Abstract
Purpose
This study examined a cohort of primary knee arthroplasties revised for peri-prosthetic infection to (1) determine whether the microorganisms isolated by sampling (up to 6 months pre-operatively) are representative of the microorganisms encountered at the time of knee revision, (2) determine whether the antibiotic sensitivity profiles of matching organisms correlate and (3) determine whether the proportion of organism and antibiotic sensitivity matches is influenced by the type of infection, timing of sample collection and the type of microorganism isolated.
Methods
From the National Joint Registry database for England and Wales, a consecutive series of primary knee arthroplasties performed between 2003 and 2014 that went on to have a revision for peri-prosthetic infection were identified. Each case was then linked to a national microbiology database held by Public Health England. Following data linkage, intra-operative and pre-operative cultures were identified and compared in a group of 75 patients.
Results
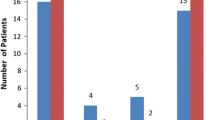
Pre-operative genus matched intra-operative genus in 56 of 75 cases (75 %). Of those 56, the corresponding antimicrobial sensitivities matched in 37 (66 % of cases). Overall, 37 of 75 cases (49 %) matched for both microorganism and antimicrobial sensitivity. The proportion of matches was highest in the pure Staphylococcal genus infections (genus match 88 %, sensitivity match 62 %, genus and sensitivity match 55 %) and lowest in those patients with mixed organism infections (genus match 29 %, sensitivity match 14 %).
Conclusion
Pre-operative joint sampling obtained by either aspiration or tissue biopsy is advocated in cases where peri-prosthetic infection is suspected and provides the only means of determining infecting organism prior to revision. Overall, only half of all pre-operative cultures matched completely the findings of intra-operative samples in terms of both the microorganism(s) encountered and their corresponding antimicrobial sensitivity profile. Clinicians should be vigilant regarding the possibility of the patient acquiring further microorganisms or the development of new antibiotic resistance by the time of revision, especially in historic pre-operative cultures. Broad spectrum antibiotic therapies should therefore be employed until final microorganisms and antimicrobial sensitivities are confirmed from intra-operative samples.
Level of evidence
IV.

Similar content being viewed by others
References
Baker P, Petheram TG, Kurtz S, Konttinen YT, Gregg P, Deehan D (2013) Patient reported outcome measures after revision of the infected TKR: comparison of single versus two-stage revision. Knee Surg Sports Traumatol Arthrosc 21:2713–2720
Blake MP, Halasz SJ (1995) The effects of X-ray contrast media on bacterial growth. Australas Radiol 39:10–13
Buchholz HW, Elson RA, Engelbrecht E, Lodenkämper H, Röttger J, Siegel A (1981) Management of deep infection of total hip replacement. J Bone Joint Surg Br 63-B:342–353
Burnett RSJ, Aggarwal A, Givens SA, McClure JT, Morgan PM, Barrack RL (2009) Prophylactic antibiotics do not affect cultures in the treatment of an infected TKA: a prospective trial. Clin Orthop Relat Res 468:127–134
Duff GP, Lachiewicz PF, Kelley SS (1996) Aspiration of the knee joint before revision arthroplasty. Clin Orthop Relat Res 331:132–139
von Essen R (1997) Culture of joint specimens in bacterial arthritis. Impact of blood culture bottle utilization. Scand J Rheumatol 26:293–300
Fink B, Makowiak C, Fuerst M, Berger I, Schäfer P, Frommelt L (2008) The value of synovial biopsy, joint aspiration and C-reactive protein in the diagnosis of late peri-prosthetic infection of total knee replacements. J Bone Joint Surg Br 90:874–878
Holleyman RJ, Baker P, Charlett A, Gould K, Deehan DJ (2015) Microorganisms responsible for periprosthetic knee infections in England and Wales. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3539-2
Johnson JA, Christie MJ, Sandler MP, Parks PF, Homra L, Kaye JJ (1988) Detection of occult infection following total joint arthroplasty using sequential technetium-99 m HDP bone scintigraphy and indium-111 WBC imaging. J Nucl Med 29:1347–1353
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27(61–5):e1
Meehan JP, Danielsen B, Kim SH, Jamali AA, White RH (2014) Younger age is associated with a higher risk of early periprosthetic joint infection and aseptic mechanical failure after total knee arthroplasty. J Bone Joint Surg Am 96:529–535
Meermans G, Haddad FS (2010) Is there a role for tissue biopsy in the diagnosis of periprosthetic infection? Clin Orthop Relat Res 468:1410–1417
Moran E, Masters S, Berendt AR, McLardy-Smith P, Byren I, Atkins BL (2007) Guiding empirical antibiotic therapy in orthopaedics: the microbiology of prosthetic joint infection managed by debridement, irrigation and prosthesis retention. J Infect 55:1–7
Mortazavi SMJ, Vegari D, Ho A, Zmistowski B, Parvizi J (2011) Two-stage exchange arthroplasty for infected total knee arthroplasty: predictors of failure. Clin Orthop Relat Res 469:3049–3054
Parvizi J, Azzam K, Ghanem E, Austin MS, Rothman RH (2009) Periprosthetic infection due to resistant staphylococci: serious problems on the horizon. Clin Orthop Relat Res 467:1732–1739
Parvizi J, Erkocak OF, Valle Della CJ (2014) Culture-negative periprosthetic joint infection. J Bone Joint Surg Am 96:430–436
Parvizi J, Gehrke T, Chen AF (2013) Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J 95-B:1450–1452
Parvizi J, Pawasarat IM, Azzam KA, Joshi A, Hansen EN, Bozic KJ (2010) Periprosthetic joint infection: the economic impact of methicillin-resistant infections. J Arthroplasty 25:103–107
Phillips WC, Kattapuram SV (1983) Efficacy of preoperative hip aspiration performed in the radiology department. Clin Orthop Relat Res 179:141–146
Qu X, Zhai Z, Wu C, Jin F, Li H, Wang L, Liu G, Liu X, Wang W, Li H, Zhang X, Zhu Z, Dai K (2013) Preoperative aspiration culture for preoperative diagnosis of infection in total hip or knee arthroplasty. J Clin Microbiol 51:3830–3834
Squire MW, Valle Della CJ, Parvizi J (2011) Preoperative diagnosis of periprosthetic joint infection: role of aspiration. Am J Roentgenol 196:875–879
Van den Bekerom MPJ, Stuyck J (2006) The value of pre-operative aspiration in the diagnosis of an infected prosthetic knee: a retrospective study and review of literature. Acta Orthop Belg 72:441–447
Acknowledgments
The authors would like to thank the patients and staff of all the hospitals in England, Wales and Northern Ireland who have contributed data to the National Joint Registry. We are grateful to the Healthcare Quality Improvement Partnership (HQIP), the NJR steering committee and the staff at the NJR centre for facilitating this work. The authors have conformed to the NJR’s standard protocol for data access and publication. The views expressed represent those of the authors and do not necessarily reflect those of the National Joint Register Steering Committee or the Health Quality Improvement Partnership (HQIP), who do not vouch for how the information is presented.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
Appendix
Rights and permissions
About this article
Cite this article
Holleyman, R.J., Deehan, D.J., Charlett, A. et al. Does pre-operative sampling predict intra-operative cultures and antibiotic sensitivities in knee replacements revised for infection?: a study using the NJR dataset. Knee Surg Sports Traumatol Arthrosc 24, 3056–3063 (2016). https://doi.org/10.1007/s00167-015-3841-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3841-z