Abstract
We present areas of uncertainty concerning intensive care unit-acquired weakness (ICUAW) and identify areas for future research. Age, pre-ICU functional and cognitive state, concurrent illness, frailty, and health trajectories impact outcomes and should be assessed to stratify patients. In the ICU, early assessment of limb and diaphragm muscle strength and function using nonvolitional tests may be useful, but comparison with established methods of global and specific muscle strength and physical function and determination of their reliability and normal values would be important to advance these techniques. Serial measurements of limb and respiratory muscle strength, and systematic screening for dysphagia, would be helpful to clarify if and how weakness of these muscle groups is independently associated with outcome. ICUAW, delirium, and sedatives and analgesics may interact with each other, amplifying the effects of each individual factor. Reduced mobility in patients with hypoactive delirium needs investigations into dysfunction of central and peripheral nervous system motor pathways. Interventional nutritional studies should include muscle mass, strength, and physical function as outcomes, and prioritize elucidation of mechanisms. At follow-up, ICU survivors may suffer from prolonged muscle weakness and wasting and other physical impairments, as well as fatigue without demonstrable weakness on examination. Further studies should evaluate the prevalence and severity of fatigue in ICU survivors and define its association with psychiatric disorders, pain, cognitive impairment, and axonal loss. Finally, methodological issues, including accounting for baseline status, handling of missing data, and inclusion of patient-centered outcome measures should be addressed in future studies.
Similar content being viewed by others

Introduction
Surviving critical illness is not benign. Professor Richard Griffiths previously commented that “we have learned about the ‘legacy of critical care’ and how having a critical illness impacts life after ICU through its consequential effects on physical and psychological function and the social landscape” [1].
Intensive care unit (ICU)-acquired weakness (ICUAW) develops as a complication of critical illness [2] (suppl ref [1–5]) and may represent the extreme end of a spectrum of weakness that begins with any serious illness regardless of care location (suppl ref [6]). ICUAW is associated with prolonged mechanical ventilation and ICU stay, as well as increased ICU, hospital, and 1-year mortality [3] (suppl ref [3, 5–7]). Age, sepsis, longer ICU length of stay, longer duration of mechanical ventilation, and bed rest increase the risk of developing ICUAW [3]. Long-term impairment of physical function can persist for months or even years after ICU discharge.
In a round table meeting that was held in Brussels in March 2016, the factors that impact on recovery after critical illness were examined in detail with a major recommendation to “look outside the ICU and embrace the continuum of illness including pre-ICU trajectory, recovery, and adaptation”.
The aim of this review is to present the areas of uncertainty concerning ICUAW to inform future research.
Impact of pre-ICU admission status
Age, functional status, comorbidity, frailty, and trajectory of health status
Background
The patients’ functional and neurocognitive state prior to critical illness is the upper limit for post-ICU recovery, affecting both their absolute level of function and the rate of change in function over time. In acute respiratory distress syndrome (ARDS) survivors, older age and comorbidity are associated with decline in physical status over the subsequent 5 years [4, 5]. In older populations, pre-ICU disability and hearing and visual impairment substantially increase the risk of death and more severe disability following critical illness [6, 7]. Comorbid conditions have a great impact on acute mortality, long-term residual disability, and response to rehabilitation [8] (suppl ref [8]). Frailty identifies a vulnerable population at increased risk of multiple adverse outcomes (suppl ref [9–11]). Decreased functional capacity prior to hospital admission is associated with increased hospital mortality regardless of age, comorbidities, disease severity, and type of ICU admission [9]. Admission to the ICU from within the hospital as a marker of poor health status portends an unfavorable prognosis [10].
In individuals 70 years or older [6], the pre-ICU functional trajectory strongly influences post-ICU functional status. Pre-morbid health status, functional decline in the ICU, and post-ICU functional status are likely determined by a complexity of different factors over time (suppl ref [12]). For example, patients with sepsis, a major risk factor for ICUAW [3], have substantial excess attributable mortality even after matching for prior health status [11] and those with worse pre-sepsis health or functional status may also have increased mortality. Thus, the complex interplay between pre-existing health status and acute and persisting critical illness in determining long-term functional and cognitive outcome remains to be elucidated at a disease-specific mechanistic level to inform bedside decision-making and therapy for individual patients (Fig. 1) [5, 10, 12, 13].

Modified from Iwashyna (2012) Trajectories of recovery and dysfunction after acute illness, with implications for clinical trial design. Am J Respir Crit Care Med, 186, pp 302–304 [12]
Possible trajectories of recovery with interaction between pre-ICU status and trajectory, and duration of ICU stay. Recovery across different patient groups can be variable. Healthy young individuals with short duration of ICU stay are more likely to recover their pre-ICU functional condition and have faster recovery compared to young individuals with comorbidity or elderly individuals with severe comorbidity and prolonged ICU stay [6, 10, 13]. Trajectories of recovery can be characterized by acute functional decline in the ICU followed by recovery (A, “big hit”); constant decline over time (B, “slow burn”); or repeated acute exacerbations and partial recoveries (C, “relapsing recurrences”) [5, 12]. Hatched lines indicate the trajectories of functioning that would have occurred if the subject had not developed critical illness
Limits of current knowledge
Few longitudinal studies with accurate assessment of pre-ICU condition have evaluated the impact of critical illness on late functional impairment [6, 14, 15].
Indications for future studies
The trajectory of patients’ pre-ICU health status may be difficult to capture but conveys important prognostic information. Studies on long-term outcomes should consider age, pre-ICU functional and cognitive status, concurrent burden of illness, frailty, and current trajectory of health status to target patient populations that can achieve functional independence and good patient- and family-centered outcomes after critical illness.
Diagnosis and treatment
Limb muscle involvement
Background
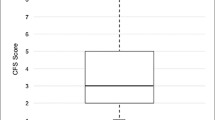
ICUAW is a clinical diagnosis made by physical examination of muscle strength using volitional tests such as the Medical Research Council sum score (MRCss) or a handgrip dynamometer [2] (suppl ref [5, 7, 13]). Muscle weakness is generalized, symmetrical, and affects both limb and respiratory skeletal muscles; however, clinical phenotype can be different depending on age, burden of comorbid disease, and duration of ICU stay and mechanical ventilation [16]. With MRCss, muscle strength is assessed in 12 muscle groups and a summed score below 48/60 designates ICUAW (suppl ref [5]). With handgrip dynamometry, cutoff scores of less than 11 kg (IQR 10–40) in men and less than 7 kg (IQR 0–7.3) in women indicates ICUAW (suppl ref [14]). Nonvolitional tests include electrical and magnetic neuromuscular twitch stimulation to assess strength and muscle ultrasound to assess skeletal muscle mass and architecture [17] (suppl ref [15–17]). Loss of muscle mass, as evidenced by a reduction in rectus femoris muscle cross-sectional area, is dependent on the severity of the illness with multiorgan failure associated with greatest loss of skeletal muscle [18, 19]. Muscle mass at ICU admission may be an independent predictor of mortality (suppl ref [18]), and lower admission muscle mass may be associated with increased disability and higher frequency of discharge to a nursing home (suppl ref [18]).
