Abstract
Introduction
Ventilator-associated pneumonia (VAP) may contribute to the mortality associated with acute respiratory distress syndrome (ARDS). We aimed to determine the incidence, outcome, and risk factors of bacterial VAP complicating severe ARDS in patients ventilated by using a strictly standardized lung-protective strategy.
Methods
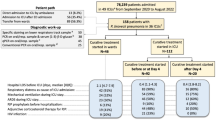
This prospective epidemiologic study was done in all the 339 patients with severe ARDS included in a multicenter randomized, placebo-controlled double-blind trial of cisatracurium besylate in severe ARDS patients. Patients with suspected VAP underwent bronchoalveolar lavage to confirm the diagnosis.
Results
Ninety-eight (28.9%) patients had at least one episode of microbiologically documented bacterial VAP, including 41 (41.8%) who died in the ICU, compared with 74 (30.7%) of the 241 patients without VAP (P = 0.05). After adjustment, age and severity at baseline, but not VAP, were associated with ICU death. Cisatracurium besylate therapy within 2 days of ARDS onset decreased the risk of ICU death. Factors independently associated with an increased risk to develop a VAP were male sex and worse admission Glasgow Coma Scale score. Tracheostomy, enteral nutrition, and the use of a subglottic secretion-drainage device were protective.
Conclusions
In patients with severe ARDS receiving lung-protective ventilation, VAP was associated with an increased crude ICU mortality which did not remain significant after adjustment.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) still carries a high mortality rate. Ventilator-associated pneumonia (VAP) is a complication of ARDS that may increase the risk of multiple organ failure and death. However, the impact of nosocomial pneumonia on mortality in mechanically ventilated patients remains controversial [1–4], and few data are available on mortality in ARDS patients who experience VAP [5–10]. Moreover, many of the studies related to VAP in ARDS patients were performed before the use of lung-protective mechanical-ventilation strategies. Modifications in mechanical-ventilation settings may have modified the epidemiology and outcomes of VAP in patients with severe ARDS [11].
Here, we report the results of an epidemiologic study performed in all patients included in a multicenter randomized, placebo-controlled double-blind trial conducted to determine whether briefly administering the neuromuscular blocking agent (NMBA) cisatracurium besylate early in the course of severe ARDS improved the clinical outcomes. The results of this therapeutic intervention have been reported elsewhere [12]. The main objective of this prospective study was to determine whether bacterial VAP complicating severe ARDS was associated with ICU death in patients receiving lung-protective mechanical ventilation. We also determined the incidence and risk factors of VAP.
Materials and methods
Patients were enrolled from March 2006 through March 2008 at 20 French intensive care units [12]. The study protocol was approved for all centers by the ethics committee of the Marseille University Hospital (Comité Consultatif de Protection des Personnes dans la Recherche Biomédicale Marseille 1, no 04/37). According to French law, written informed consent was obtained from the patients or their surrogates.
Patients
Patients receiving endotracheal mechanical ventilation for severe ARDS were eligible if the following criteria were met for no more than 48 hours before enrollment: ratio of partial pressure of arterial oxygen to fraction of inspired oxygen (PaO2:FIO2) no greater than 150 mm Hg at the time of enrollment, with a PEEP of at least 5 cm H2O and a tidal volume of 6 to 8 ml/kg, recent appearance of bilateral pulmonary infiltrates consistent with edema, and no evidence of left atrial hypertension.
Exclusion criteria were age younger than 18 years, lack of consent, continuous infusion of NBMA, known allergy to NMBA, known pregnancy, participation in another trial within 30 days before meeting the eligibility criteria, increased intracranial pressure, severe chronic respiratory disease requiring long-term oxygen therapy or home mechanical ventilation, actual body weight exceeding 1 kg/cm of height, severe burns, severe chronic liver disease (Child-Pugh class C), bone marrow transplantation or chemotherapy-induced neutropenia, pneumothorax, expected duration of mechanical ventilation shorter than 48 hours, and decision to withhold life-sustaining treatment.
