Abstract
Background
The goal of this study was to assess the impact of prone positioning on the incidence of ventilator-associated pneumonia (VAP) and the role of VAP in mortality in a recent multicenter trial performed on patients with severe ARDS.
Methods
An ancillary study of a prospective multicenter randomized controlled trial on early prone positioning in patients with severe ARDS. In suspected cases of VAP the diagnosis was based on positive quantitative cultures of bronchoalveolar lavage fluid or tracheal aspirate at the 104 and 107 CFU/ml thresholds, respectively. The VAP cases were then subject to central, independent adjudication. The cumulative probabilities of VAP were estimated in each position group using the Aalen–Johansen estimator and compared using Gray’s test. A univariate and a multivariate Cox model was performed to assess the impact of VAP, used as a time-dependent covariate for mortality hazard during the ICU stay.
Results
In the supine and prone position groups, the incidence rate for VAP was 1.18 (0.86–1.60) and 1.54 (1.15–2.02) per 100 days of invasive mechanical ventilation (p = 0.10), respectively. The cumulative probability of VAP at 90 days was estimated at 46.5 % (27–66) in the prone group and at 33.5 % (23–44) in the supine group. The difference between the two cumulative probability curves was not statistically significant (p = 0.11). In the univariate Cox model, VAP was associated with an increase in the mortality rate during the ICU stay [HR 1.65 (1.05–2.61), p = 0.03]. HR increased to 2.2 (1.39–3.52) (p < 0.001) after adjustment for position group, age, SOFA score, McCabe score, and immunodeficiency.
Conclusions
In severe ARDS patients prone positioning did not reduce the incidence of VAP and VAP was associated with higher mortality.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is a complex condition [1] with a high mortality rate [2]. Ventilator-associated pneumonia (VAP) may complicate the outcome of ARDS and is difficult to diagnose. The morbidity and mortality rates associated with VAP are high [3] but the issue of whether or not VAP is associated with mortality in ARDS patients is still a matter of debate. In their meta-analysis of four observational studies conducted on ARDS patients, Melsen et al. concluded that this association was not significant contrary to other settings [4]. However, this result pertained to studies done before the era of lung protective mechanical ventilation, and notably the use of lower tidal volume [5]. Since then, Forel et al. have reanalyzed the results of a placebo-controlled trial on neuromuscular blockade in which ARDS patients benefited from a lung protective strategy. They found that VAP occurred in almost one-third of patients but the results of the analysis did not support a significant association between VAP and mortality [6]. Furthermore, this trial was carried out on patients with severe ARDS and demonstrated outcome benefits from the use of neuromuscular blockade. A significant improvement in survival from using the prone position, as compared to the supine position, was found in a trial that combined the use of a lung protective strategy and neuromuscular blockade in patients with severe ARDS [7]. This trial included an ancillary study specifically dedicated to VAP and the relevant data were prospectively collected for both the supine and prone groups [8]. Therefore, the present report addresses the following questions: (1) does prone positioning affect the incidence of VAP, and hence could prone positioning be used as a strategy to prevent VAP in severe ARDS and could VAP prevention be a mechanism by which prone positioning improves patient outcomes? (2) Is there a significant relationship between VAP and mortality in these patients? Our primary hypothesis was that the prone position is associated with a reduction in VAP incidence. In addition to the fact that expelling respiratory secretions is enhanced in the prone position, a mechanism by which prone positioning reduces VAP, we based our hypothesis on two tenets. The first was that in our first trial in all-comer patients with acute hypoxemic respiratory failure, the prone position was associated with a reduction in the incidence of VAP per 100 days of mechanical ventilation [9]. The second was that in our last trial in patients with severe ARDS survival was significantly improved by prone positioning, and the reduction in VAP might have contributed to this improvement [7].
Patients and methods
Inclusion criteria
We included adults (18 years or older), endotracheally intubated for ARDS [10], ongoing for the previous 36 h, with severity criteria (PaO2/fraction of inspired oxygen (FiO2) <150 mmHg under FiO2 ≥ 0.6, positive end-expiratory pressure (PEEP) ≥5 cmH2O, and tidal volume (VT) = 6 ml/kg predicted body weight) fulfilled after a 12–24 h stabilization period, and for whom the next of kin gave their consent to participate [7].