Ultrasound can confirm histologically defined myofiber necrosis (muscle echogenicity) as well as fascial inflammation and fasciitis (fascial echogenicity) [20]. Muscle necrosis portends a worse prognosis than loss of myosin filaments [2], and fascial inflammation and fasciitis may cause severe pain [20].
Electrophysiological studies (EPS) of peripheral nerves and muscles assess whether ICUAW is caused by a critical illness polyneuropathy (CIP) (suppl ref [1–3]), myopathy (CIM), or both [21] (suppl ref [4]). EPS can inform prognosis and pathways by which ICUAW may occur [2]. Normal EPS implies disuse atrophy, which may have a better prognosis than CIP or CIM (suppl ref [19]). Simplified electrophysiological tests are feasible in the ICU (for review, see [21]) (suppl ref [20]), and, if abnormal, may predict short-term (suppl ref [21, 22]) and long-term physical dysfunction and mortality [22] (suppl ref [23, 24]). The peroneal nerve test (PENT) has been validated in two multicenter prospective studies as a reliable substitute for complete EPS [23].
Limits of current knowledge
Volitional tests can be assessed in a minority of patients who are awake and cooperative (suppl ref [17, 25, 26]). MRC has limitations including a ceiling effect and inability to detect less severe forms of ICUAW, difficulty in differentiation between MRC grades 3 and 4 (suppl ref [17, 27]), and weak correlations with physical functioning [24] (suppl ref [26]). It is uncertain if handgrip strength is representative of global muscle strength in critically ill patients (suppl ref [17, 28]). Further evaluation of the measurement properties of nonvolitional tests is needed.
Ultrasound evaluates alterations of limb muscle size and structure. However, the clinical relevance of these observations is yet to be determined, and further correlation with muscle strength and functional outcome is needed.
EPS are complex and require specialized training. Moreover, EPS are done infrequently because management is supportive regardless of specific diagnosis. When using EPS without clinical evaluation, only a diagnosis of “probable” CIP or CIM can be established [2] for which the impact on outcome might be relevant [22].
There are no specific treatments with proven efficacy for ICUAW. Intensive insulin treatment to achieve normal blood glucose reduces EPS-proven CIP and reduces the duration of mechanical ventilation, but exposes patients to an increased risk of hypoglycemia (suppl ref [29–33]). Neuromuscular electrical stimulation (NMES) restores impaired glucose transporter-4 (GLUT4) translocation to the sarcolemmal membrane, which is a central mechanism of impaired glucose supply to muscle cells in patients with CIM [25], and can be used at the bedside to stimulate nerve-muscle function, but effectiveness is not yet proven (suppl ref [34]). Early mobilization and rehabilitation in the ICU are safe [26–28] (suppl ref [35]); they have positive effects on short-term outcome in medical and surgical ICU patients when initiated early [26, 28] (suppl ref [36, 37]), but not if started late [29, 30], or if not combined with optimized sedation protocols [31]. The effects of early mobilization and rehabilitation on long-term outcome are unknown [32] (suppl ref [38]). An integrated approach of early mobilization and rehabilitation in the ICU with standardized rehabilitation in the hospital and after hospital discharge may be beneficial in patients with no preexisting chronic disease [8].
Indications for future studies
Within populations of critically ill patients, further evaluation of nonvolitional measurements of muscle strength and function with established methods of global and specific muscle strength and physical function [4, 5, 33] (suppl ref [15–17]), assessment of inter- and intrarater reliability, and determination of normal values would be important to advance these techniques.
Diagnostic utility of simplified electrophysiological tests and muscle ultrasound performed by ICU personnel should be further evaluated for potential adoption in daily practice. Also partnership with industry would be important to design low cost, simplified EPS and ultrasound machines to be tested for use in the ICU. Further observational studies could evaluate if pure electrophysiological abnormalities, as in probable CIP or CIM, or qualitative and quantitative changes in locomotor skeletal muscles are associated with hospital and long-term mortality and with persisting muscle weakness, fatigue, and physical dysfunction in survivors of critical illness. Randomized controlled trials (RCT) of treatment interventions could consider the use of EPS to identify patients without CIP or CIM who may be more likely to benefit from treatment [20]. Specific electrophysiological (i.e., normal findings, CIP, CIM, and combined CIP and CIM) (suppl ref [39]) and muscle ultrasound diagnoses (i.e., loss of muscle mass, fascial inflammation, and muscle fiber necrosis) should be confirmed as relevant outcome measures in adequately powered longitudinal studies.
Future studies should evaluate the impact of early mobilization in the ICU on long-term outcomes using a standardized set of outcome measures collected at consistent time points [32] (suppl ref [40]). Active and passive in-bed cycle ergometry, NMES, functional electrical stimulation cycling (i.e., combined NMES and bedside cycling), and whole body vibration are promising techniques that should continue to be tested in randomized clinical trials with the perspective of integrating these techniques into clinical practice for optimized mobilization [27]. Studies assessing the efficacy of specific treatments for ICUAW are urgently needed, as are studies assessing the effects of a continuum of physical rehabilitation from early ICU admission to post-acute care hospital discharge after stratifying cohorts by the presence or absence of chronic disease states.
Respiratory muscle involvement
Background
CIP, CIM, and diaphragm atrophy are important causes of failed weaning from the ventilator [2] (suppl ref [1, 41]). Diaphragm dysfunction assessed using bilateral anterior magnetic phrenic nerve stimulation and diaphragm ultrasonography is twice as frequent as limb muscle weakness and is directly associated with a high rate of weaning failure and mortality [34] (suppl ref [42]).
Ultrasound imaging of the diaphragm can be used to evaluate the diaphragmatic dysfunction or paralysis at the bedside (suppl ref [42–44]), to predict weaning failure, and to assess respiratory effort and progression of atrophy in mechanically ventilated patients [35–37].
Understanding respiratory muscle weakness after mechanical ventilation [as assessed by measuring maximal inspiratory pressure (MIP)] may be important given its association with 1-year mortality [38].