Design
Suspected pneumonia was defined as the presence of new or persistent radiographic features suggesting pneumonia without any other obvious cause and with two of the following: fever > 38°C, leukocytosis (> 11.0 109/L) or leukopenia (< 3.5 109/L), purulent endotracheal aspirate, recent isolation of pathogenic bacteria from the endotracheal aspirate [13], and increasing oxygen requirements. These criteria had to be present more than 2 days after ARDS onset. Bronchoalveolar lavage (BAL) was done in the affected region of the lung identified on a chest radiograph. When PaO2:FIO2 was lower than 80, protected minibronchoalveolar lavage with a protected telescopic catheter could be performed.
Diagnosis of ventilator-associated pneumonia
In each ICU, an investigator made daily rounds to identify eligible patients and patients meeting criteria for suspected VAP. VAP was diagnosed when a quantitative culture of BAL fluid grew at least one bacterial organism in a concentration ≥ 104 colony-forming units (CFU)/ml or when mini-BAL fluid grew at least one bacterial organism in a concentration ≥ 103 CFU/ml [14].
Definitions
Early-onset VAP complicating ARDS was defined as pneumonia diagnosed between the third and seventh days after ARDS onset. Late-onset VAP complicating ARDS was defined as pneumonia diagnosed more than 7 days after ARDS. Patients were monitored for VAP until their discharge from the ICU to a maximum of 90 days.
Empiric antibiotic therapy was started within a 24-hour period after microbiologic samples were obtained by BAL or protected telescoping catheter. Appropriate empiric antibiotic therapy was defined as in vitro susceptibility to at least one antibiotic of the organism(s) recovered from the BAL or the protected telescoping catheter samples. However, if Pseudomonas sp. was isolated, susceptibility to two drugs was required [15].
In patients with clinical and radiographic evidence of deterioration after an initial improvement after a first VAP, relapsing or recurrent infection was suspected if the organism found initially was identified, and superinfection, if a different organism was found.
Data collection
Demographic data were collected. For the 24 hours before randomization, we collected the physiological variables, relevant therapeutic interventions, radiographic findings, co-morbidities, and medications. Ventilator settings, physiological variables, radiographic findings, and relevant therapeutic interventions were recorded just before starting the study drug and then 24, 48, 72, and 96 hours later, and daily thereafter between 6 a.m. and 10 a.m. until day 90 or hospital discharge while breathing without assistance. Patients were monitored daily for 28 days for signs of failure of nonpulmonary organs and systems [16]. We recorded the culture results, antibiotics used, duration of mechanical ventilation, ICU-stay length, and hospital-stay length. Throughout the ICU stay and until weaning off the ventilator for patients without VAP or the diagnosis of VAP for patients with VAP, we recorded daily the following factors potentially associated with VAP: neuromuscular blocking agent (NMBA) use during the first 48 hours, enteral nutrition, stress-ulcer prophylaxis, tracheostomy, transport out of the ICU (operating room, CT-scan), subglottic secretion drainage, selective digestive decontamination, emergency reintubation, prone positioning, and renal replacement therapy.
Ventilation strategy
The volume-assist control mode was used, with a low tidal volume of 6 ml/kg of predicted body weight. The oxygenation goal was to maintain an arterial oxyhemoglobin saturation measured by pulse oximetry of 88% to 95% or a PaO2 of 55 to 80 mm Hg. This goal was achieved by adjusting FIO2 and PEEP, as done in the ARMA study [16]. The same ventilator-weaning protocol was used in both groups. Weaning was to be started on day 3 if the FIO2 was no greater than 0.6.