Non-inclusion criteria
Patients were not included in the trial either because of contraindications to proning, or respiratory treatments or specific clinical settings, or for other reasons, all of which are detailed in the ESM.
Body positioning
Patients allocated to the prone group were put into the prone position within the hour after randomization for at least 16 consecutive hours until predetermined stopping criteria were met. Patients in the supine group were installed in the semirecumbent position. Both groups were identically managed in terms of lung protective mechanical ventilation, using 6 ml/kg predicted body weight tidal volume [5], neuromuscular blockade and sedation, and weaning from mechanical ventilation.
Ventilator-associated pneumonia diagnosis and management
VAP was suspected if, at least 48 h after inclusion, features suggesting pneumonia were found on the daily chest X-ray in association with a new occurrence of hyperthermia >38 °C with no other obvious cause or a neutrophil count <4000 or >12,000 GB/mm3, and at least one of the following criteria: purulent secretions, cough or dyspnea or tachypnea, suggestive auscultation, deterioration in arterial blood gas levels.
The above criteria were checked on a daily basis by the investigator in charge of the protocol in each center. Once these criteria were present respiratory secretions were sampled using either Wimberley brush or protected distal sampling, or bronchoalveolar lavage (BAL) or tracheal aspirates, according to the routine practice in each center. The diagnosis of VAP was established if at least one microorganism grew in concentration ≥103 or ≥104 or ≥107 colony forming units (CFU/ml), according to the previously mentioned diagnostic tool. The day of VAP was therefore the day on which the lung sample tested positive.
The overall antibiotic therapy strategy in patients with suspected VAP might be to start after lung sampling, but before the results are received (empiric antibiotic therapy) or after the partial results are received (such as direct examination of the sample). Empiric antibiotic therapy can be reassessed after the full results from the lung sample specimens are received, including antibiotic susceptibility.
Data collection
Demographic data were collected on ICU admission. From inclusion to day 28, the ventilator settings, physiological variables, relevant co-interventions and medications were collected daily. Once the diagnosis of the first episode of VAP was made, a specific sheet included in the case report form for the PROSEVA trial was filled out for the following items: the diagnostic procedure for lung sampling, antibiotic therapy (empiric or reassessed after the results of the lung cultures), results of the lung cultures, duration of antibiotic therapy. Patients were assessed for survival or death at the time of ICU discharge, day 28 and 90, the length of ICU stay, and the time spent under invasive mechanical ventilation.
Data analysis
Central adjudication of VAP cases
The first episode of VAP was recorded in the patient case record form by the investigator in charge of the protocol in each center. The date and results of the bacteriological sampling, the date of intubation, and the nature of the antibiotic therapy were reported in a specific form filled out by the coordinating research fellow and sent to an intensivist abroad who was not involved in the trial (Didier Tassaux, MD, Intensive Care Unit, Geneva University Hospital, Geneva, Switzerland) for the central adjudication of the VAP cases. His task was to confirm the diagnosis of VAP and to assess the appropriateness of the antibiotic therapy on the basis of American Thoracic Society (ATS) recommendations [11]. At the time of this assessment, the adjudicator was blinded to the patient’s position group. Furthermore, the adjudication was not communicated to the clinician responsible for the patient.
In order to investigate the first objective, we measured the incidence of the first episode of VAP. In order to investigate the second objective, we measured the fatality rate during the ICU stay up to 90 days after randomization. For both patients with and without VAP we also described the number of days free from ventilator support, the duration of the ICU stay, the duration of organ failure, and the appropriateness of the antibiotic therapy.
The quantitative characteristics of patients were described using their mean values and standard deviation or their median values together with the first and third quartiles. The qualitative characteristics were described using the absolute and relative frequency in each category. The quantitative characteristics were compared using the Student t test or the Mann–Whitney non-parametric test. The qualitative characteristics were compared using the Chi square test or the Fisher exact test as required.
