Scand J Med Sci Sports 9(3):134–140
Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S (1999) Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol 54(8):502–506
Ammann N, Schiapparelli FF, Moser LB, Rasch H, Amsler F, Hirschmann MT (2018) Good correlation between bone tracer uptake in SPECT/CT and intraoperative findings of chondral lesions graded with the ICRS scoring. J Orthop Res 37(2):522–528
Bulgheroni P, Murena L, Ratti C, Bulgheroni E, Ronga M, Cherubino P (2010) Follow-up of collagen meniscus implant patients: clinical, radiological, and magnetic resonance imaging results at 5 years. Knee 17(3):224–229
Efe T, Getgood A, Schofer MD, Fuchs-Winkelmann S, Mann D, Paletta JR et al (2012) The safety and short-term efficacy of a novel polyurethane meniscal scaffold for the treatment of segmental medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc 20(9):1822–1830
Filardo G, Kon E, Perdisa F, Sessa A, Di Martino A, Busacca M et al (2017) Polyurethane-based cell-free scaffold for the treatment of painful partial meniscus loss. Knee Surg Sports Traumatol Arthrosc 25(2):459–467
Genovese E, Angeretti MG, Ronga M, Leonardi A, Novario R, Callegari L et al (2007) Follow-up of collagen meniscus implants by MRI. Radiol Med 112(7):1036–1048
Grassi A, Zaffagnini S, Marcheggiani Muccioli GM, Benzi A, Marcacci M (2014) Clinical outcomes and complications of a collagen meniscus implant: a systematic review. Int Orthop 38(9):1945–1953
Gwinner C, von Roth P, Schmidt S, Ode JE, Wulsten D, Hoburg A (2017) Biomechanical performance of a collagen meniscus implant with regard to suture material and irrigation fluid. Knee 24(4):726–732
Harston A, Nyland J, Brand E, McGinnis M, Caborn DN (2012) Collagen meniscus implantation: a systematic review including rehabilitation and return to sports activity. Knee Surg Sports Traumatol Arthrosc 20(1):135–146
Hefti F, Muller W, Jakob RP, Staubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234
Hirschmann MT, Keller L, Hirschmann A, Schenk L, Berbig R, Luthi U et al (2013) One-year clinical and MR imaging outcome after partial meniscal replacement in stabilized knees using a collagen meniscus implant. Knee Surg Sports Traumatol Arthrosc 21(3):740–747
Houck DA, Kraeutler MJ, Belk JW, McCarty EC, Bravman JT (2018) Similar clinical outcomes following collagen or polyurethane meniscal scaffold implantation: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(8):2259–2269
Monllau JC, Gelber PE, Abat F, Pelfort X, Abad R, Hinarejos P et al (2011) Outcome after partial medial meniscus substitution with the collagen meniscal implant at a minimum of 10 years' follow-up. Arthroscopy 27(7):933–943
Rodkey WG, DeHaven KE, Montgomery WH 3rd, Baker CL Jr, Beck CL Jr, Hormel SE et al (2008) Comparison of the collagen meniscus implant with partial meniscectomy. A prospective randomized trial. J Bone Jt Surg Am 90(7):1413–1426
Scotti C, Hirschmann MT, Antinolfi P, Martin I, Peretti GM (2013) Meniscus repair and regeneration: review on current methods and research potential. Eur Cells Mater 26:150–170
Schuttler KF, Haberhauer F, Gesslein M, Heyse TJ, Figiel J, Lorbach O et al (2016) Midterm follow-up after implantation of a polyurethane meniscal scaffold for segmental medial meniscus loss: maintenance of good clinical and MRI outcome. Knee Surg Sports Traumatol Arthrosc 24(5):1478–1484
Schuttler KF, Pottgen S, Getgood A, Rominger MB, Fuchs-Winkelmann S, Roessler PP et al (2015) Improvement in outcomes after implantation of a novel polyurethane meniscal scaffold for the treatment of medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc 23(7):1929–1935
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Zaffagnini S, Giordano G, Vascellari A, Bruni D, Neri MP, Iacono F et al (2007) Arthroscopic collagen meniscus implant results at 6 to 8 years follow up. Knee Surg Sports Traumatol Arthrosc 15(2):175–183
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Bonanzinga T, Nitri M, Raggi F et al (2015) MRI evaluation of a collagen meniscus implant: a systematic review. Knee Surg Sports Traumatol Arthrosc 23(11):3228–3237
Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, Bonanzinga T, Filardo G, Canales Passalacqua A et al (2011) Arthroscopic lateral collagen meniscus implant in a professional soccer player. Knee Surg Sports Traumatol Arthrosc 19(10):1740–1743
Zaffagnini S, Marcheggiani Muccioli GM, Lopomo N, Bruni D, Giordano G, Ravazzolo G et al (2011) Prospective long-term outcomes of the medial collagen meniscus implant versus partial medial meniscectomy: a minimum 10-year follow-up study. Am J Sports Med 39(5):977–985
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There was no outside funding recieved for this study.
Ethical approval
All investigations were conducted in conformity with ethical principles of research and that institutional approval of the human protocol for this investigation was obtained.
Informed consent
Informed consent for participation in the study was obtained by the local institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schenk, L., Bethge, L., Hirschmann, A. et al. Ongoing MRI remodeling 3–7 years after collagen meniscus implantation in stable knees. Knee Surg Sports Traumatol Arthrosc 28, 1099–1104 (2020). https://doi.org/10.1007/s00167-019-05714-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05714-w