Statistical analysis
We report means (± SD), relative risks with 95% confidence intervals (CIs), and medians with interquartile ranges (IQR) as appropriate. Differences between groups were assessed by using the Student t test, Wilcoxon test, χ2 analysis, or Fisher Exact test. We used the Wilcoxon test to compare the numbers of ventilator-free days, ICU-free days, and organ-failure-free days, all of which had skewed distributions. All reported P values are two-sided.
Kaplan-Meier curves were constructed to assess the time from enrollment to death and to unassisted breathing within 90 days.
To analyze the effect of VAP on ICU mortality, we reported crude ICU mortality. We also performed a logistic regression (forced-entry model) to identify factors independently associated with ICU death. We planned to include all variables with P values < 0.20 by univariate analysis. Colinearity also was assessed. The occurrence of a VAP and the use of NMBA during the first 48 hours of ARDS were also entered in the model. In addition, we performed a multistate approach (clock-forward multistate model) to take into account both the time-dependence of the VAP and the presence of competing risks (for example, ICU death and discharge alive from the ICU) at each time point.
To identify risk factors for bacterial VAP, we also used the clock-forward multistate model. Of the 11 variables finally included in the model, seven had P values < 0.20 by univariate analysis (male sex, baseline Glasgow Coma Scale score, emergency reintubation, tracheostomy, transport out of the ICU, enteral nutrition, and subglottic secretion drainage) and four were predefined covariates (baseline SAPS II score, baseline PaO2:FI O2, baseline respiratory system compliance, and continuous NMBA use during the first 48 hours of ARDS).
All statistical analyses were performed by using PASW Statistics software version 17 and R development Core Team (2010). The multistage analysis was done by using mstate package 0.2.6 (see Additional file 1) [17, 18].
Results
Study population
Table 1 reports the main characteristics of the 339 severe ARDS patients. ARDS was caused by a direct lung injury in 265 (78%) patients. The ICU mortality rate was 33.9% (115 of 339). We found no clinically significant differences between the groups with and without VAP regarding the main baseline characteristics, co-morbidities, or severity scores at ICU admission, except for a significantly higher proportion of male patients in the VAP group.
Incidence of ventilator-associated pneumonia
During the study period, 120 suspected first episodes of bacterial VAP were evaluated by using BAL or mini-BAL. A bacterial VAP was diagnosed in 98 (28.9%) patients, with 26 cases of early-onset and 72 of late-onset first VAP episode. In 69 patients, a single VAP episode occurred. Twenty-two of the 98 patients had a second episode of VAP, whereas five had three episodes, and two had four episodes. A relapse or recurrent infection was diagnosed in six patients, and superinfections, in 32 patients.
Median time on mechanical ventilation from ARDS onset to the first VAP episode was 10 days (IQR, 6 to 17 days). Median time on mechanical ventilation from endotracheal intubation to the first VAP episode was 11 days (IQR, 7 to 17 days). Most of the first VAP episodes occurred within 3 weeks after ARDS onset. Figure 1 shows the cumulative probability of developing VAP over time. The daily risk for developing bacterial VAP increased until day 9 and then decreased throughout the remainder of the ICU stay (Figure 2). The daily risk was 9% on day 7, 6% on day 12, and 3% on day 21.
Hazard rate for ventilator-associated pneumonia over time after the diagnosis of severe acute respiratory distress syndrome. The hazard function evaluates the conditional probability of ventilator-associated pneumonia on the next day in an event-free patient. The hazard rate is the event rate per day over the duration of mechanical ventilation.
In all, 112 bacterial strains grew in significant concentrations in BAL or protected mini-BAL specimens during the first VAP episode. As indicated in Table 2, the most common bacteria were nonfermenting, gram-negative bacilli (P. aeruginosa, Acinetobacter baumannii, and Stenotrophomonas maltophilia) (40%) followed by Enterobacteriaceae (29%) and Staphylococcus aureus (21%).