The incidence rate of VAP was calculated as the number of first episodes of VAP divided by the cumulative number of days of intubation for the patients without VAP and up to the date of the first episode of VAP for the other patients. It was estimated along with its 95 % confidence interval for the entire cohort and for each position group. The comparison between the two groups was made using the Z-score test.
In order to analyze the impact of prone positioning on the risk of VAP taking into account the competing risk corresponding to death, the cumulative probabilities of VAP were estimated for each position group using the Aalen–Johansen estimator [9]. Gray’s test was used to compare the two curves of cumulative probabilities [10].
In order to analyze the impact of VAP on the mortality rate during the ICU stay we used a Cox model in which VAP was introduced as a time-dependent covariate. In this analysis the observations were censored at the time of ICU discharge or at 90 days. The univariate Cox model was built first. Then, the effect of the VAP was adjusted for age, SOFA score at the time of inclusion, McCabe score, and immunodeficiency, which are well-known predictors of mortality, and also for the position group in a multivariate Cox model. Furthermore, two adjusted multivariate Cox models were explored, one with and one without interaction between VAP and the position group.
The statistical significant threshold was set to p < 0.05; p values were reported as two-sided. The statistical analysis was performed using SPSS (IBM SPSS statistics 19.0, SPSS inc.), R, version 3.1.3 (R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, URL http://www.R-project.org), and Open Epi software.
Results
VAP incidence
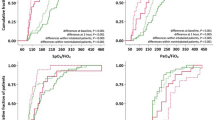
From 1 January 2008 to 25 July 2011, 466 patients with severe ARDS were analyzed in the PROSEVA trial in an intention-to-treat fashion, 229 in the supine and 237 in the prone group. A first episode of VAP was observed in 93 patients (20 %) after the central adjudication process. The incidence rate of VAP was therefore 1.35 [95 % confidence interval (1.09–1.66)] per 100 days of invasive mechanical ventilation. In the univariate comparison, male gender and use of neuromuscular blockade were observed more frequently in patients with VAP than those without (Table 1). The median time to VAP from intubation was 12 (7–19) days. In the supine and prone groups, first episodes of VAP occurred in 41 and 52 patients, respectively, and hence the corresponding attack rates were 17.9 and 22.8 % (p = 0.19). For the incidence rates per 100 days of invasive mechanical ventilation they were 1.18 (0.858–1.60) and 1.54 (1.15–2.02), respectively, in the supine and prone groups (p = 0.10). The cumulative probability of VAP was higher in the prone than in the supine position group (Fig. 1), but the difference did not reach statistical significance (p = 0.11). The cumulative probability of VAP was estimated as 46.5 % at 90 days in the prone position group (27–66) and 33.5 % in the supine position group (23–44 %).
VAP diagnosis
In 23 cases the VAP diagnosis made by the clinician was not confirmed by the adjudicator, with no difference between the supine and prone groups (10 vs 13 %, i.e., 4.4 vs 5.5 %, p = 0.58). Fiberoptic BAL and tracheal aspirates were used in 66 and 27 patients, respectively. For the purposes of the VAP diagnosis, 112 strains were retrieved (Table 2 ESM) with no statistical difference in the distribution of the strains across the supine and the prone groups (not shown). The most common microorganism was Pseudomonas aeruginosa (Table 2 ESM).
Antibiotic therapy for VAP management
In 91.4 % of the VAP cases (85/93) antibiotic therapy was started empirically, i.e., immediately after lung sampling and was appropriate in 81.7 % of cases (76/93), with no difference between the supine and prone groups. The antibiotic therapy was reassessed after receipt of the lung culture results in 51.6 % (48/93) of cases and was then appropriate in 94.6 % (88/93), again with no difference between the supine and prone groups. The total duration of antibiotic therapy for VAP averaged 10 ± 5 days over all patients with VAP. It was 10 ± 6 days in patients who died, and 11 ± 4 days in those who were alive at the time of ICU discharge (p = 0.45).
Mortality
The proportion of patients amongst those who developed VAP during the ICU stay who died was 33.3 (31/93) and 25.5 % (95/373) for those who did not develop VAP (p = 0.28). The median time to death from VAP diagnosis was 14.5 (5–24) days. In the univariate Cox model, VAP was associated with an increase in the mortality rate during the ICU stay [hazard ratio (HR) 1.65 (1.05–2.61) (p = 0.03)].
