Abstract
Purpose
The acromioclavicular ligament complex (ACLC) is the primary stabilizer against horizontal translation with the superior ACLC providing the main contribution. The purpose of this study was to evaluate the specific regional contributions in the superior half of ACLC, where the surgeon can easily access and repair or reconstruct, for posterior translational and rotational stability.
Methods
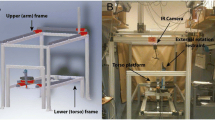
The superior half of ACLC was divided into three regions; Region A (0°–60°): an anterior 1/3 region of the superior half of ACLC, Region B (60°–120°): a superior 1/3 region of the superior half of ACLC, and Region C (120°–180°): a posterior 1/3 region of the superior half of ACLC. Fifteen fresh-frozen cadaveric shoulders were used. Biomechanical testing was performed to evaluate the resistance force against passive posterior translation (10 mm) and the resistance torque against passive posterior rotation (20°) during the following the four conditions. (1) Stability was tested on all specimens in their intact condition (n = 15). (2) The ACLC was dissected and stability was tested (n = 15). (3) Specimens were randomly divided into three groups by regions of suturing. Stability was tested after suturing Region A, Region B, or Region C (n = 5 per group). (4) Stability was tested after suturing additional regions: Region A + B (0°–120°), Region B + C (60°–180°), or Region A + C (0°–60°, 120°–180°, n = 5 per group).
Results
The translational force increased after suturing Region A when compared with dissected ACLC (P = 0.025). The force after suturing Region A + B was significantly higher compared to the dissected ACLC (P < 0.001). The rotational torque increased after suturing Region A or Region B compared with dissected ACLC (P = 0.020, P = 0.045, respectively). The torque after suturing the Region A + C was significantly higher compared to the dissected ACLC (P < 0.001).
Conclusion
The combined Region A + B contributed more to posterior translational stability than Region B + C or Region A + C. In contrast, combined Region A + C contributed more to posterior rotational stability than Region A + B or Region B + C. Based on these findings, surgical techniques restoring the entire superior ACLC are recommended to address both posterior translational and rotational stability of the AC joint.







Similar content being viewed by others
References
Barth J, Duparc F, Baverel L, Bahurel J, Toussaint B, Bertiaux S et al (2015) Prognostic factors to succeed in surgical treatment of chronic acromioclavicular dislocations. Orthop Traumatol Surg Res 101:S305–S311
Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG et al (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29:387–397
Beitzel K, Obopilwe E, Apostolakos J, Cote MP, Russell RP, Charette R et al (2014) Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med 42:2141–2148
Beitzel K, Obopilwe E, Chowaniec DM, Niver GE, Nowak MD, Hanypsiak BT et al (2011) Biomechanical comparison of arthroscopic repairs for acromioclavicular joint instability: suture button systems without biological augmentation. Am J Sports Med 39:2218–2225
Beitzel K, Sablan N, Chowaniec DM, Obopilwe E, Cote MP, Arciero RA et al (2012) Sequential resection of the distal clavicle and its effects on horizontal acromioclavicular joint translation. Am J Sports Med 40:681–685
Braun S, Beitzel K, Buchmann S, Imhoff AB (2015) Arthroscopically assisted treatment of acute dislocations of the acromioclavicular joint. Arthrosc Tech 4:e681–e685
Dawson PA, Adamson GJ, Pink MM, Kornswiet M, Lin S, Shankwiler JA et al (2009) Relative contribution of acromioclavicular joint capsule and coracoclavicular ligaments to acromioclavicular stability. J Shoulder Elbow Surg 18:237–244
Debski RE, Parsons IMT, Woo SL, Fu FH (2001) Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am 83-A:1344–1351
Dyrna FGE, Imhoff FB, Voss A, Braun S, Obopilwe E, Apostolakos JM et al (2018) The integrity of the acromioclavicular capsule ensures physiological centering of the acromioclavicular joint under rotational loading. Am J Sports Med 46:1432–1440
Fukuda K, Craig EV, An KN, Cofield RH, Chao EY (1986) Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am 68:434–440
Hann C, Kraus N, Minkus M, Maziak N, Scheibel M (2018) Combined arthroscopically assisted coraco- and acromioclavicular stabilization of acute high-grade acromioclavicular joint separations. Knee Surg Sports Traumatol Arthrosc 26:212–220
