Abstract
Purpose
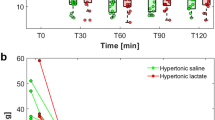
Preventive treatments of traumatic intracranial hypertension are not yet established. We aimed to compare the efficiency of half-molar sodium lactate (SL) versus saline serum solutions in preventing episodes of raised intracranial pressure (ICP) in patients with severe traumatic brain injury (TBI).
Methods
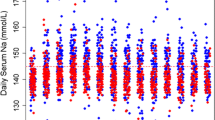
This was a double-blind, randomized controlled trial including 60 patients with severe TBI requiring ICP monitoring. Patients were randomly allocated to receive a 48-h continuous infusion at 0.5 ml/kg/h of either SL (SL group) or isotonic saline solution (control group) within the first 12 h post-trauma. Serial measurements of ICP, as well as fluid, sodium, and chloride balance were performed over the 48-h study period. The primary outcome was the number of raised ICP (≥20 mmHg) requiring a specific treatment.
Results
Raised ICP episodes were reduced in the SL group as compared to the control group within the 48-h study period: 23 versus 53 episodes, respectively (p < 0.05). The proportion of patients presenting raised ICP episodes was smaller in the SL group than in the saline group: 11 (36 %) versus 20 patients (66 %) (p < 0.05). Cumulative 48-h fluid and chloride balances were reduced in the SL group compared to the control group (both p < 0.01).
Conclusion
A 48-h infusion of SL decreased the occurrence of raised ICP episodes in patients with severe TBI, while reducing fluid and chloride balances. These findings suggest that SL solution could be considered as an alternative treatment to prevent raised ICP following severe TBI.



Similar content being viewed by others
References
Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J (2006) A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien) 148:255–268
Stein DM, Hu PF, Brenner M, Sheth KN, Liu KH, Xiong W, Aarabi B, Scalea TM (2011) Brief episodes of intracranial hypertension and cerebral hypoperfusion are associated with poor functional outcome after severe traumatic brain injury. J Trauma 71:364–373
Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright DW (2007) Guidelines for the management of severe traumatic brain injury IX. Cerebral perfusion thresholds. J Neurotrauma 24(Suppl 1):S59–S64
Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright DW (2007) Guidelines for the management of severe traumatic brain injury II. Hyperosmolar therapy. J Neurotrauma 24(Suppl 1):S14–S20
Francony G, Fauvage B, Falcon D, Canet C, Dilou H, Lavagne P, Jacquot C, Payen JF (2008) Equimolar doses of mannitol and hypertonic saline in the treatment of increased intracranial pressure. Crit Care Med 36:795–800
Paczynski RP (1997) Osmotherapy. Basic concepts and controversies. Crit Care Clin 13:105–129
Kamel H, Navi BB, Nakagawa K, Hemphill JC 3rd, Ko NU (2011) Hypertonic saline versus mannitol for the treatment of elevated intracranial pressure: a meta-analysis of randomized clinical trials. Crit Care Med 39:554–559
Ichai C, Armando G, Orban JC, Berthier F, Rami L, Samat-Long C, Grimaud D, Leverve X (2009) Sodium lactate versus mannitol in the treatment of intracranial hypertensive episodes in severe traumatic brain-injured patients. Intensive Care Med 35:471–479
Schurr A, West CA, Rigor BM (1988) Lactate-supported synaptic function in the rat hippocampal slice preparation. Science 240:1326–1328
Gallagher CN, Carpenter KL, Grice P, Howe DJ, Mason A, Timofeev I, Menon DK, Kirkpatrick PJ, Pickard JD, Sutherland GR, Hutchinson PJ (2009) The human brain utilizes lactate via the tricarboxylic acid cycle: a 13C-labelled microdialysis and high-resolution nuclear magnetic resonance study. Brain 132:2839–2849