Inspiratory muscle training during mechanical ventilation increases inspiratory muscle strength and weaning success in the ICU [39] (suppl ref [45]), and may improve inspiratory muscle strength and quality of life after successful weaning in patients with prolonged mechanical ventilation [40].
ICU-acquired swallowing dysfunction is common and is associated with serious complications related to choking, aspiration, and respiratory failure, but is frequently under-recognized and poorly managed [41] (suppl ref [46]); aspiration pneumonia is among the top ten most common reasons for recurrent hospitalization in the 90 days after sepsis [42, 43]. Treatments include diet modification, postural and behavioral changes, enteral feeding tubes, and surface electromyography biofeedback [41] (suppl ref [47]).
Limits of current knowledge
Magnetic phrenic nerve stimulation is difficult to use in everyday practice. Inspiratory muscle strength, assessed using MIP, is a volitional testing that relies on patient cooperation and low values may reflect poor technique or effort, rather than true weakness [44]. Efficacy of inspiratory muscle training during weaning or in the post-extubation period has been explored in selected patient populations and in studies with short follow-up periods. Ultrasound-assessed diaphragmatic dysfunction has not been assessed in a large representative population of critically ill patients [37], and abdominal muscle dysfunction is awaiting further definition and assessment. Large prospective studies assessing the frequency of ICU-acquired swallowing dysfunction, using instrumental evaluation, are lacking, as are RCTs of potentially effective treatments.
Indications for future studies
Further studies could evaluate whether an increased duration of mechanical ventilation, by promoting bed rest, leads to ICUAW or if ICUAW primarily induces prolonged duration of MV. Ultrasound-assessed diaphragm dysfunction should be evaluated in large-scale prospective studies of unselected patient populations to determine feasibility and reproducibility of ultrasound findings, and to further evaluate derived parameters relative to clinically relevant outcomes. In mechanically ventilated patients, titration of ventilatory support to maintain normal levels of inspiratory effort may prevent decrease in diaphragm thickness with a potential impact on clinical outcomes [35], and warrants further study. Given that weakness of the abdominal muscles can impair effective cough, ultrasound evaluation could inform this disability as well. Further longitudinal studies with serial measurements of limb and respiratory muscle strength, and with proper consideration of age, pre-ICU functional status, comorbidity and frailty, and sepsis as confounders, would be helpful to clarify if weakness of these muscle groups is independently associated with outcome. Mechanisms of increased mortality after ICU discharge would also be worth studying (e.g., neuromuscular respiratory failure with inefficient cough, pneumonia, and increased rate of ICU readmission) (suppl ref [48]).
Systematic screening for dysphagia, using simple validated tests, in survivors of critical illness, as in acute stroke patients, should be further evaluated. Prospective evaluation of swallowing disorders with validation of bedside testing is needed [45]. Intervention studies for swallowing disorders are eagerly awaited.
Interaction between muscle weakness, sedatives, analgesics, and delirium
Background
Deep sedation is associated with a longer duration of mechanical ventilation, weaning time, and stay in the ICU, and increased mortality (suppl ref [49–53]). Delirium is a common and severe complication in ICU patients (suppl ref [54–59]). However, there is no evidence that sedatives, analgesics, or delirium have a direct impact on ICUAW. Immobility, a consequence of deep sedation, increases the risk of ICUAW (Fig. 2). Delirium and ICUAW possibly interact with each other as early rehabilitation in the ICU improves physical function and may reduce the duration of delirium [26, 28] (suppl ref [60]).
Limits of current knowledge
Ongoing NIH-sponsored investigations are exploring the co-occurrence of ICUAW and delirium, and whether these two conditions influence each other (Nathan Brummel and Wes Ely, personal communication, Grant number: K76AG054864, https://projectreporter.nih.gov/project_info_description.cfm?aid=9229869&icde=32020754&ddparam=&ddvalue=&ddsub=&cr=1&csb=default&cs=ASC).
No study has investigated the cause(s) of reduced mobility in patients with hypoactive delirium, whether it is the exclusive consequence of central nervous system (brain, spinal cord) or of combined central and peripheral nervous system motor pathway dysfunction (CIP, CIM). White matter abnormalities in the frontal lobe, corpus callosum, and anterior limb of the internal capsule are reported in patients with delirium, which might explain diminished motor activity [46]; however, it is unknown if these alterations are more common in patients with hypoactive delirium than in patients with hyperactive delirium.
Indications for future studies
Causes of reduced mobility in patients with hypoactive delirium could be investigated with EPS of peripheral nerves and muscles. Insights into central motor pathway involvement may be gained through the use of transcranial magnetic stimulation with measurement of central motor conduction time (suppl ref [61]). Moreover, diffusion tensor imaging [46] and dual-coil transcranial magnetic stimulation offer the opportunity to investigate plasticity and connectivity between different parts of the brain (suppl ref [62]), which can be relevant for studying pathophysiological mechanisms of concurrent ICUAW and delirium, and development of cognitive impairments in survivors of critical illness. Absence of intentional movements can be caused by selective structural damage to thalamocortical circuits that can be explored with functional magnetic resonance imaging studies (suppl ref [63]).
Interaction between muscle weakness and nutrition
Background
Critical illness induces a metabolic response, which secures energy provision to vital organs and protects processes of tissue repair and immune response. The muscle is a key player in this adaptive response as amino acids from increased proteolysis are made available for gluconeogenesis and production of acute phase proteins by the liver. Peripheral resistance to anabolic signaling further aggravates hyperglycemia and alters substrate availability in the muscle. Driving forces of this hypermetabolic response include stimulation of the sympathetic nervous system, inflammation, immobilization, and release of anterior pituitary hormones [47] (suppl ref [64]). Also, malnutrition due to poor gastrointestinal and metabolic function could contribute to pronounced muscle wasting and accompanying weakness in the acute stage of critical illness. Nutritional status indeed is linked to weakness: starvation in healthy volunteers causes loss of muscle mass, strength, and function (suppl ref [65]). Challenging this hypothesis is the finding that tolerating a macronutrient deficit in the early stage of critical illness, as compared to early caloric parenteral substitution, reduces the incidence of weakness and hastens recovery [48]. More efficient muscle cell autophagy preserving muscle structure can be the underlying mechanism [48]. Follow-up studies, from 60 days up to 12 months, corroborate that early hypocaloric feeding does not worsen muscle strength, physical function, or long-term quality of life [49–51]. The observation that a high protein feeding load is associated with greater skeletal muscle wasting also challenges the approach to current nutrition practices [18].
