Abstract
Purpose
Quantitative MRI T2 mapping is a non-invasive imaging technique sensitive to biochemical changes, but no studies have evaluated T2 mapping in pathologic rotator cuff tendons. It was sought to evaluate the efficacy of T2 mapping in detecting differences in the supraspinatus tendon (SST) among patients with tendinosis, partial tears and minimally retracted full-thickness tears, relative to asymptomatic volunteers.
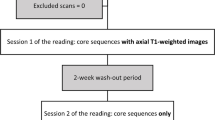
Methods
The pathologic cohort consisted of two arthroscopically verified groups: tendinosis and a tear group of partial tears or minimally retracted full-thickness tears, and was compared to an asymptomatic cohort with no prior history of shoulder pathology. The SST was manually segmented from the footprint to the medial humeral head in the coronal and sagittal planes and divided into six clinically relevant subregions. Mean T2 values and inter- and intra-rater reliability were assessed.
Results
In the anterolateral subregion, the tear group exhibited significantly higher mean T2 values (43.9 ± 12.7 ms) than the tendinosis (34.9 ± 3.9 ms; p = 0.006) and asymptomatic (33.6 ± 5.3 ms; p = 0.015) groups. In the posterolateral subregion, the tear group had higher mean T2 values (45.2 ± 13.7) than the asymptomatic group (34.7 ± 6.7; p = 0.012). Inter- and intra-rater reliability was mostly excellent (ICC > 0.75).
Conclusion
T2 mapping is an accurate non-invasive method to identify quantitatively early rotator cuff pathology. The lateral region in the coronal plane in particular may differentiate partial and small minimally retracted full-thickness tears from tendinosis and asymptomatic tendons. Understanding and being able to measure quantitatively the process of tendon degeneration and subsequent tearing may help clinicians to better predict at-risk groups and to stratify treatment options.
Level of evidence
III.



Similar content being viewed by others
References
Anz AW, Lucas EP, Fitzcharles EK, Surowiec RK, Millett PJ, Ho CP (2014) MRI T2 mapping of the asymptomatic supraspinatus tendon by age and imaging plane using clinically relevant subregions. Eur J Radiol 83(5):801–805
Balich SM, Sheley RC, Brown TR, Sauser DD, Quinn SF (1997) MR imaging of the rotator cuff tendon: interobserver agreement and analysis of interpretive errors. Radiology 204:191–194
Bedi A, Maak T, Walsh C, Rodeo SA, Grande D, Dines DM, Dines JS (2012) Cytokines in rotator cuff degeneration and repair. J Shoulder Elb Surg 21:218–227
Bryant L, Shnier R, Bryant C, Murrell GA (2002) A comparison of clinical estimation, ultrasonography, magnetic resonance imaging and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elb Surg 11:219–224
Buck FM, Grehn H, Hilbe M, Pfirrmann CW, Manzanell S, Hodler J (2010) Magnetic resonance histologic correlation in rotator cuff tendons. J Magn Reson Imaging 32:165–172
Fleiss JL (1986) The design and analysis of clinical experiments. Wiley, New York
Juras V, Apprich S, Pressl C, Zbyn S, Szomolanyi P, Domayer S, Hofstaetter JG, Trattnig S (2013) Histological correlation of 7 T multi-parametric MRI performed in ex vivo Achilles tendon. Eur J Radiol 82:740–744
Juras V, Zbyn S, Pressl C, Valkovic L, Szomolanyi P, Frollo I, Trattnig S (2012) Regional variations of T2* in healthy and pathologic achilles tendon in vivo at 7 Tesla: preliminary results. Magn Reson Med 5:1607–1613
Kang JR, Gupta R (2012) Mechanisms of fatty degeneration in massive rotator cuff tears. J Shoulder Elb Surg 21:175–180
Khazzam M, Kuhn JE, Mulligan E, Abboud JA, Baumgarten KM, Brophy RH, Jones GL, Miller B, Smith M, Wright RW (2012) Magnetic resonance imaging identification of rotator cuff retears after repair: interobserver and intraobserver agreement. Am J Sports Med 40:1722–1727
Kijowski R, Blankenbaker DG, Munoz Del Rio A, Baer GS, Graf BK (2013) Evaluation of the articular cartilage of the knee joint: value of adding a T2 mapping sequence to a routine MR imaging protocol. Radiology 267:503–513
Kim M, Dahiya N, Teefey SA, Middleton WD, Stobbs G, Steger-May K, Yamaguchi K, Keener JD (2010) Location and initiation of degenerative rotator cuff tears. J Bone Joint Surg Am 92:1088–1096
Kim T, Min BH, Yoon SH, Kim H, Park S, Lee HY, Kwack KS (2014) An in vitro comparative study of T2 and T2* mappings of human articular cartilage at 3-Tesla MRI using histology as the standard of reference. Skelet Radiol 43:947–954
Lattanzi R, Petchprapa C, Ascani D, Babb JS, Chu D, Davidovitch RI, Youm T, Meislin RJ, Recht MP (2014) Detection of cartilage damage in femoroacetabular impingement with standardized dGEMRIC at 3 T. Osteoarthr Cartil 22:447–456