Oddo M, Levine JM, Frangos S, Maloney-Wilensky E, Carrera E, Daniel RT, Levivier M, Magistretti PJ, Leroux PD (2012) Brain lactate metabolism in humans with subarachnoid hemorrhage. Stroke 43:1418–1421
Maran A, Cranston I, Lomas J, Macdonald I, Amiel SA (1994) Protection by lactate of cerebral function during hypoglycaemia. Lancet 343:16–20
Chen T, Qian YZ, Rice A, Zhu JP, Di X, Bullock R (2000) Brain lactate uptake increases at the site of impact after traumatic brain injury. Brain Res 861:281–287
Meierhans R, Brandi G, Fasshauer M, Sommerfeld J, Schupbach R, Bechir M, Stover J (2012) Arterial lactate above 2 mM is associated with increased brain lactate and decreased brain glucose in patients with severe traumatic brain injury. Minerva Anestesiol 78:185–193
Shackford SR, Zhuang J, Schmoker J (1992) Intravenous fluid tonicity: effect on intracranial pressure, cerebral blood flow, and cerebral oxygen delivery in focal brain injury. J Neurosurg 76:91–98
Gordon GR, Choi HB, Rungta RL, Ellis-Davies GC, MacVicar BA (2008) Brain metabolism dictates the polarity of astrocyte control over arterioles. Nature 456:745–749
Marshall LF, Marshall SB, Klauber MR, van Clark Berkum M, Eisenberg HM, Jane JA, Luerssen TG, Marmarou A, Foulkes MA (1991) A new classification of head injury based on computerized tomography. J Neurosurg 75:S14–S20
Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, Schouten J, Shutter L, Timmons SD, Ullman JS, Videtta W, Wilberger JE, Wright DW (2007) Guidelines for the management of severe traumatic brain injury VIII. Intracranial pressure thresholds. J Neurotrauma 24(Suppl 1):S55–S58
Stewart PA (1978) Independent and dependent variables of acid-base control. Respir Physiol 33:9–26
Stocchetti N, Colombo A, Ortolano F, Videtta W, Marchesi R, Longhi L, Zanier ER (2007) Time course of intracranial hypertension after traumatic brain injury. J Neurotrauma 24:1339–1346
Roquilly A, Mahe PJ, Latte DD, Loutrel O, Champin P, Di Falco C, Courbe A, Buffenoir K, Hamel O, Lejus C, Sebille V, Asehnoune K (2011) Continuous controlled-infusion of hypertonic saline solution in traumatic brain-injured patients: a 9-year retrospective study. Crit Care 15:R260
Froelich M, Ni Q, Wess C, Ougorets I, Hartl R (2009) Continuous hypertonic saline therapy and the occurrence of complications in neurocritically ill patients. Crit Care Med 37:1433–1441
Prins ML (2008) Cerebral metabolic adaptation and ketone metabolism after brain injury. J Cereb Blood Flow Metab 28:1–16
Holloway R, Zhou Z, Harvey HB, Levasseur JE, Rice AC, Sun D, Hamm RJ, Bullock MR (2007) Effect of lactate therapy upon cognitive deficits after traumatic brain injury in the rat. Acta Neurochir (Wien) 149:919–927
Levasseur JE, Alessandri B, Reinert M, Clausen T, Zhou Z, Altememi N, Bullock MR (2006) Lactate, not glucose, up-regulates mitochondrial oxygen consumption both in sham and lateral fluid percussed rat brains. Neurosurgery 59:1122–1130
Rice AC, Zsoldos R, Chen T, Wilson MS, Alessandri B, Hamm RJ, Bullock MR (2002) Lactate administration attenuates cognitive deficits following traumatic brain injury. Brain Res 928:156–159
Berthet C, Lei H, Thevenet J, Gruetter R, Magistretti PJ, Hirt L (2009) Neuroprotective role of lactate after cerebral ischemia. J Cereb Blood Flow Metab 29:1780–1789
King P, Kong MF, Parkin H, MacDonald IA, Barber C, Tattersall RB (1998) Intravenous lactate prevents cerebral dysfunction during hypoglycaemia in insulin-dependent diabetes mellitus. Clin Sci (Lond) 94:157–163
Tsacopoulos M, Magistretti PJ (1996) Metabolic coupling between glia and neurons. J Neurosci 16:877–885
Belanger M, Allaman I, Magistretti PJ (2011) Brain energy metabolism: focus on astrocyte-neuron metabolic cooperation. Cell Metab 14:724–738