Limits of current knowledge
Attenuation of the hypermetabolic response by providing anabolic or anti-catabolic agents is feasible, but data supporting actual translation into clinical benefits are absent for most of these drugs and pharmaco-nutrients (suppl ref [64, 66]). This is troublesome as recombinant human growth hormone, which exerts clear anabolic effects in critically ill patients, increased mortality rates (suppl ref [67]). Intensive insulin therapy on the other hand improved electrophysiological signs of ICUAW and need for prolonged mechanical ventilation (suppl ref [29–31]), but these benefits could not be attributed to the anabolic effects of insulin [52], and hypoglycemia remains of concern (suppl ref [32]). Regarding nutrition, early hypocaloric feeding appears to be at least as good as a full caloric supply [48, 50, 51, 53] (suppl ref [68, 69]), but the optimal nutritional approach remains unclear (suppl ref [70, 71]). At some threshold, adequate energy supply undoubtedly becomes essential to promote anabolism. Biomarkers indicating this transition are absent. Nutritional assessment tool scores may be useful to select patients who may benefit most from optimal amounts of macronutrients, but their value has not been consistently demonstrated [54] (suppl ref [72–75]). Other approaches to improve protein synthesis, including intermittent bolus feeding compared to continuous feeding and the use of whey proteins compared to soy or casein-based proteins, warrant investigation (suppl ref [76]). Indirect calorimetry may better estimate “requirements” than energy equations, but its benefit on outcome is not established (suppl ref [77]). Nutritional content may be more important than caloric intake. In particular, preserved or enhanced protein intake to arrest catabolism and preserve muscle function is an exciting concept (suppl ref [78, 79]), but solid evidence supporting such a strategy is lacking [55] (suppl ref [80]).
Indications for future studies
Novel modulators of the hypermetabolic response should be tested in adequately powered studies, including patient-centered outcomes to assess safety and efficacy, rather than use of surrogate outcomes. Promising agents with the theoretical potential to stimulate protein synthesis or exert anti-catabolic effects include branched-chain amino acids, omega-3 fatty acids, metformin, β-blockers, oxandrolone, fenofibrate, and myostatin inhibitors, among others (suppl ref [66, 81]). Study design should consider the complexity of the metabolic response and specific clinical conditions and diseases. Biomarkers should be identified and validated to identify the optimal timing for increasing energy supply. Adequately powered RCTs should study optimal energy and protein targets independently, both in the acute phase and post-acute phase of critical illness, taking into consideration the dynamics of metabolism. Exercise potentially improves anabolic resistance (suppl ref [36]), providing the rationale for RCTs that integrate exercise and nutritional therapy (e.g., clinicaltrials.gov NCT02822170) (suppl ref [82]), include muscle strength and physical function as outcomes, and comprise mechanistic studies such as whole body protein kinetics, structural, molecular, and electrophysiological data.
ICUAW at follow-up
Weakness and fatigue
Background
Survivors of critical illness may suffer from prolonged muscle weakness and physical impairments [4–7, 10, 24, 56, 57]. In patients with significant weakness, sustained atrophy and decreased quadriceps voluntary contractile capacity can be demonstrated [57]. Physical dysfunction may persist longer than muscle weakness, and can be detected using dynamic tests such as the 6-min walk distance test or 4-m gait speed test [58] (suppl ref [83]) and physical activity monitoring [59].
Patients may not have any demonstrable weakness on examination, but may report having various degrees of perceived muscle weakness [4] or fatigue suggesting that a central mechanism may be responsible for weakness in addition to peripheral mechanisms. Fatigue is a common symptom in many medical conditions, including cancer, neurologic diseases, and psychiatric disorders (suppl ref [84–87]). The prevalence of fatigue is about 70% in ARDS survivors [50], and is often associated with anxiety and depression, pain, and cognitive impairments which are common in ICU survivors [1, 51, 60] (suppl ref [88]). Experimental endotoxemia in healthy humans causes transient weakness of voluntary quadriceps contraction, but leaves the electrically stimulated (nonvolitional) contraction unaffected (suppl ref [89]). In septic rats, disruption of repetitive firing of brain motor neurons is an important and early contributor to persistent weakness (suppl ref [90]).
Limits of current knowledge
It is uncertain if ICU survivors who feel weak despite having normal muscle strength have mild muscle weakness that is not detected by testing methods or if they have fatigue. It is also uncertain if fatigue can be diagnosed as systemic exertion intolerance disease (SEID) or chronic fatigue syndrome, a multisystem disorder with manifestations causing substantial morbidity and increased mortality [61] (suppl ref [91, 92]). A prominent feature of SEID is that any type of exertion—physical, cognitive, emotional—can adversely affect many organ systems and many aspects of life [61]. It is unknown if fatigue in ICU survivors could be caused by degeneration of nerve axons, as in survivors of Guillain–Barré syndrome where axonal loss is revealed by motor unit number estimation (MUNE), but not by clinical examination and conventional EPS that remain normal [62]. Lastly, the relationship between muscle weakness, fatigue, and psychiatric disorders remains to be elucidated. Exercise may improve depression in ICU survivors (suppl ref [93]), but the beneficial effect of treating depression on physical functioning in older adults (suppl ref [94]) has not been demonstrated yet in ICU survivors.
Indications for future studies
Further studies should evaluate the prevalence and severity of fatigue in ICU survivors, define its association with psychiatric disorders, pain, cognitive impairment, and other morbidities, and the relationship with muscle weakness and physical dysfunction [50]. Assessment of post-exertional physical, cognitive, and emotional exhaustion as in SEID should be studied in patients with profound fatigue. Studies should evaluate MUNE in patients with CIP. Rasagiline, modafinil, and doxepin are associated with improvement in fatigue and are not associated with an increased risk of adverse effects in patients with Parkinson disease [63], and should be studied in ICU populations. Collaborative care studies with multi-professional approach to patient care, structured management plan, scheduled patient follow-ups, and enhanced inter-professional communication are recommended for an integrated approach to patients with chronic mental and physical disorders (suppl ref [95, 96]), and would be needed to explore the efficacy of treatments for depression, weakness, and fatigue in ICU survivors.
Weakness, pain, and small nerve fiber pathology
Background
Persistent pain is a major problem in survivors of critical illness [64], and pain assessment in these patients was rated as “very important” in a recent expert consensus for physical rehabilitation in ICU survivors [33]. Of ICU survivors, 36–60% complain of moderate to severe pain which interferes with physical activity in daily life [64]. Causes include inadequately treated acute pain or degeneration of small intraepidermal nerve fibers (neuropathic pain) [65] (suppl ref [97, 98], decubitus ulcers [66], joint (shoulder) pathology [67], and fascial muscle inflammation [20] (Fig. 3).
