Abstract
Purpose
This study aimed to delineate epidemiology of infecting microorganism genus in first-time revision knee arthroplasty for indication of periprosthetic joint infection in England and Wales using linked registry data.
Methods
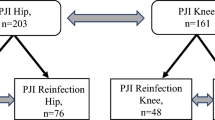
From the National Joint Registry database for England and Wales, a consecutive series of primary knee arthroplasties performed between April 2003 and January 2014 that went on to have a revision for periprosthetic infection were identified (n = 2810). Each case was then linked to microbiology data held by Public Health England in order to identify infecting microorganism at time of revision surgery established from intra-operative cultures. Following data linkage, 403 culture results at time of revision surgery were identified in a group of 331 patients. The demographic characteristics of five microorganism groups were compared: pure staphylococcus (single genus), pure streptococcus (single genus), other gram-positive infections (single genus), gram-negative infections (single genus) and mixed genus infections.
Results
Staphylococcus species was the most common organism genus isolated after revision of a primary implant for infection and present in 72 % of cases overall (71.3 % of patients with a single-genus infection and 76.8 % of patients with mixed genus infection). A pure staphylococcal infection was present in 59 % of all cases. A single-genus infection was responsible for infection in 83.1 % of cases, and mixed genera were responsible in 16.9 % of cases. A significant difference was observed for mean age at primary procedure in the cohort of patients where there was an isolated pure streptococcal infection (73.2 years) when compared to gram-negative infections (65.0 years). No other significant differences were observed between microorganism groups in terms of BMI, gender, ASA grade, indication for primary procedure and primary implant characteristics.
Conclusion
Staphylococci were the most commonly isolated organism species responsible for periprosthetic infection of primary arthroplasty in England and Wales. This information can be used by surgeons to benchmark and audit their own practice against national, publicly available data. Furthermore, this study has shown that even when using the largest national databases available, there is a substantial volume of missing data. Antimicrobial resistance represents a growing clinical problem with significant health and social costs. In order to counteract this threat, this study would advocate the consolidation of national microbial data in order to guide effective strategies towards targeting and combating the threat of antimicrobial resistance.
Level of evidence
IV.

Similar content being viewed by others
References
Aggarwal V, Bakhshi H, Ecker N, Parvizi J, Gehrke T, Kendoff D (2014) Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J Knee Surg 27:399–406
Baker P, Cowling P, Kurtz S, Jameson S, Gregg P, Deehan D (2012) Reason for revision influences early patient outcomes after aseptic knee revision. Clin Orthop Relat Res 470:2244–2252
Baker P, Petheram TG, Kurtz S, Konttinen YT, Gregg P, Deehan D (2013) Patient reported outcome measures after revision of the infected TKR: comparison of single versus two-stage revision. Knee Surg Sports Traumatol Arthrosc 21:2713–2720
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ (2009) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51
Bozic KJ, Ries MD (2005) The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am 87:1746–1751
Charnley J, Eftekhar N (1969) Postoperative infection in total prosthetic replacement arthroplasty of the hip-joint. With special reference to the bacterial content of the air of the operating room. Br J Surg 56:641–649
Fulkerson E, Valle CJD, Wise B, Walsh M, Preston C, Di Cesare PE (2006) Antibiotic susceptibility of bacteria infecting total joint arthroplasty sites. J Bone Joint Surg Am 88:1231–1237
Jämsen E, Huhtala H, Puolakka T, Moilanen T (2009) Risk factors for infection after knee arthroplasty. A register-based analysis of 43,149 cases. J Bone Joint Surg Am 91:38–47
Koyonos L, Zmistowski B, Valle Della CJ, Parvizi J (2011) Infection control rate of irrigation and débridement for periprosthetic joint infection. Clin Orthop Relat Res 469:3043–3048
Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J (2012) Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 27:61.e1–65.e1
Lavernia C, Lee DJ, Hernandez VH (2006) The increasing financial burden of knee revision surgery in the United States. Clin Orthop Relat Res 446:221–226
Mittal Y, Fehring TK, Hanssen A, Marculescu C, Odum SM, Osmon D (2007) Two-stage reimplantation for periprosthetic knee infection involving resistant organisms. J Bone Joint Surg Am 89:1227–1231
Mortazavi SMJ, Vegari D, Ho A, Zmistowski B, Parvizi J (2011) Two-stage exchange arthroplasty for infected total knee arthroplasty: predictors of failure. Clin Orthop Relat Res 469:3049–3054
National Joint Registry for England, Wales, Ireland N (2014) 11th annual report. National Joint Registry for England, Wales and Northern Ireland, pp 1–135
Odum SM, Fehring TK, Lombardi AV, Zmistowski BM, Brown NM, Luna JT, Fehring KA, Hansen EN, Periprosthetic Infection Consortium (2011) Irrigation and debridement for periprosthetic infections: does the organism matter? J Arthroplasty 26:114–118
Peersman G, Laskin R, Davis J, Peterson M (2001) Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res 392:15–23
Phillips JE, Crane TP, Noy M, Elliott TSJ, Grimer RJ (2006) The incidence of deep prosthetic infections in a specialist orthopaedic hospital: a 15-year prospective survey. J Bone Joint Surg Br 88:943–948
Pulido L, Ghanem E, Joshi A, Purtill JJ, Parvizi J (2008) Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res 466:1710–1715
Pun SY, Ries MD (2008) Effect of gender and preoperative diagnosis on results of revision total knee arthroplasty. Clin Orthop Relat Res 466:2701–2705
Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB (1999) Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am 81:1434–1445
Stefánsdóttir A, Johansson D, Knutson K, Lidgren L, Robertsson O (2009) Microbiology of the infected knee arthroplasty: report from the Swedish Knee Arthroplasty Register on 426 surgically revised cases. Scand J Infect Dis 41:831–840
Van Houwelingen AP, Garbuz DS, Masri BA, Duncan CP (2012) Methicillin-resistant infection after hip and knee replacement: reason to change practice? J Orthop Trauma Rehabil 16:9–12
van Kempen RWTM, Schimmel JJP, van Hellemondt GG, Vandenneucker H, Wymenga AB (2013) Reason for revision TKA predicts clinical outcome: prospective evaluation of 150 consecutive patients with 2-years followup. Clin Orthop Relat Res 471:2296–2302
Acknowledgments
The authors would like to thank the patients and staff of all the hospitals in England, Wales and Northern Ireland who have contributed data to the National Joint Registry. We are grateful to the Healthcare Quality Improvement Partnership (HQIP), the NJR steering committee and the staff at the NJR centre for facilitating this work. The authors have conformed to the NJR’s standard protocol for data access and publication.
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding author
Additional information
The views expressed represent those of the authors and do not necessarily reflect those of the National Joint Register Steering Committee or the Health Quality Improvement Partnership (HQIP), who do not vouch for how the information is presented.
Rights and permissions
About this article
Cite this article
Holleyman, R.J., Baker, P., Charlett, A. et al. Microorganisms responsible for periprosthetic knee infections in England and Wales. Knee Surg Sports Traumatol Arthrosc 24, 3080–3087 (2016). https://doi.org/10.1007/s00167-015-3539-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3539-2