Prieto R, Tavazzi B, Taya K, Barrios L, Amorini AM, Di Pietro V, Pascual JM, Marmarou A, Marmarou CR (2011) Brain energy depletion in a rodent model of diffuse traumatic brain injury is not prevented with administration of sodium lactate. Brain Res 1404:39–49
Mustafa I, Leverve XM (2002) Metabolic and hemodynamic effects of hypertonic solutions: sodium-lactate versus sodium chloride infusion in postoperative patients. Shock 18:306–310
Leverve XM, Boon C, Hakim T, Anwar M, Siregar E, Mustafa I (2008) Half-molar sodium-lactate solution has a beneficial effect in patients after coronary artery bypass grafting. Intensive Care Med 34:1796–1803
Halestrap AP, Wilson MC (2012) The monocarboxylate transporter family–role and regulation. IUBMB Life 64:109–119
Kahle KT, Staley KJ, Nahed BV, Gamba G, Hebert SC, Lifton RP, Mount DB (2008) Roles of the cation-chloride cotransporters in neurological disease. Nat Clin Pract Neurol 4:490–503
Jourdain P, Pavillon N, Moratal C, Boss D, Rappaz B, Depeursinge C, Marquet P, Magistretti PJ (2011) Determination of transmembrane water fluxes in neurons elicited by glutamate ionotropic receptors and by the cotransporters KCC2 and NKCC1: a digital holographic microscopy study. J Neurosci 31:11846–11854
Bergsneider M, Hovda DA, Shalmon E, Kelly DF, Vespa PM, Martin NA, Phelps ME, McArthur DL, Caron MJ, Kraus JF, Becker DP (1997) Cerebral hyperglycolysis following severe traumatic brain injury in humans: a positron emission tomography study. J Neurosurg 86:241–251
Vespa P, Bergsneider M, Hattori N, Wu HM, Huang SC, Martin NA, Glenn TC, McArthur DL, Hovda DA (2005) Metabolic crisis without brain ischemia is common after traumatic brain injury: a combined microdialysis and positron emission tomography study. J Cereb Blood Flow Metab 25:763–774
Pannier JL, Demeester G, Leusen I (1974) The influence of nonrespiratory alkalosis on cerebral blood flow in cats. Stroke 5:324–329
Yoon S, Zuccarello M, Rapoport RM (2012) PCO(2) and pH regulation of cerebral blood flow. Front Physiol 3:365. doi:10.3389/fphys.2012.00365
Acknowledgments
This paper is dedicated to the memory of Professor Xavier Leverve, who provided the intellectual framework for this clinical study. Regrettably, he died on November 8th, 2010. The research team behind this work is honored to have worked under his superb guidance and vitality.
We thank Innogene Kalbiotech, Pte. Ltd (24 Raffles Place 27 - 06 Clifford Centre, Singapore 048621, Malaysia) for their gift of NaCl and half-molar sodium lactate solutions. The half-molar sodium lactate-containing solution is patented (WO 2004/096204 -11/11/04, Gazette 2004/46) and registered (Totilac™).
The trial was investigator driven. Half-molar sodium lactate solution was kindly provided by Innogene Kalbiotech, Singapore, Malaysia. The company had no role in the study design, data collection, data analysis, data interpretation or writing of the report.
Conflicts of interest
All authors had full access to all the study data, and all agreed to submit for publication. Professor Xavier Leverve was a member of the Innogene International Scientific Board of Advisors. The other authors declare no conflict of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
X. M. Leverve is deceased.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ichai, C., Payen, JF., Orban, JC. et al. Half-molar sodium lactate infusion to prevent intracranial hypertensive episodes in severe traumatic brain injured patients: a randomized controlled trial. Intensive Care Med 39, 1413–1422 (2013). https://doi.org/10.1007/s00134-013-2978-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2978-9