Interplay between ICU-acquired weakness and pain. Bed rest with reduced mobility increases the risk of decubitus ulcers [56, 66], and also predicts weakness at long-term follow-up [56]. Decreased muscle tone may facilitate the instability of joins, particularly shoulder join, causing pain [67]. Loss of small intraepidermal nerve fibers [65] and fascial muscle inflammation [20] may cause pain, but their relationship with ICUAW needs further investigation
Limits of current knowledge
Small fiber pathology may cause chronic neuropathic pain [65] (suppl ref [99–101]), but its role in ICU survivors has been assessed in only a few patients.
Indications for future studies
Future studies should evaluate the relationship between ICUAW, reduced mobility, and chronic pain. The association between chronic neuropathic pain and degeneration of small intraepidermal nerve fibers during the acute stage of critical illness also deserves attention. Neuropathic pain can be severe and resistant to nonsteroidal anti-inflammatory drugs, so future efficacy trials should test if antidepressants (tryciclic antidepressants, serotonin-norepinephrine reuptake inhibitors), anticonvulsants (gabapentin, pregabalin), opioids, and lidocaine topical application can mitigate symptoms (suppl ref [102–105]). Skin biopsy is minimally invasive and can be repeated to follow the natural progression of disease and response to treatments (suppl ref [99, 100]). Future studies should evaluate muscle and fascial pain, and their relationship with qualitative inflammatory changes observed in the muscle [20].
Weakness and muscle pathology
Background
Muscle biopsy contributes to an understanding of the pathophysiology of myopathic changes by showing that early muscle fiber atrophy is associated with nonexcitable muscle membrane [68], decreased content [57, 69] and dysfunction [69] of satellite cells, mechanical silencing [70], altered muscle protein synthesis and degradation [18, 19, 52], aberrant expression of genes involved in muscle regeneration and repair [57] as well as mechanisms fueling muscle injury, and increased autophagy as protective mechanism [48]. In septic mice, engrafting mesenchymal stem cells decreases systemic inflammation, restores satellite cell function, and improves muscle strength [69]. Muscle biopsy also contributes to defining severity of weakness. Muscle necrosis, which is described in 40% of critically ill patients [18, 21] (suppl ref [4, 106–109]), is associated with a worse prognosis than loss of myosin filaments [2].
Limits of current knowledge
Mechanisms of poor muscle regeneration with persisting muscle atrophy in ICU survivors are poorly understood [57].
Indications for future studies
Skeletal muscle regeneration depends on stem (satellite) cells. Evaluation of satellite cell count and function in patients with persisting muscle atrophy and physical dysfunction compared to patients with good recovery would be important to better define the pathogenetic role of satellite cell dysfunction. Comprehensive mechanistic studies of muscle injury and repair are also needed.
Methodological issues for future research
Several methodological considerations arise in the study of ICUAW. Some have solutions developed in other fields while others are potentially unique, requiring new methodological research.
Accounting for baseline status
Baseline functional status of patients admitted to the ICU may be less than population norms. Therefore, investigators must exercise caution in attributing observed deficits to the ICU episode, especially in cohort studies with no control group. In large RCTs, investigators can rely on the likelihood that groups will be comparable at baseline, such that observed differences during follow-up can be attributed to the randomly assigned interventions. In non-random designs with control groups, investigators will need baseline measures, and can use a difference-in-differences analysis approach to understand how a given intervention affects the trajectory of ICUAW.
Accounting for missingness and censoring
Measures of weakness for a group of ICU patients will often be missing because the patient cannot participate in an evaluation or is lost to follow-up or has died. Such data loss is unlikely to occur randomly. There are techniques to handle both informative (non-random) and non-informative (random) missingness using various forms of imputation. Such techniques can also explore the extent to which missing information is or is not informative. For example, an inability to complete a physical strength assessment could itself be informative. Imputation methods or explicit modeling of the selection process likely help produce less biased estimates than those estimates generated from observed rates censored by non-random missingness. However, all analytic techniques deteriorate if missingness rates are high.
Generating and selecting measures
ICUAW can be considered at multiple levels, ranging from muscle cell function to muscle architecture and function, physical function, and, ultimately, the impact of physical dysfunction on activities and health-related quality of life. Similarly, the factors influencing these domains are protean. Not all factors can be captured in any one study, requiring researchers to decide which domains are most important on the basis of the aims of the study, the extent to which a particular measure can capture that domain with adequate fidelity, and the potential burden to patients, families, researchers, and clinicians posed by the execution of that measure. Since these measures must largely be deployed prospectively and many done in-person, researchers must factor this into the study design. Thus, a study assessing the speed of recovery of ICUAW may require frequent assessments, which may need to be brief. Another study, focused only on morbidities, may assess patients only once with a wider battery of tests.
Accounting for multiple outcomes and generating causal inference among multiple events
ICUAW has multiple plausible contributing, potentiating, and mitigating factors, and multiple interactions among biologic and clinical outcomes. For example, even if there was a specific somatic muscle lesion that drove ICUAW, it might be caused by many concurrent events during critical illness. The evolution of the lesion could be further influenced by intercurrent illness or drug and device use during the ICU. The subsequent outcomes could evolve differently depending on different underlying genetic predisposition, overall health status, capacity to engage in physical rehabilitation, and other post-ICU sequelae, which in turn could influence health and rehabilitation participation. Furthermore, the relationship between biologic outcomes (recovery of muscle architecture and function) and clinical outcomes (physical function and health-related quality of life) could vary depending on these other factors. These questions require datasets of adequate sample size (to account for representation of the different factors described above) and adequate clinical and biologic detail (to measure these factors properly) and analytic techniques capable of modeling potential relationships between these factors, including the generation of potential causal links (suppl ref [110]).