Clinical outcomes
Mortality
The median time from VAP diagnosis to death was 8.5 days (IQR, 5.5 to 17 days). Of the 98 patients with VAP, 41 (41.8%; CI, 32.6% to 51.7%) died in the ICU, compared with 74 (30.7%; CI, 25.2% to 36.8%) of the 241 patients without VAP (Table 3 and Figure 3) (P = 0.05). In patients with early-onset VAP, mortality was 53.9% (14 of 26 patients; CI, 35.5% to 71.3%), compared with 37.5% (27 of 72 patients; CI, 27.2% to 49.1%) in patients with late-onset VAP (P = 0.15).
To determine whether VAP was an independent risk factor for dying during the ICU stay in ARDS patients, we performed a multiple logistic regression and a Cox analysis by using a multistate model. As mentioned in Table 4, age, male sex, plateau pressure on inclusion, SOFA on inclusion, McCabe score, the systematic use of NMBA, and the occurrence of VAP were entered into the logistic regression model. The occurrence of a VAP was not independently associated with the risk of ICU death. With the multistate model, and after controlling for the same risk factors, we were able to confirm that the occurrence of a bacterial VAP was not associated with the risk of ICU death (HR, 0.25; 95% CI from 0.003 to 23.5; P = 0.55). We conducted a post hoc analysis excluding the patients who were not ventilated for at least 9 days after inclusion (the first death in the VAP group occurred at day 10). Survival was higher in the group of ARDS patients not developing a VAP (P = 0.038 by log-rank test). However, VAP was not associated independently with death with a Cox regression analysis with the same risk factors (P = 0.055).
Ventilator-free days
As indicated in Table 3, the numbers of ventilator-free days from day 1 to day 28 and to day 90 were significantly larger in patients without VAP than in patients with VAP. The median duration of mechanical ventilation was longer in patients with VAP who were alive on day 90. As shown in Figure 4, patients without VAP were disconnected earlier from the ventilator.
Adequacy of empiric antibiotic treatment
Empiric treatment was adequate in 95% of patients. The mean duration of antibiotic treatment for VAP was 10.4 ± 5.2 days overall and 11.3 ± 5.2 days in patients alive at ICU discharge.
Risk factors for ventilator-associated pneumonia
By univariate analysis (Table 5), male sex and transport out of the ICU were strongly associated with VAP. Both consciousness alterations and enteral nutrition showed trends toward associations with VAP. In contrast, VAP was not associated with NMBA use, stress-ulcer prophylaxis (proton-pump inhibitors, sucralfate, H2-blockers, or antacids), ARDS severity, or admission SAPS II score. All factors listed in Table 6 were entered into the multistate model. Male sex, baseline Glasgow Coma Scale score, tracheostomy (protective), enteral nutrition (protective), and the use of a subglottic secretion-drainage system (protective) were independently associated with VAP.
Discussion
Our study has three main findings. First, bacterial VAP was diagnosed in approximately one third of patients with severe ARDS. Second, VAP was associated with a higher crude ICU mortality rate. However, no effect of VAP on ICU mortality was found after adjustment. Third, male sex and baseline Glasgow Coma Scale score were associated with VAP in our patients with severe ARDS, whereas tracheostomy, enteral nutrition, and the use of a subglottic secretion-drainage system were protective.
Study rationale
Although several [6–10] studies evaluated the incidence of VAP in patients with ARDS, only one [8] sought to identify specific risk factors for VAP, and all but one [8] used a single-center design. These studies included 30 to 134 ARDS patients (Table 7). Much more important, they were performed before the widespread use of lung-protective ventilation. To our knowledge, the epidemiology and outcomes of VAP have not been evaluated in ARDS patients receiving a strictly standardized protocol of lung-protective mechanical ventilation [12]. This standardization is important, as recent evidence indicates that cyclic stretching of lung cells promotes bacterial growth [11], suggesting that variations in the ventilation strategy may affect the risk of VAP.