After adjustment for confounding factors, the VAP HR increased to 2.21 (1.39–3.52) (Table 2). The position group, age, and SOFA score at the time of ICU admission were other predictors significantly associated with mortality during the ICU stay. The results were essentially the same when interaction between VAP and the position group was taken into account (Table 2).
Finally, the number of ICU-free days was significantly greater in patients without VAP as compared to those with VAP, whilst the opposite was true for the number of organ failure-free days (Table 3).
Discussion
In the present study of patients with severe ARDS included in the PROSEVA trial, we observed that (1) the cumulative incidence of VAP was greater in the prone as opposed to the supine group, but this difference was not statistically significant, (2) the mortality rate during the ICU stay was significantly higher in association with VAP.
The incidence rate of VAP was not significantly different between the prone and the supine position groups, a result which contradicts our initial hypothesis. However, we cannot definitively conclude that there is an absence of a true difference on the basis of this result. The cumulative incidence of VAP at 90 days is 46.5 % in the prone group vs 33.5 % in the supine group, which is a marked effect size. From this finding, we cannot argue that the prone position can reduce the incidence of VAP in ARDS patients. This can be partly explained by the lower mortality in the prone group. In the meta-analysis by Sud et al. [12] the relative risk for the VAP attack rate was 0.81 (0.66–0.99) in favor of the prone position group (p = 0.04). Even though the statistical heterogeneity was not significant (I 2 = 0 %), the fact that the diagnostic techniques for VAP were not standardized across centers and the assessors were not blinded were factors that may limit the generalizability of the results. In comatose patients without ARDS, Beuret et al. found that a short course of prone positioning was associated with a lower incidence of VAP [13]. In a prospective non-interventional study Mounier et al. found that prone positioning had no impact on the incidence of VAP in patients with hypoxemic respiratory failure receiving invasive mechanical ventilation in the ICU [14].
In the reference paper by Cook et al. [15] the incidence of VAP was 1.48/100 days of mechanical ventilation, a rate very close to the present results. The time of occurrence of VAP in patients with severe ARDS is likely to be different from a general ICU population. Some reasons for this are discussed below. The drainage of respiratory secretions, commonly observed in the prone position, is one mechanism by which proning could reduce VAP. In our previous trial on prone positioning, we found a significant reduction in the incidence of VAP in the prone position group, whilst the attack rate was similar [9]. The difference regarding the incidence of VAP between our present and previous trials may also reflect differences in the patient population. Indeed, in the previous trial, all-comer patients with hypoxemic acute respiratory failure were included, in particular patients with chronic obstructive pulmonary disease. It should be mentioned that in more than 50 % of patients included in the trial, the cause of ARDS was pneumonia. The presence of pneumonia as the cause of ARDS makes the diagnosis of a new episode of pneumonia even more difficult (non-resolving ARDS or relapsing pneumonia versus a new episode of pneumonia). With such a high number of cases in the cohort of ARDS caused by pneumonia, there is a risk that some cases of non-resolving or relapsing pneumonia have been characterized as first episodes of VAP. However, the 20 % attack rate for the first episode of VAP in the present study compares to that of 29 % found in similar patients by Forel et al. [6]. It was also close to that found in all-comer ICU patients in European ICUs, which was 19 % (465/2436 patients evaluated) [16]. The incidence of VAP in the specific subset of ARDS patients was not mentioned in that study [16]. P. aeruginosa was the most frequent microorganism involved in VAP in line with the current literature [17].
The relationship between VAP and mortality is a complex issue. We found that the rate of death during the ICU stay was 33.3 % in patients with VAP and 25.5 % in patients with no VAP. The greater rate of death in patients with VAP was not statistically significantly different from that in patients without VAP. However, this result is subject to misinterpretation because VAP is not treated as a time-dependent variable. Patients with VAP should have been included in the no VAP group until VAP occurred and then moved into the VAP group. By performing an analysis that treats VAP as a time-dependent covariate, we found a significant association between VAP occurrence and the risk of death during the ICU stay. The result was even more significant when confounding factors were taken into account. However, our analysis, which managed VAP as a time-dependent covariate, found that VAP was a significant predictor of death. Our result does not correspond to previous findings. A large cohort study of over 4479 ICU patients, of which 685 developed VAP, showed that the VAP-attributable ICU mortality was marginal amounting to 1 % [18]. Furthermore, Forel et al. [6] found that VAP was not a significant predictor of death in ARDS patients very similar to those included in the present study.