References
Stevens R, Hart N, Herridge M (2014) Textbook of post-ICU medicine: the legacy of critical care. Oxford University Press, Oxford
Latronico N, Bolton CF (2011) Critical illness polyneuropathy and myopathy: a major cause of muscle weakness and paralysis. Lancet Neurol 10:931–941
Fan E, Cheek F, Chlan L, Gosselink R, Hart N, Herridge MS, Hopkins RO, Hough CL, Kress JP, Latronico N, Moss M, Needham DM, Rich MM, Stevens RD, Wilson KC, Winkelman C, Zochodne DW, Ali NA, ATS Committee on ICU-acquired Weakness in Adults, American Thoracic Society (2014) An official American Thoracic Society clinical practice guideline: the diagnosis of intensive care unit-acquired weakness in adults. Am J Respir Crit Care Med 190:1437–1446
Herridge MS, Tansey CM, Matte A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM (2011) Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 364:1293–1304
Pfoh ER, Wozniak AW, Colantuoni E, Dinglas VD, Mendez-Tellez PA, Shanholtz C, Ciesla ND, Pronovost PJ, Needham DM (2016) Physical declines occurring after hospital discharge in ARDS survivors: a 5-year longitudinal study. Intensive Care Med 42:1557–1566
Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM (2015) Functional trajectories among older persons before and after critical illness. JAMA Intern Med 175:523–529
Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM (2016) Factors associated with functional recovery among older intensive care unit survivors. Am J Respir Crit Care Med 194:299–307
Puthucheary ZA, Denehy L (2015) Exercise interventions in critical illness survivors: understanding inclusion and stratification criteria. Am J Respir Crit Care Med 191:1464–1467
Zampieri FG, Bozza FA, Moralez GM, Mazza DD, Scotti AV, Santino MS, Ribeiro RA, Rodrigues Filho EM, Cabral MM, Maia MO, D’Alessandro PS, Oliveira SV, Menezes MA, Caser EB, Lannes RS, Alencar Neto MS, Machado MM, Sousa MF, Salluh JI, Soares M (2017) The effects of performance status one week before hospital admission on the outcomes of critically ill patients. Intensive Care Med 43:39–47
Herridge MS, Chu LM, Matte A, Tomlinson G, Chan L, Thomas C, Friedrich JO, Mehta S, Lamontagne F, Levasseur M, Ferguson ND, Adhikari NK, Rudkowski JC, Meggison H, Skrobik Y, Flannery J, Bayley M, Batt J, Santos CD, Abbey SE, Tan A, Lo V, Mathur S, Parotto M, Morris D, Flockhart L, Fan E, Lee CM, Wilcox ME, Ayas N, Choong K, Fowler R, Scales DC, Sinuff T, Cuthbertson BH, Rose L, Robles P, Burns S, Cypel M, Singer L, Chaparro C, Chow CW, Keshavjee S, Brochard L, Hebert P, Slutsky AS, Marshall JC, Cook D, Cameron JI, Investigators RP, Canadian Critical Care Trials Group (2016) The RECOVER program: disability risk groups and 1-year outcome after 7 or more days of mechanical ventilation. Am J Respir Crit Care Med 194:831–844
Prescott HC, Osterholzer JJ, Langa KM, Angus DC, Iwashyna TJ (2016) Late mortality after sepsis: propensity matched cohort study. BMJ 353:i2375
Iwashyna TJ (2012) Trajectories of recovery and dysfunction after acute illness, with implications for clinical trial design. Am J Respir Crit Care Med 186:302–304
Iwashyna TJ, Hodgson CL, Pilcher D, Bailey M, van Lint A, Chavan S, Bellomo R (2016) Timing of onset and burden of persistent critical illness in Australia and New Zealand: a retrospective, population-based, observational study. Lancet Respir Med 4:566–573
Iwashyna TJ, Netzer G, Langa KM, Cigolle C (2012) Spurious inferences about long-term outcomes: the case of severe sepsis and geriatric conditions. Am J Respir Crit Care Med 185:835–841
Barnato AE, Albert SM, Angus DC, Lave JR, Degenholtz HB (2011) Disability among elderly survivors of mechanical ventilation. Am J Respir Crit Care Med 183:1037–1042
Batt J, dos Santos CC, Cameron JI, Herridge MS (2013) Intensive care unit-acquired weakness: clinical phenotypes and molecular mechanisms. Am J Respir Crit Care Med 187:238–246
Connolly B, MacBean V, Crowley C, Lunt A, Moxham J, Rafferty GF, Hart N (2015) Ultrasound for the assessment of peripheral skeletal muscle architecture in critical illness: a systematic review. Crit Care Med 43:897–905
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, Hopkinson NS, Padhke R, Dew T, Sidhu PS, Velloso C, Seymour J, Agley CC, Selby A, Limb M, Edwards LM, Smith K, Rowlerson A, Rennie MJ, Moxham J, Harridge SD, Hart N, Montgomery HE (2013) Acute skeletal muscle wasting in critical illness. JAMA 310:1591–1600
Wollersheim T, Woehlecke J, Krebs M, Hamati J, Lodka D, Luther-Schroeder A, Langhans C, Haas K, Radtke T, Kleber C, Spies C, Labeit S, Schuelke M, Spuler S, Spranger J, Weber-Carstens S, Fielitz J (2014) Dynamics of myosin degradation in intensive care unit-acquired weakness during severe critical illness. Intensive Care Med 40:528–538
Puthucheary ZA, Phadke R, Rawal J, McPhail MJ, Sidhu PS, Rowlerson A, Moxham J, Harridge S, Hart N, Montgomery HE (2015) Qualitative ultrasound in acute critical illness muscle wasting. Crit Care Med 43:1603–1611
Latronico N (2016) Critical illness polyneuropathy and myopathy 20 years later. No manʼs land? No, it is our land! Intensive Care Med 42:1790–1793
Hermans G, Van Mechelen H, Bruyninckx F, Vanhullebusch T, Clerckx B, Meersseman P, Debaveye Y, Casaer MP, Wilmer A, Wouters PJ, Vanhorebeek I, Gosselink R, Van den Berghe G (2015) Predictive value for weakness and 1-year mortality of screening electrophysiology tests in the ICU. Intensive Care Med 41:2138–2148
Latronico N, Nattino G, Guarneri B, Fagoni N, Amantini A, Bertolini G, GiVITI Study Investigators (2014) Validation of the peroneal nerve test to diagnose critical illness polyneuropathy and myopathy in the intensive care unit: the multicentre Italian CRIMYNE-2 diagnostic accuracy study. F1000Res 3:127
Needham DM, Wozniak AW, Hough CL, Morris PE, Dinglas VD, Jackson JC, Mendez-Tellez PA, Shanholtz C, Ely EW, Colantuoni E, Hopkins RO, National Institutes of Health NHLBI ARDS Network (2014) Risk factors for physical impairment after acute lung injury in a national, multicenter study. Am J Respir Crit Care Med 189:1214–1224