Incidence of ventilator-associated pneumonia
None of the patients received new antibiotics before BAL or mini-BAL. Thus, the 28.9% incidence probably reflects the incidence of bacterial VAP in our ARDS patients, even if some suspicions were unconfirmed (maybe some false-negatives existed). The main difference between our study and earlier studies [6–10] is that the patients received lung-protective mechanical ventilation according to a strict protocol.
Mortality and ventilator-associated pneumonia
The excess mortality potentially associated with VAP in patients with severe ARDS is difficult to assess, because many factors may contribute to death in such patients. The management of ARDS has changed over the last 15-year period. Lung-protective mechanical ventilation is now the standard of care. This change may contribute to explaining the differences in ICU mortality between our study (41.8% versus 30.7% with and without VAP, respectively) and previously published studies [6–8] (52% to 78% versus 59% to 92% with and without VAP, respectively), which occurred despite similar baseline severity scores (Table 7). However, improvements have occurred in general ICU care and mortality in many other critical illnesses during recent years.
Risk factors for VAP
Only male sex and the admission Glasgow Coma Scale score were independently associated with an increased risk of developing a bacterial VAP in our patients with severe ARDS. In a study of 5,081 patients, Combes et al. [19] found that nosocomial pneumonia was more common in men than in women (51% versus 44%; P = 0.01). In a large US database including 9,080 patients, male gender was an independent risk factor for VAP. Differences in VAP risk between men and women may be related to differences in sex hormones [20], to sex-related polymorphisms affecting immune responses to bacterial agents [21], to differences in the distribution of pathogens responsible for infections, to differences in chronic comorbidities [22], and/or to differences in the level of care [23]. Severity of illness, and most notably neurologic failure [24–29], is associated with an increased risk of VAP. Finally, routine NMBA use during the early phase of ARDS was not associated with the risk of VAP. This is in contrast with some previous studies [25, 30, 31], in which NMBA use (for whatever duration) in nonselected mechanically ventilated ICU patients was associated with a higher risk of VAP.
Study limitations
As stated in the ACURASYS study report [12], only 339 of 1,326 patients with severe ARDS assessed for eligibility were included. However, the vast majority of the remaining 987 patients had exclusion criteria. The strictly standardized ventilation protocol and strategy for VAP diagnosis are major strengths of our study. Viral pneumonia was not evaluated, as some of the participating centers did not routinely perform viral studies. A study of the impact of viral infection on outcomes of ARDS patients might be of interest.
Conclusions
In those with severe ARDS, patients ventilated according to a standardized lung-protective strategy, the development of VAP was associated with a higher risk for dying in the ICU. However, no relation to ICU death was found after adjustment.
Key messages
-
In severe ARDS patients ventilated according to a strictly standardized lung-protection strategy, VAP increased crude ICU mortality.
-
However, after adjustment, VAP did not remain associated with ICU mortality.
-
Factors independently associated with an increased risk of acquiring VAP were male sex and admission Glasgow Coma Scale score.
Abbreviations
- ARDS:
-
acute respiratory distress syndrome
- VAP:
-
ventilator-associated pneumonia
- NMBA:
-
neuromuscular blocking agent
- PaO2:
-
FIO2: ratio of partial pressure of arterial oxygen to fraction of inspired oxygen
- BAL:
-
bronchoalveolar lavage
- (CFU)/ml:
-
colony-forming units per milliliter
- SAPS II:
-
Simplified Acute Physiology Score
- SOFA:
-
sequential organ failure assessment.
References
Bregeon F, Ciais V, Carret V, Gregoire R, Saux P, Gainnier M, Thirion X, Drancourt M, Auffray JP, Papazian L: Is ventilator-associated pneumonia an independent risk factor for death? Anesthesiology 2001, 94: 554-560. 10.1097/00000542-200104000-00005
Fagon J, Chastre J, Hance A, Montravers P, Novara A, Gibert C: Nosocomial pneumonia in ventilated patients: a cohort study evaluating attributable mortality and hospital stay. Am J Med 1993, 94: 281-288. 10.1016/0002-9343(93)90060-3
Papazian L, Bregeon F, Thirion X, Gregoire R, Saux P, Denis J, Perin G, Charrel J, Dumon J, Affray J, Gouin F: Effect of ventilator-associated pneumonia on mortality and morbidity. Am J Respir Crit Care Med 1996, 154: 91-97.