The present result underlines the importance of implementing measures for VAP prevention in settings where patients with severe ARDS are offered prone positioning.
We found that the number of organ failure-free days was greater in patients with VAP. We have no explanation for this finding. It should be stressed that this result is subject to misinterpretation because VAP is not treated as a time-dependent variable as previously discussed. The diagnosis of VAP in this study was mostly assessed using invasive techniques, notably fiberoptic-directed BAL [19] (71 % of the procedures). A prospective observational study performed in 27 European ICUs of 465 cases of VAP found that fiberoptic BAL accounted for 13.6 % of VAP diagnoses [16], with no mention of the ARDS subgroup.
Limitations and strengths
The present study has limitations. The main limitation is that we did not assess VAP risk factors after inclusion, unlike the study by Forel et al. [6]. In the latter, the risk factors recorded at the time of inclusion were male gender and Glasgow coma score on admission but these were further expanded with tracheostomy, enteral nutrition, and subglottic secretion drainage recorded over the course of the study. We mistakenly used a cutoff of ≥107 CFU/ml for tracheal aspirates. This high threshold decreases the sensitivity of the methods without offering any significant advantage in terms of specificity. However, the same threshold was used for both body position groups. Finally, the vast majority of the study cohort consisted of patients with a medical admission; therefore it might not be possible to generalize the results or extrapolate them to other types of patients with severe ARDS, such as trauma patients.
However, our study also has several strengths. It is a prospective study in a large population of patients with severe ARDS. The VAP diagnosis was confirmed with central adjudication by an intensivist not involved in the trial, blinded to the supine or prone position group. We used the Cox proportional hazards regression model to investigate the covariates associated with the mortality at the time of ICU discharge by taking into account VAP as a time-dependent covariate. According to this analysis VAP was associated with patient outcome. Antibiotic therapy showed a very high level of compliance with the ATS guidelines.
Conclusion
In severe ARDS patients prone positioning did not reduce the incidence of VAP and VAP was associated with higher mortality.
References
Azoulay E, Citerio G, Bakker J, Bassetti M, Benoit D, Cecconi M, Curtis JR, Hernandez G, Herridge M, Jaber S, Joannidis M, Papazian L, Peters M, Singer P, Smith M, Soares M, Torres A, Vieillard-Baron A, Timsit JF (2014) Year in review in Intensive Care Medicine 2013: II. Sedation, invasive and noninvasive ventilation, airways, ARDS, ECMO, family satisfaction, end-of-life care, organ donation, informed consent, safety, hematological issues in critically ill patients. Intensive Care Med 40:305–319
Hernu R, Wallet F, Thiolliere F, Martin O, Richard JC, Schmitt Z, Wallon G, Delannoy B, Rimmele T, Demaret C, Magnin C, Vallin H, Lepape A, Baboi L, Argaud L, Piriou V, Allaouchiche B, Aubrun F, Bastien O, Lehot JJ, Ayzac L, Guerin C (2013) An attempt to validate the modification of the American-European consensus definition of acute lung injury/acute respiratory distress syndrome by the Berlin definition in a university hospital. Intensive Care Med 39:2161–2170
Nair GB, Niederman MS (2015) Ventilator-associated pneumonia: present understanding and ongoing debates. Intensive Care Med 41:34–48
Melsen WG, Rovers MM, Bonten MJ (2009) Ventilator-associated pneumonia and mortality: a systematic review of observational studies. Crit Care Med 37:2709–2718
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Forel JM, Voillet F, Pulina D, Gacouin A, Perrin G, Barrau K, Jaber S, Arnal JM, Fathallah M, Auquier P, Roch A, Azoulay E, Papazian L (2012) Ventilator-associated pneumonia and ICU mortality in severe ARDS patients ventilated according to a lung-protective strategy. Crit Care 16:R65
Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, Mercier E, Badet M, Mercat A, Baudin O, Clavel M, Chatellier D, Jaber S, Rosselli S, Mancebo J, Sirodot M, Hilbert G, Bengler C, Richecoeur J, Gainnier M, Bayle F, Bourdin G, Leray V, Girard R, Baboi L, Ayzac L, PROSEVA Study Group (2013) Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 368:2159–2168
Ayzac L, Baboi L, Beuret P, Girard R, Richard JC, Guérin C (2014) Ventilator associated pneumonia in severe ARDS patients treated by prone position. Results from a multicenter randomized controlled trial. Intensive Care Med 40:005
Guerin C, Gaillard S, Lemasson S, Ayzac L, Girard R, Beuret P, Palmier B, Le QV, Sirodot M, Rosselli S, Cadiergue V, Sainty JM, Barbe P, Combourieu E, Debatty D, Rouffineau J, Ezingeard E, Millet O, Guelon D, Rodriguez L, Martin O, Renault A, Sibille JP, Kaidomar M (2004) Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA 292:2379–2387
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149:818–824
American Thoracic Society, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Sud S, Sud M, Friedrich JO, Adhikari NK (2008) Effect of mechanical ventilation in the prone position on clinical outcomes in patients with acute hypoxemic respiratory failure: a systematic review and meta-analysis. CMAJ 178:1153–1161
Beuret P, Carton MJ, Nourdine K, Kaaki M, Tramoni G, Ducreux JC (2002) Prone position as prevention of lung injury in comatose patients: a prospective, randomized, controlled study. Intensive Care Med 28:564–569
Mounier R, Adrie C, Francais A, Garrouste-Orgeas M, Cheval C, Allaouchiche B, Jamali S, Dinh-Xuan AT, Goldgran-Toledano D, Cohen Y, Azoulay E, Timsit JF, Ricard JD, OUTCOMEREA Study Group (2010) Study of prone positioning to reduce ventilator-associated pneumonia in hypoxaemic patients. Eur Respir J 35:795–804
Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, Jaeschke RZ, Brun-Buisson C (1998) Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Ann Intern Med 129:433–440
Koulenti D, Lisboa T, Brun-Buisson C, Krueger W, Macor A, Sole-Violan J, Diaz E, Topeli A, DeWaele J, Carneiro A, Martin-Loeches I, Armaganidis A, Rello J, EU-VAP/CAP Study Group (2009) Spectrum of practice in the diagnosis of nosocomial pneumonia in patients requiring mechanical ventilation in European intensive care units. Crit Care Med 37:2360–2368
Timsit JF, Citerio G, Bakker J, Bassetti M, Benoit D, Cecconi M, Curtis JR, Hernandez G, Herridge M, Jaber S, Joannidis M, Papazian L, Peters M, Singer P, Smith M, Soares M, Torres A, Vieillard-Baron A, Azoulay E (2014) Year in review in Intensive Care Medicine 2013: III. Sepsis, infections, respiratory diseases, pediatrics. Intensive Care Med 40:471–483
Bekaert M, Timsit JF, Vansteelandt S, Depuydt P, Vesin A, Garrouste-Orgeas M, Decruyenaere J, Clec’h C, Azoulay E, Benoit D, Outcomerea Study Group (2011) Attributable mortality of ventilator-associated pneumonia: a reappraisal using causal analysis. Am J Respir Crit Care Med 184:1133–1139
Torres A, Fernandez-Barat L (2014) New developments in the diagnosis of VAP make bronchoalveolar lavage less useful: some considerations. Intensive Care Med 40:1778–1779
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Take-home message: Prone positioning does not reduce the incidence of ventilator-associated pneumonia in severe ARDS patients. VAP was associated with higher mortality in severe ARDS patients.
On the behalf of the PROSEVA trial investigators.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ayzac, L., Girard, R., Baboi, L. et al. Ventilator-associated pneumonia in ARDS patients: the impact of prone positioning. A secondary analysis of the PROSEVA trial. Intensive Care Med 42, 871–878 (2016). https://doi.org/10.1007/s00134-015-4167-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4167-5