Weber-Carstens S, Schneider J, Wollersheim T, Assmann A, Bierbrauer J, Marg A, Al Hasani H, Chadt A, Wenzel K, Koch S, Fielitz J, Kleber C, Faust K, Mai K, Spies CD, Luft FC, Boschmann M, Spranger J, Spuler S (2013) Critical illness myopathy and GLUT4: significance of insulin and muscle contraction. Am J Respir Crit Care Med 187:387–396
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373:1874–1882
Hodgson CL, Bailey M, Bellomo R, Berney S, Buhr H, Denehy L, Gabbe B, Harrold M, Higgins A, Iwashyna TJ, Papworth R, Parke R, Patman S, Presneill J, Saxena M, Skinner E, Tipping C, Young P, Webb S, Trial of Early Activity and Mobilization Study Investigators (2016) A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in the ICU. Crit Care Med 44:1145–1152
Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, Heim M, Houle T, Kurth T, Latronico N, Lee J, Meyer MJ, Peponis T, Talmor D, Velmahos GC, Waak K, Walz JM, Zafonte R, Eikermann M, International Early SOMS-guided Mobilization Research Initiative (2016) Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 388:1377–1388
Denehy L, Skinner EH, Edbrooke L, Haines K, Warrillow S, Hawthorne G, Gough K, Hoorn SV, Morris ME, Berney S (2013) Exercise rehabilitation for patients with critical illness: a randomized controlled trial with 12 months of follow-up. Crit Care 17:R156
Moss M, Nordon-Craft A, Malone D, Van Pelt D, Frankel SK, Warner ML, Kriekels W, McNulty M, Fairclough DL, Schenkman M (2016) A randomized trial of an intensive physical therapy program for patients with acute respiratory failure. Am J Respir Crit Care Med 193:1101–1110
Morris PE, Berry MJ, Files DC, Thompson JC, Hauser J, Flores L, Dhar S, Chmelo E, Lovato J, Case LD, Bakhru RN, Sarwal A, Parry SM, Campbell P, Mote A, Winkelman C, Hite RD, Nicklas B, Chatterjee A, Young MP (2016) Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: a randomized clinical trial. JAMA 315:2694–2702
Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL (2016) The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med 18:1–3
Major ME, Kwakman R, Kho ME, Connolly B, McWilliams D, Denehy L, Hanekom S, Patman S, Gosselink R, Jones C, Nollet F, Needham DM, Engelbert RH, van der Schaaf M (2016) Surviving critical illness: what is next? An expert consensus statement on physical rehabilitation after hospital discharge. Crit Care 20:354
Dres M, Dube BP, Mayaux J, Delemazure J, Reuter D, Brochard L, Similowski T, Demoule A (2017) Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med 195:57–66
Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, Rittayamai N, Lanys A, Tomlinson G, Singh JM, Bolz SS, Rubenfeld GD, Kavanagh BP, Brochard LJ, Ferguson ND (2015) Evolution of diaphragm thickness during mechanical ventilation. Impact of inspiratory effort. Am J Respir Crit Care Med 192:1080–1088
Spadaro S, Grasso S, Mauri T, Dalla Corte F, Alvisi V, Ragazzi R, Cricca V, Biondi G, Di Mussi R, Marangoni E, Volta CA (2016) Can diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? The role of diaphragmatic rapid shallow breathing index. Crit Care 20:305
Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrillo A (2017) Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med 43:29–38
Medrinal C, Prieur G, Frenoy E, Robledo Quesada A, Poncet A, Bonnevie T, Gravier FE, Lamia B, Contal O (2016) Respiratory weakness after mechanical ventilation is associated with one-year mortality—a prospective study. Crit Care 20:231
Martin AD, Smith BK, Davenport PD, Harman E, Gonzalez-Rothi RJ, Baz M, Layon AJ, Banner MJ, Caruso LJ, Deoghare H, Huang TT, Gabrielli A (2011) Inspiratory muscle strength training improves weaning outcome in failure to wean patients: a randomized trial. Crit Care 15:R84
Bissett BM, Leditschke IA, Neeman T, Boots R, Paratz J (2016) Inspiratory muscle training to enhance recovery from mechanical ventilation: a randomised trial. Thorax 71:812–819
Macht M, Wimbish T, Bodine C, Moss M (2013) ICU-acquired swallowing disorders. Crit Care Med 41:2396–2405
Prescott HC, Langa KM, Iwashyna TJ (2015) Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA 313:1055–1057
Mayr FB, Talisa VB, Balakumar V, Chang CH, Fine M, Yende S (2017) Proportion and cost of unplanned 30-day readmissions after sepsis compared with other medical conditions. JAMA 317(5):530–531
Doorduin J, van Hees HW, van der Hoeven JG, Heunks LM (2013) Monitoring of the respiratory muscles in the critically ill. Am J Respir Crit Care Med 187:20–27
Brodsky MB, Suiter DM, Gonzalez-Fernandez M, Michtalik HJ, Frymark TB, Venediktov R, Schooling T (2016) Screening accuracy for aspiration using bedside water swallow tests: a systematic review and meta-analysis. Chest 150:148–163
Morandi A, Rogers BP, Gunther ML, Merkle K, Pandharipande P, Girard TD, Jackson JC, Thompson J, Shintani AK, Geevarghese S, Miller RR 3rd, Canonico A, Cannistraci CJ, Gore JC, Ely EW, Hopkins RO, VISIONS Investigation, VISualizing Icu SurvivOrs Neuroradiological Sequelae (2012) The relationship between delirium duration, white matter integrity, and cognitive impairment in intensive care unit survivors as determined by diffusion tensor imaging: the VISIONS prospective cohort magnetic resonance imaging study. Crit Care Med 40:2182–2189
Van den Berghe G (2016) On the neuroendocrinopathy of critical illness. Perspectives for feeding and novel treatments. Am J Respir Crit Care Med 194:1337–1348
Hermans G, Casaer MP, Clerckx B, Guiza F, Vanhullebusch T, Derde S, Meersseman P, Derese I, Mesotten D, Wouters PJ, Van Cromphaut S, Debaveye Y, Gosselink R, Gunst J, Wilmer A, Van den Berghe G, Vanhorebeek I (2013) Effect of tolerating macronutrient deficit on the development of intensive-care unit acquired weakness: a subanalysis of the EPaNIC trial. Lancet Respir Med 1:621–629