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K: International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009, 302: 2323-2329. 10.1001/jama.2009.1754
Iregui MG, Kollef MH: Ventilator-associated pneumonia complicating the acute respiratory distress syndrome. Seminars in respiratory and critical care medicine 2001, 22: 317-326. 10.1055/s-2001-15788
Chastre J, Trouillet JL, Vuagnat A, Joly-Guillou ML, Clavier H, Dombret MC, Gibert C: Nosocomial pneumonia in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 1998, 157: 1165-1172.
Delclaux C, Roupie E, Blot F, Brochard L, Lemaire F, Brun-Buisson C: Lower respiratory tract colonization and infection during severe acute respiratory distress syndrome: incidence and diagnosis. Am J Respir Crit Care Med 1997, 156: 1092-1098.
Markowicz P, Wolff M, Djedaini K, Cohen Y, Chastre J, Delclaux C, Merrer J, Herman B, Veber B, Fontaine A, Dreyfuss D: Multicenter prospective study of ventilator-associated pneumonia during acute respiratory distress syndrome. Incidence, prognosis, and risk factors. ARDS Study Group. Am J Respir Crit Care Med 2000, 161: 1942-1948.
Sutherland KR, Steinberg KP, Maunder RJ, Milberg JA, Allen DL, Hudson LD: Pulmonary infection during the acute respiratory distress syndrome. Am J Respir Crit Care Med 1995, 152: 550-556.
Meduri GU, Reddy RC, Stanley T, El-Zeky F: Pneumonia in acute respiratory distress syndrome. A prospective evaluation of bilateral bronchoscopic sampling. Am J Respir Crit Care Med 1998, 158: 870-875.
Pugin J, Dunn-Siegrist I, Dufour J, Tissieres P, Charles PE, Comte R: Cyclic stretch of human lung cells induces an acidification and promotes bacterial growth. Am J Respir Cell Mol Biol 2008, 38: 362-370.
Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, Constantin JM, Courant P, Lefrant JY, Guerin C, Prat G, Morange S, Roch A: Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 2010, 363: 1107-1116. 10.1056/NEJMoa1005372
Michel F, Franceschini B, Berger P, Arnal JM, Gainnier M, Sainty JM, Papazian L: Early antibiotic treatment for BAL-confirmed ventilator-associated pneumonia: a role for routine endotracheal aspirate cultures. Chest 2005, 127: 589-597. 10.1378/chest.127.2.589
Bregeon F, Papazian L, Thomas P, Carret V, Garbe L, Saux P, Drancourt M, Auffray JP: Diagnostic accuracy of protected catheter sampling in ventilator-associated bacterial pneumonia. Eur Respir J 2000, 16: 969-975. 10.1183/09031936.00.16596900
Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia Am J Respir Crit Care Med 2005, 171: 388-416.
Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network N Engl J Med 2000, 342: 1301-1308.
