Abstract
Purpose
To describe the current practices of volume expansion in French intensive care units (ICU).
Methods
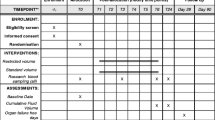
In 19 ICUs, we prospectively observed the prescription and monitoring practices of volume expansion in consecutive adult patients with shock [sustained hypotension and/or need of vasopressor therapy, associated with at least tachycardia and/or sign (s) of hypoperfusion]. Patients were included at the time of prescription of the first fluid bolus (FB). Thereafter, all the FBs administered during the 96 h following shock onset were surveyed. An FB was defined as an intravenous bolus of at least 100 ml of a blood volume expander intended to rapidly improve the patient’s circulatory condition.
Results
We included 777 patients [age: 63 ± 15 years; female gender: 274 (35 %); simplified acute physiology score II: 55.9 ± 20.6; ICU length of stay: 6 days (interquartile range (IQR) 3–13); ICU mortality: 32.8 %] and surveyed 2,694 FBs. At enrolment mean arterial pressure was 63 mmHg (IQR 55–71). The most frequent triggers of FB were hypotension, low urine output, tachycardia, skin mottling and hyperlactataemia. Amount of fluid given at each FB was highly variable between centres. Crystalloids were used in 91 % (2,394/2,635) and synthetic colloids in 3.3 % (87/2,635) of FBs. Overall, clinicians used any kind of haemodynamic assessment (central venous pressure measurement, predictive indices of fluid responsiveness, echocardiography, cardiac output monitoring or a combination of these) in 23.6 % (635/2,694) of all FBs surveyed, with an important between-centre heterogeneity.
Conclusions
High between-centre variability characterised all the aspects of FB prescription and monitoring, but overall haemodynamic exploration to help guide and monitor FB was infrequent.
Similar content being viewed by others
References
Finfer S, Liu B, Taylor C, Bellomo R, Billot L, Cook D, Du B, McArthur C, Myburgh J, SAFE TRIPS Investigators (2010) Resuscitation fluid use in critically ill adults: an international cross-sectional study in 391 intensive care units. Crit Care 14:R185
Antonelli M, Levy M, Andrews PJ et al (2007) Hemodynamic monitoring in shock and implications for management. International consensus conference, Paris, France, 27–28 April 2006. Intensive Care Med 33:575–590
Dellinger RP, Levy MM, Rhodes A et al (2013) Surviving sepsis campaign guidelines committee including the pediatric subgroup: surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 41:580–637
Vincent JL, De Backer D (2013) Circulatory shock. N Engl J Med 369:1726–1734
Perner A, De Backer D (2014) Understanding hypovolaemia. Intensive Care Med 40:613–615
Cavallaro F, Sandroni C, Marano C et al (2010) Diagnostic accuracy of passive leg raising for prediction of fluid responsiveness in adults: systematic review and meta-analysis of clinical studies. Intensive Care Med 36:1475–1483
Marik PE, Cavallazzi R, Vasu T, Hirani A (2009) Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med 37:2642–2647
Boulain T, Meziani F, Ehrmann S, Lascarrou JB, Bouglé A, Chiche A, Lakhal K, Gaudry S, Perbet S, Desachy A, Cabasson S, Geneau I, Courouble P, Clavieras N, Massanet P, Bellec F, Falquet Y, Réminiac F, Vignon P (2013) Pratiques de l’expansion volémique en reanimation. Etude observationnelle multicentrique française. Réanimation 23(Suppl 1):S20
Ait-Oufella H, Lemoinne S, Boelle PY, Galbois A, Baudel JL, Lemant J, Joffre J, Margetis D, Guidet B, Maury E, Offenstadt G (2011) Mottling score predicts survival in septic shock. Intensive Care Med 37:801–807
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Perner A, Haase N, Guttormsen AB, 6S Trial Group; Scandinavian Critical Care Trials Group et al (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
Myburgh JA, Finfer S, Bellomo R, CHEST Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group et al (2012) Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 367:1901–1911
Perel P, Roberts I, Ker K (2013) Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev 2:CD000567. doi:10.1002/14651858.CD000567.pub6
Marik PE, Cavallazzi R (2013) Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med 41:1774–1781
Rivers E, Nguyen B, Havstad S et al (2001) Early goal-directed therapy collaborative group: early goal directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Weil MH, Henning RJ (1979) New concepts in the diagnosis and fluid treatment of circulatory shock. Anesth Analg 58:124–132
Vincent JL, Weil MH (2006) Fluid challenge revisited. Crit Care Med 34:1333–1337
Monnet X, Rienzo M, Osman D et al (2006) Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med 34:1402–1407
Boulain T, Achard JM, Teboul JL et al (2002) Changes in BP induced by passive leg raising predict response to fluid loading in critically ill patients. Chest 121:1245–1252
Lakhal K, Ehrmann S, Runge I et al (2010) Central venous pressure measurements improve the accuracy of leg raising-induced change in pulse pressure to predict fluid responsiveness. Intensive Care Med 36:940–948
Lakhal K, Ehrmann S, Benzekri-Lefèvre D et al (2012) Brachial cuff measurements of blood pressure during passive leg raising for fluid responsiveness prediction. Ann Fr Anesth Reanim 31:67–72