Doig GS, Simpson F, Sweetman EA, Finfer SR, Cooper DJ, Heighes PT, Davies AR, O’Leary M, Solano T, Peake S, Early PN Investigators of the ANZICS Clinical Trials Group (2013) Early parenteral nutrition in critically ill patients with short-term relative contraindications to early enteral nutrition: a randomized controlled trial. JAMA 309:2130–2138
Needham DM, Dinglas VD, Bienvenu OJ, Colantuoni E, Wozniak AW, Rice TW, Hopkins RO, NIH NHLBI ARDS Network (2013) One year outcomes in patients with acute lung injury randomised to initial trophic or full enteral feeding: prospective follow-up of EDEN randomised trial. BMJ 346:f1532
Needham DM, Dinglas VD, Morris PE, Jackson JC, Hough CL, Mendez-Tellez PA, Wozniak AW, Colantuoni E, Ely EW, Rice TW, Hopkins RO (2013) Physical and cognitive performance of patients with acute lung injury 1 year after initial trophic versus full enteral feeding. EDEN trial follow-up. Am J Respir Crit Care Med 188:567–576
Derde S, Hermans G, Derese I, Guiza F, Hedstrom Y, Wouters PJ, Bruyninckx F, D’Hoore A, Larsson L, Van den Berghe G, Vanhorebeek I (2012) Muscle atrophy and preferential loss of myosin in prolonged critically ill patients. Crit Care Med 40:79–89
Arabi YM, Aldawood AS, Haddad SH, Al-Dorzi HM, Tamim HM, Jones G, Mehta S, McIntyre L, Solaiman O, Sakkijha MH, Sadat M, Afesh L, Permi TTG (2015) Permissive underfeeding or standard enteral feeding in critically ill adults. N Engl J Med 372:2398–2408
Arabi YM, Aldawood AS, Al-Dorzi HM, Tamim HM, Haddad SH, Jones G, McIntyre L, Solaiman O, Sakkijha MH, Sadat M, Mundekkadan S, Kumar A, Bagshaw SM, Mehta S, Permi TTG (2016) Permissive underfeeding or standard enteral feeding in high and low nutritional risk critically ill adults: post-hoc analysis of the permit trial. Am J Respir Crit Care Med 372(25):2398–2408
Ferrie S, Allman-Farinelli M, Daley M, Smith K (2016) Protein requirements in the critically ill: a randomized controlled trial using parenteral nutrition. JPEN J Parenter Enteral Nutr 40:795–805
Fan E, Dowdy DW, Colantuoni E, Mendez-Tellez PA, Sevransky JE, Shanholtz C, Himmelfarb CR, Desai SV, Ciesla N, Herridge MS, Pronovost PJ, Needham DM (2014) Physical complications in acute lung injury survivors: a 2-year longitudinal prospective study. Crit Care Med 42:849–859
Dos Santos C, Hussain SN, Mathur S, Picard M, Herridge M, Correa J, Bain A, Guo Y, Advani A, Advani SL, Tomlinson G, Katzberg H, Streutker CJ, Cameron JI, Schols A, Gosker HR, Batt J, Group MI, Investigators RP, Canadian Critical Care Translational Biology Group (2016) Mechanisms of chronic muscle wasting and dysfunction after an intensive care unit stay: a pilot study. Am J Respir Crit Care Med 194:821–830
Chan KS, Aronson Friedman L, Dinglas VD, Hough CL, Morris PE, Mendez-Tellez PA, Jackson JC, Ely EW, Hopkins RO, Needham DM (2016) Evaluating physical outcomes in acute respiratory distress syndrome survivors: validity, responsiveness, and minimal important difference of 4-meter gait speed test. Crit Care Med 44:859–868
McNelly AS, Rawal J, Shrikrishna D, Hopkinson NS, Moxham J, Harridge SD, Hart N, Montgomery HE, Puthucheary ZA (2016) An exploratory study of long-term outcome measures in critical illness survivors: construct validity of physical activity, frailty, and health-related quality of life measures. Crit Care Med 44:e362–e369
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, Brummel NE, Hughes CG, Vasilevskis EE, Shintani AK, Moons KG, Geevarghese SK, Canonico A, Hopkins RO, Bernard GR, Dittus RS, Ely EW, BRAIN-ICU Study Investigators (2013) Long-term cognitive impairment after critical illness. N Engl J Med 369:1306–1316
Clayton EW (2015) Beyond myalgic encephalomyelitis/chronic fatigue syndrome: an IOM report on redefining an illness. JAMA 313:1101–1102
Drenthen J, Jacobs BC, Maathuis EM, van Doorn PA, Visser GH, Blok JH (2013) Residual fatigue in Guillain-Barre syndrome is related to axonal loss. Neurology 81:1827–1831
Elbers RG, Berendse HW, Kwakkel G (2016) Treatment of fatigue in Parkinson disease. JAMA 315:2340–2341
Baumbach P, Gotz T, Gunther A, Weiss T, Meissner W (2016) Prevalence and characteristics of chronic intensive care-related pain: the role of severe sepsis and septic shock. Crit Care Med 44:1129–1137
Latronico N, Filosto M, Fagoni N, Gheza L, Guarneri B, Todeschini A, Lombardi R, Padovani A, Lauria G (2013) Small nerve fiber pathology in critical illness. PLoS One 8:e75696
Eachempati SR, Hydo LJ, Barie PS (2001) Factors influencing the development of decubitus ulcers in critically ill surgical patients. Crit Care Med 29:1678–1682
Battle CE, Lovett S, Hutchings H (2013) Chronic pain in survivors of critical illness: a retrospective analysis of incidence and risk factors. Crit Care 17:R101
Bierbrauer J, Koch S, Olbricht C, Hamati J, Lodka D, Schneider J, Luther-Schroder A, Kleber C, Faust K, Wiesener S, Spies CD, Spranger J, Spuler S, Fielitz J, Weber-Carstens S (2012) Early type II fiber atrophy in intensive care unit patients with nonexcitable muscle membrane. Crit Care Med 40:647–650
Rocheteau P, Chatre L, Briand D, Mebarki M, Jouvion G, Bardon J, Crochemore C, Serrani P, Lecci PP, Latil M, Matot B, Carlier PG, Latronico N, Huchet C, Lafoux A, Sharshar T, Ricchetti M, Chretien F (2015) Sepsis induces long-term metabolic and mitochondrial muscle stem cell dysfunction amenable by mesenchymal stem cell therapy. Nat Commun 6:10145
Corpeno Kalamgi R, Salah H, Gastaldello S, Martinez-Redondo V, Ruas JL, Fury W, Bai Y, Gromada J, Sartori R, Guttridge DC, Sandri M, Larsson L (2016) Mechano-signalling pathways in an experimental intensive critical illness myopathy model. J Physiol 594:4371–4388
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Latronico, N., Herridge, M., Hopkins, R.O. et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med 43, 1270–1281 (2017). https://doi.org/10.1007/s00134-017-4757-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-017-4757-5