de Wreede LC, Fiocco M, Putter H: The mstate package for estimation and prediction in non- and semi-parametric multi-state and competing risks models. Computer methods and programs in biomedicine 2010, 99: 261-274. 10.1016/j.cmpb.2010.01.001
Putter H, Fiocco M, Geskus RB: Tutorial in biostatistics: competing risks and multi-state models. Statistics in medicine 2007, 26: 2389-2430. 10.1002/sim.2712
Combes A, Luyt CE, Trouillet JL, Nieszkowska A, Chastre J: Gender impact on the outcomes of critically ill patients with nosocomial infections. Crit Care Med 2009, 37: 2506-2511. 10.1097/CCM.0b013e3181a569df
Federman DD: The biology of human sex differences. N Engl J Med 2006, 354: 1507-1514. 10.1056/NEJMra052529
Hubacek JA, Stuber F, Frohlich D, Book M, Wetegrove S, Ritter M, Rothe G, Schmitz G: Gene variants of the bactericidal/permeability increasing protein and lipopolysaccharide binding protein in sepsis patients: gender-specific genetic predisposition to sepsis. Crit Care Med 2001, 29: 557-561. 10.1097/00003246-200103000-00015
Esper AM, Moss M, Lewis CA, Nisbet R, Mannino DM, Martin GS: The role of infection and comorbidity: Factors that influence disparities in sepsis. Crit Care Med 2006, 34: 2576-2582. 10.1097/01.CCM.0000239114.50519.0E
Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG: Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med 2003, 31: 1901-1907. 10.1097/01.CCM.0000069347.78151.50
Craven DE, Kunches LM, Kilinsky V, Lichtenberg DA, Make BJ, McCabe WR: Risk factors for pneumonia and fatality in patients receiving continuous mechanical ventilation. Am Rev Respir Dis 1986, 133: 792-796.
Cook DJ, Walter SD, Cook RJ, Griffith LE, Guyatt GH, Leasa D, Jaeschke RZ, Brun-Buisson C: Incidence of and risk factors for ventilator-associated pneumonia in critically ill patients. Ann Intern Med 1998, 129: 433-440.
Magret M, Amaya-Villar R, Garnacho J, Lisboa T, Diaz E, Dewaele J, Deja M, Manno E, Rello J: Ventilator-associated pneumonia in trauma patients is associated with lower mortality: results from EU-VAP study. J Trauma 2010, 69: 849-854. 10.1097/TA.0b013e3181e4d7be
Esperatti M, Ferrer M, Theessen A, Liapikou A, Valencia M, Saucedo LM, Zavala E, Welte T, Torres A: Nosocomial pneumonia in the intensive care unit acquired during mechanical ventilation or not. Am J Respir Crit Care Med 2010, 182: 1533-1539. 10.1164/rccm.201001-0094OC
Ewig S, Torres A, El-Ebiary M, Fabregas N, Hernandez C, Gonzalez J, Nicolas JM, Soto L: Bacterial colonization patterns in mechanically ventilated patients with traumatic and medical head injury. Incidence, risk factors, and association with ventilator-associated pneumonia. Am J Respir Crit Care Med 1999, 159: 188-198.
Rello J, Torres A, Ricart M, Valles J, Gonzalez J, Artigas A, Rodriguez-Roisin R: Ventilator-associated pneumonia by Staphylococcus aureus. Comparison of methicillin-resistant and methicillin-sensitive episodes. Am J Respir Crit Care Med 1994, 150: 1545-1549.