Izadpanah K, Jaeger M, Ogon P, Sudkamp NP, Maier D (2015) Arthroscopically assisted reconstruction of acute acromioclavicular joint dislocations: anatomic AC ligament reconstruction with protective internal bracing-the “AC-RecoBridge” technique. Arthrosc Tech 4:e153–e161
Kibler WB, Sciascia AD, Morris BJ, Dome DC (2017) Treatment of symptomatic acromioclavicular joint instability by a docking technique: clinical indications, surgical technique, and outcomes. Arthroscopy 33:696–708
Kippe MA, Demetropoulos CK, Baker KC, Jurist KA, Guettler JH (2009) Failure of coracoclavicular artificial graft reconstructions from repetitive rotation. Arthroscopy 25:975–982
Klimkiewicz JJ, Williams GR, Sher JS, Karduna A, Des Jardins J, Iannotti JP (1999) The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg 8:119–124
Nakazawa M, Nimura A, Mochizuki T, Koizumi M, Sato T, Akita K (2016) The orientation and variation of the acromioclavicular ligament: an anatomic study. Am J Sports Med 44:2690–2695
Salzmann GM, Walz L, Buchmann S, Glabgly P, Venjakob A, Imhoff AB (2010) Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med 38:1179–1187
Scheibel M, Droschel S, Gerhardt C, Kraus N (2011) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 39:1507–1516
Tauber M, Gordon K, Koller H, Fox M, Resch H (2009) Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med 37:181–190
Tauber M, Valler D, Lichtenberg S, Magosch P, Moroder P, Habermeyer P (2016) Arthroscopic stabilization of chronic acromioclavicular joint dislocations: triple- versus single-bundle reconstruction. Am J Sports Med 44:482–489
Triantafyllopoulos IK, Lampropoulou-Adamidou K, Schizas NP, Karadimas EV (2017) Surgical treatment of acute type V acromioclavicular joint dislocations in professional athletes: an anatomic ligament reconstruction with synthetic implant augmentation. J Shoulder Elbow Surg 26:e369–e375
Voss A, Singh H, Dyrna F, Buchmann S, Cote MP, Imhoff AB et al (2017) Biomechanical analysis of intra-articular pressure after coracoclavicular reconstruction. Am J Sports Med 45:150–156
Weiser L, Nuchtern JV, Sellenschloh K, Puschel K, Morlock MM, Rueger JM et al (2017) Acromioclavicular joint dislocations: coracoclavicular reconstruction with and without additional direct acromioclavicular repair. Knee Surg Sports Traumatol Arthrosc 25:2025–2031
Funding
The University of Connecticut Health Center/UConn Musculoskeletal Institute has received direct funding and material support from Arthrex Inc., Naples, FL, USA. The company had no influence on study design, data collection, or interpretation of the results or the final manuscript.
Author information
Authors and Affiliations
Contributions
Authors DM, JDJ, EO, and BS participated in obtaining the data. Authors ADM and MPC were responsible for the analysis of data. Authors FD, FBI, and KB made substantial contribution in designing the methodology and providing oversight to the conduct of the study. All authors (DM, JDJ, EO, BS, ADM, MPC, FD, FBI, and KB) made significant contributions to the development and revision of the manuscript. In addition, all authors have given final approval for the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors DM, FD, JDJ, EO, FBI, BS declare no conflict of interest. MPC received personal fee from the Arthroscopy Association of North America. KB is a consultant for Arthrex GmbH, Germany. ADM received grants to his institution from Arthrex Inc. Naples, Fl, USA. He is a consultant for Arthrex Inc. Naples Fl, USA and Ortho x, Inc., Lewisville, TX, USA.
Ethical approval
The above study was conducted using only de-identified cadaveric specimens and is therefore not considered human subjects research. Our institutional review board (IRB) provides a Human Research Determination Form to help investigators determine whether IRB review is needed. While we have confirmed with our IRB that projects conducted in our biomechanics laboratory that utilize de-identified specimens does not constitute human subjects research and therefore no review required.
Rights and permissions
About this article
Cite this article
Morikawa, D., Dyrna, F., Cote, M.P. et al. Repair of the entire superior acromioclavicular ligament complex best restores posterior translation and rotational stability. Knee Surg Sports Traumatol Arthrosc 27, 3764–3770 (2019). https://doi.org/10.1007/s00167-018-5205-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5205-y