Liem D, Lichtenberg S, Magosch P, Habermeyer P (2007) Magnetic resonance imaging of arthroscopic supraspinatus tendon repair. J Bone Joint Surg Am 89:1770–1776
Longo UG, Franceschi F, Ruzzini L, Rabitti C, Morini S, Maffulli N, Denaro V (2008) Histopathology of the supraspinatus tendon in rotator cuff tears. Am J Sports Med 36:533–538
Malhi AM, Khan R (2005) Correlation between clinical diagnosis and arthroscopic findings of the shoulder. Postgrad Med J 81:657–659
Matsen FA III, Arntz CT, Lippitt SB (1998) Rotator Cuff. In: Rockwood CA, Matsen FA III (eds) The shoulder, 2nd edn. Saunders, Philadelphia, pp 755–839
Mazzocca AD, Rincon LM, O’Connor RW, Obopilwe E, Anderson M, Geaney L, Arciero RA (2008) Intra-articular partial-thickness rotator cuff tears: analysis of injured and repaired strain and behavior. Am J Sports Med 36:110–116
Mochizuki T, Sugaya H, Uomizu M, Maeda K, Matsuki K, Sekiya I, Muneta T, Akita K (2008) Humeral insertion of the supraspinatus and infraspinatus. J Bone Joint Surg Am 90:962–969
Nho SJ, Yadav H, Shindle MK, MacGillivray JD (2008) Rotator cuff degeneration: etiology and pathogenesis. Am J Sports Med 36:987–993
Nishioka H, Hirose J, Nakamura E, Okamoto N, Karasugi T, Taniwaki T, Okada T, Yamashita Y, Mizuta H (2013) Detecting ICRS grade 1 cartilage lesions in anterior cruciate ligament injury using T1rho and T2mapping. Eur J Radiol 82:1499–1505
Nishioka H, Hirose J, Nakamura E, Oniki Y, Takada K, Yamashita Y, Mizuta H (2012) T1ρ and T2 mapping reveal the in vivo extracellular matrix of articular cartilage. J Magn Reson Imaging 35:147–155
Nissi MJ, Töyräs J, Laasanen MS, Rieppo J, Saarakkala S, Lappalainen R, Jurvelin JS, Nieminen MT (2004) Proteoglycan and collagen sensitive MRI evaluation of normal and degenerated articular cartilage. J Orthop Res 22:557–564
Ostör AJ, Richards CA, Tytherleigh-Strong G, Bearcroft PW, Prevost AT, Speed CA, Hazleman BL (2013) Validation of clinical examination versus magnetic resonance imaging and arthroscopy for the detection of rotator cuff lesions. Clin Rheumatol 32:1283–1291
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res 254:81–86
Reinus WR, Shady KL, Mirowitz SA, Totty WG (1995) MR diagnosis of rotator cuff tears of the shoulder: value of using T2-weighted fat-saturated images. Am J Roentgenol 164:1451–1455
Robertson PL, Schweitzer ME, Mitchell DG, Schlesinger F, Epstein RE, Frieman BG, Fenlin JM (1995) Rotator cuff disorders: interobserver and intraobserver variation in diagnosis with MR imaging. Radiology 194:831–835
Spencer EE, Dunn WR, Wright RW, Wolf BR, Spindler KP, McCarty E, Ma CB, Jones G, Safran M, Holloway GN, Kuhn JE (2008) Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med 36:99–103
Takamiya H, Kusaka Y, Seo Y, Noguchi M, Ikoma K, Morimoto T, Hirasawa Y (2000) Characteristics of proton NMR T(2) relaxation of water in the normal and regenerating tendon. Jpn J Physiol 50:569–576
Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K (2004) Detection and quantification of rotator cuff tears. comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am 86-A:708–716
Vitale MA, Vitale MG, Zivin JG, Braman JP, Bigliani LU, Flatow EL (2007) Rotator cuff repair: an analysis of utility scores and cost-effectiveness. J Shoulder Elb Surg 16(2):181–187
Watrin-Pinzano A, Ruaud JP, Olivier P, Grossin L, Gonord P, Blum A, Netter P, Guillot G, Gillet P, Loeuille D (2005) Effect of proteoglycan depletion on T2 mapping in rat patellar cartilage. Radiology 234:162–170
Williams A, Qian Y, Golla S, Chu CR (2012) UTE-T2* mapping detects sub-clinical meniscus injury after anterior cruciate ligament tear. Osteoarthr Cartil 20:486–494
Yao W, Qu N, Lu Z, Yang S (2009) The application of T1 and T2 relaxation time and magnetization transfer ratios to the early diagnosis of patellar cartilage osteoarthritis. Skelet Radiol 38:1055–1062
Acknowledgments
Funding for this study came from the internal institution Steadman Philippon Research Institute, where the research was performed. None of the authors have a conflict of interest related to the subject of this article.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study. This study was approved by the Institutional Review Board at Steadman Philippon Research Institute, and the approved protocol number is 2012–2007.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ganal, E., Ho, C.P., Wilson, K.J. et al. Quantitative MRI characterization of arthroscopically verified supraspinatus pathology: comparison of tendon tears, tendinosis and asymptomatic supraspinatus tendons with T2 mapping. Knee Surg Sports Traumatol Arthrosc 24, 2216–2224 (2016). https://doi.org/10.1007/s00167-015-3547-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3547-2