Da Silva PS, Neto HM, de Aguiar VE, Lopes E Jr, de Carvalho WB: Impact of sustained neuromuscular blockade on outcome of mechanically ventilated children. Pediatr Int 2010, 52: 438-443. 10.1111/j.1442-200X.2010.03104.x
Leone M, Delliaux S, Bourgoin A, Albanese J, Garnier F, Boyadjiev I, Antonini F, Martin C: Risk factors for late-onset ventilator-associated pneumonia in trauma patients receiving selective digestive decontamination. Intensive Care Med 2005, 31: 64-70. 10.1007/s00134-004-2514-z
Acknowledgements
Marseille: Hôpital Nord - J. Albanese, V. Blasco, M. Leone, F. Antonini, P. Visintini; Hôpital Sainte-Marguerite -D. Blayac, B. Eon, P. Michelet, P. Saux, D. Lambert, V. Fulachier; Hôpital Sainte-Marguerite - C. Guervilly, J. Allardet-Servent, D. Demory, N. Embriaco, M. Gainnier, L. Papazian; Hôpital Ambroise Paré - J.M. Seghboyan, N. Beni Chougrane, R. Soundaravelou, A. Piera, M. Bonnetty. Paris: Hôpital Saint-Louis - E. Azoulay. Besançon: Hôpital Jean Minjoz - D. Perez, G. Capellier, P. Midez, C. Patry, E. Laurent, E. Belle, J.C. Navellou. Clermont-Ferrand: Hôpital Hôtel-Dieu - J.M. Constantin, S. Cayot-Constantin, R. Guerin. Avignon: Centre Hospitalier - P. Courant, T. Signouret, K. Pavaday, P. Garcia, L. Delapierre, K. Debbat. Toulon: Hôpital Font-Pré -J. Durand-Gasselin, G. Corno, A. Orlando, I. Granier, S.Y. Donati. Rennes: Hôpital Pontchaillou -Y. Le Tulzo, S. Lavoue, C. Camus. Nîmes: Hôpital Caremeau - C. Gervais, C. Bengler, C. Arich; Hôpital Caremeau - J.Y. Lefrant, P. Poupard, L. Muller, P. Joubert, R. Cohendy, G. Saissi, P. Barbaste. Lyon: Hôpital de la Croix-Rousse - C. Guérin, F. Bayle, J.C. Richard, J.M. Badet. Bordeaux: Hôpital Pellegrin - G. Hilbert, H. Bruno, E. Rosier, W. Pujol, H.N. Bui. Montpellier: Hôpital Sanit-Eloi -B. Jung, M. Sebbane, G. Chanques. Brest: Hôpital La Cavale Blanche - G. Prat, E. L'Her, J.M. Tonnelier. Aix-en-Provence: Centre Hospitalier du Pays d'Aix - O. Baldesi, C. Leroy, L. Rodriguez, J.L. Le Grand, B. Garrigues. Nice: Hôpital de l'Archet - G. Bernardin, J. Dellamonica. Grenoble: Hôpital Sud - C. Schwebel, J.F. Timsit, R. Hamidfar, L. Hammer, G. Dessertaine, C. De Couchon, A. Bonadona. Saint-Etienne: Hôpital Bellevue - F. Zeni, D. Thevenet, C. Venet, S. Guyomarc'h. Other acknowledgments:Kahena Amichi, Patrick Sudour, Teodora Iordanova, Jean-Charles Reynier, Mohamed Fathallah, Karine Barrau, Yann Lebras, Nathalie Boggi, Ammar Zerrar, Cécile Roché-Thiaux, Fabienne Brégeon, Didier Dreyfuss, Marie-Josée Bonavita, Marie-Dominique Chollet, Didier Sanchez, Antoinette Wolfe.
This work was supported by the Assistance Publique Hôpitaux de Marseille; and by a grant from the Ministère de la santé [Programme Hospitalier de Recherche Clinique régional 2004-26]; Glaxo-SmithKline France donated the cisatracurium and placebo.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Glaxo-SmithKline France provided the cisatracurium and placebo for the study. Glaxo-SmithKline France gave 30 k€ for the ACURASYS study (main investigator, Laurent Papazian).
Authors' contributions
LP, JMF, AR, DP, and FV were responsible for study concept and design; AG, GP, SJ, JMA, and EA, acquisition of the data; MF, KB, PA, JMF, and LP, analysis and interpretation of the data; JMF, LP, and AR, drafting of the manuscript; and EA, critical revision of the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
13054_2011_530_MOESM1_ESM.DOCX
Additional file 1: Multistate analysis procedure. Description of the multistate model and syntax used in the mstate package 0.2.6 of R development Core Team (2010). (DOCX 39 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Forel, JM., Voillet, F., Pulina, D. et al. Ventilator-associated pneumonia and ICU mortality in severe ARDS patients ventilated according to a lung-protective strategy. Crit Care 16, R65 (2012). https://doi.org/10.1186/cc11312
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11312