Melot J, Sebbane M, Dingemans G, AzuRéa Groupe et al (2012) Use of indicators of fluid responsiveness in septic shock: a survey in public emergency departments. Ann Fr Anesth Reanim 31:583–590
Rajaram SS, Desai NK, Kalra A, et al (2013) Pulmonary artery catheters for adult patients in intensive care. Cochrane Database Syst Rev 2:CD003408. doi:10.1002/14651858.CD003408.pub3
Hilton AK, Bellomo R (2012) A critique of fluid bolus resuscitation in severe sepsis. Crit Care 16:302
Raghunathan K, McGee WT, Higgins T (2012) Importance of intravenous fluid dose and composition in surgical ICU patients. Curr Opin Crit Care 18:350–357
Westphal M (2013) Get to the point in intensive care medicine—the sooner the better? Crit Care 17(Suppl 1):S8
Kox M, Pickkers P (2013) “Less is more” in critically III patients: not too intensive. JAMA Intern Med 173:1369
Myburgh JA, Mythen MG (2013) Resuscitation fluids. N Engl J Med 369:1243–1251
Myers C (1997) Fluid resuscitation. Eur J Emerg Med 4:224–232
Hilton AK, Bellomo R (2011) Totem and taboo: fluids in sepsis. Crit Care 15:164
Prowle JR (2012) Fluid resuscitation in septic shock: too much, too little or just right? Crit Care 16:436
Wiedemann HP, Wheeler AP, Bernard GR et al (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Schortgen F, Deye N, Brochard L, CRYCO Study Group (2004) Preferred plasma volume expanders for critically ill patients: results of an international survey. Intensive Care Med 30:2222–2229
The FLUIDS study investigators for the Scandinavian Critical Care Trials Group (2008) Preferences for colloid use in Scandinavian intensive care units: preferences for colloid use. Acta Anaesth Scand 52:750–758
Boldt J, Lenz M, Kumle B et al (1998) Volume replacement strategies on intensive care units: results from a postal survey. Intensive Care Med 24:147–151
Vincent JL, de Mendonça A, Cantraine F et al (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European society of intensive care medicine. Crit Care Med 26:1793–1800
Acknowledgments
Additional contributors to the PREVER Study Group: Olivier Baudin, Sylvie Calvat, Christophe Cracco, Charles Lafon, Stéphane Rouleau (Angoulême, CRICS group); Julien Pascal, Matthieu Jabaudon, Renaud Guérin, Sophie Cayot, Jean-Michel Constantin (Clermont-Ferrand); Damien Roux, Sylvain Jean-Baptiste, Clément Leclaire, Karim Ben Ahmed, Jonathan Messika Jean-Damien Ricard, Didier Dreyfuss, Louis-Marie Dumont, Camille Lhotte, Pauline Balagny, Julia Attali, Sonia Ayllon-Milla (Colombes); Aihem Yehia, Konstantinos Bachoumas, Gwenhael Colin, Maud Fiancette, Jean Claude Lacherade, Matthieu Henry Lagarrigue, Christine Lebert, Laurent Martin-Lefèvre, Jean Reignier, Isabelle Vinatier, (La Roche Sur Yon, CRICS group); Olivier Lesieur (La Rochelle); Marc Clavel, Nicolas Pichon, Bruno François, Emmanuelle Begot, Anne-Laure Fedou, Thomas Daix, Roxana Donisanu, Bénédicte Durgueil, Céline Gonzalez, Tiffany Duvoid (Limoges, CRICS group); Patrick Bardou, Michel Bonnivard, Anne Marco, Jérôme Roustan, Sylvie Vimeux (Montauban, CRICS group); Matthieu Conseil, Samir Jaber, Guillaume Rao, Daniel Verzilli (Department of Critical Care Medicine and Anesthesiology, Montpellier); Philippe Corne, Gilles Vincent (Department of Intensive Care Medicine, Montpellier); Laurent Brisard, Patrick Michel, Sophie Pajot, Pierre-André Rodie-Talbere, Nelly Rondeau (Nantes); François Barbier, Dalila Benzekri-Lefevre, Nicolas Bercault, Anne Bretagnol, Toufik Kamel, Armelle Mathonnet, Grégoire Muller, Isabelle Runge (Orléans, CRICS group); Romain Sonneville (Bichat, Paris); Alain Cariou, Fabrice Daviaud, Tristan Morichau-Beauchant (Cochin, Paris); René Robert, Jean-Pierre Frat, Delphine Chatellier, Anne Veinstein, Rémy Coudroy (Poitiers, CRICS group); Michel Grinand, Jérome Hoff, François Labadie, Pierre-Antoine Mielcarek, Paul Morin-Longuet, Freddy Thibaut (Saint-Nazaire); Asaêl Berger, Alexandra Boivin, Laure Stiel (Strasbourg, CRICS group);Nicolas Boussekey, Pierre-Yves Delannoy, Hugues Georges, Olivier Leroy, Agnès Meybeck, Damien Thellier (Tourcoing); Laetitia Bodet-Contentin, Denis Garot, Antoine Guillon, Aurélie Joret, Annick Legras, Claire Lhommet, Julie Mankikian, Emmanuelle Mercier, Emmanuelle Rouve (Tours, CRICS group);.
Conflicts of interest
The authors declare they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message:
Modalities of volume expansion in shocked patients were highly variable in French intensive care units. Overall the use of any kind of haemodynamic assessment to help decide and guide fluid bolus administration was infrequent.
For the Clinical Research in Intensive Care and Sepsis Group, Tours, France (http://www.crics.fr/en/) and for the PREVER study investigators.
The PREVER study investigators are listed in the Acknowledgment section.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Boulain, T., Boisrame-Helms, J., Ehrmann, S. et al. Volume expansion in the first 4 days of shock: a prospective multicentre study in 19 French intensive care units. Intensive Care Med 41, 248–256 (2015). https://doi.org/10.1007/s00134-014-3576-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3576-1