Abstract
Purpose
To report determinants and outcomes associated with decisions to deny or to delay intensive care unit (ICU) admission in critically ill patients.
Methods
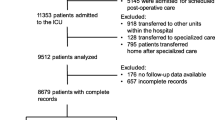
An observational prospective study over a 6-month period. All adult patients triaged for admission to a medical ICU were included prospectively. Age, gender, reasons for requesting ICU admission, severity of underlying disease, severity of acute illness, mortality and ICU characteristics were recorded. Multinomial logistic regression analysis was used for evaluating predicting factors of refused ICU admission.
Results
ICU admission was requested for 398 patients: 110 were immediately admitted (27.8%), 142 were never admitted (35.6%), and 146 were admitted at a later time (36.6%). The reasons for refusal were: too sick to benefit (31, 10.8%), too well to benefit (55, 19.1%), unit full (117, 40.6%), and more data about the patient were needed to make a decision (85, 29.5%). Multivariate analysis revealed that late ICU admission was associated with the lack of available ICU beds (OR 1.91; 95% CI 1.46–2.50; p = 0.003), cardiac disease (OR 7.77; 95% CI 2.41–25.04; p < 0.001), neurological disease (OR 3.78; 95% CI 1.40–10.26; p = 0.009), shock and sepsis (OR 2.55; 95% CI 1.06–6.13; p = 0.03), and metabolic disease (OR 2.84; 95% CI 1.11–7.30; p = 0.02). Factors for ICU refusal for never admitted patients were: severity of acute illness (OR 4.83; 95% CI 1.11–21.01; p = 0.03), cardiac disease (OR 14.26; 95% CI 3.95–51.44; p < 0.001), neurological disease (OR 4.05; 95% CI 1.33–12.28; p = 0.01) and lack of available ICU beds (OR 6.26; 95% CI 4.14–9.46; p < 0.001). Hospital mortality was 33.3% (37/110) for immediately admitted patients, 43.8% (64/146) for patients admitted later and 49.3% (70/142) for never admitted patients.
Conclusion
Refusal of ICU admission was correlated with the severity of acute illness, lack of ICU beds and reasons for admission request. Further efforts are needed to define which patients are most likely to benefit from ICU admission and to improve the accuracy of data on ICU refusal rates.


Similar content being viewed by others
References
Ip M, Galligan T, Koenig B, Raffin TA (1998) Ethical decision-making in critical care in Hong Kong. Crit Care Med 26:447–451
Scheinkestel CD (1996) The evolution of the intensivist: from health care provider to economic rationalist and ethicist. Med J Aust 164:310–312
Vincent JL (1996) European attitudes towards ethical problems in intensive care medicine/results of an ethical questionnaire. Intensive Care Med 16:256–264
Strauss MJ, LoGerfo JP, Yeltatzie JA, Temkin N, Hudson LD (1986) Rationing of intensive care unit services. Aneveryday occurrence. JAMA 255:1143–1146
Miller DH (1994) The rationing of intensive care. Crit Care Clin 10:135–143
Sprung CL, Geber D, Eidelman LA, Baras M, Pizov R, Nimrod A, Oppenheim A, Epstein L, Cotev S (1999) Evaluation of triage decisions for intensive care admission. Crit Care Med 27:1073–1079
Society of Critical Care Medicine Ethics Committee (1994) Attitudes of critical care medicine professionals concerning distribution of intensive care resources. Crit Care Med 22:358–362
Lyons RA, Wareham K, Hutchings HA, Major E, Ferguson B (2000) Population requirement for adult critical-care beds: a prospective quantitative and qualitative study. Lancet 355:595–598
Task Force of the Society of Critical Care Medicine SCCM (1999) Guidelines for intensive care unit admission, discharge, and triage. Crit Care Med 27:633–638
Bone RC, McElwee NE, Eubanks DH, Gluck EH (1993) Analysis of indications for intensive care unit admission: clinical efficiency assessment project: American College of Physicians. Chest 104:1806–1811
Consensus Development Panel (1983) Critical care medicine. JAMA 250:798–804
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ Jr, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA (1996) The effectiveness of right heart catheterization in the initial care of critically ill patients. JAMA 276:889–897
Society of Critical Care Medicine Ethics Committee (1994) Consensus statement on the triage of critically ill patients. JAMA 271:1200–1203
World Health Organization (2004–2007) Country cooperation strategy for WHO and Morocco 2004–2007. http://www.who.int/countries/en/cooperation_strategy_mar_en.pdf
McCabe WR, Jackson GG (1962) Gram negative bacteremia: etiology and ecology. Arch Intern Med 110:847–855
Lemeshow S, Teres D, Klar J, Spitz Avrunin J, Gehlbach SH, Rapoport J (1993) Mortality probability models (MPM II) based on an international cohort of intensive care unit patients. JAMA 270:2478–2486
Joynt GM, Gomersall CD, Tan P, Lee A, Ai Yu, Cheng C, Lai Yi Wong E (2001) Prospective evaluation of patients refused admission to intensive care unit: triage, futility and outcome. Intensive Care Med 27:1459–1465
Garrouste-Orgeas M, Montuclard L, Timsit JF, Reignier J, Desmettre T, Karoubi P, Moreau D, Montesino L, Duguet A, Boussat S, Ede C, Monseau Y, Paule T, Misset B, Carlet J, French ADMISSIONREA Study Group (2005) Predictors of intensive care unit refusal in French intensive care units: a multiple-center study. Crit Care Med 33:750–755
Reignier J, Dumont R, Katsahian S, Martin-Lefevre L, Renard B, Fiancette M, Lebert C, Clementi E, Bontemps F (2008) Patient-related factors and circumstances surrounding decisions to forego life-sustaining treatment, including intensive care unit admission refusal. Crit Care Med 36:2076–2083
Azoulay E, Pochard F, Chevret S, Vinsonneau C, Garrouste M, Cohen Y (2001) Compliance with triage to intensive care recommendations. Crit Care Med 29:2132–2136
Boumendil A, Somme D, Garrouste-Orgeas M, Guidet B (2007) Should elderly patients be admitted to the intensive care unit? Intensive Care Med 33:1252–1262
Metcalfe MA, Slogget A, McPherson K (1997) Mortality among appropriately referred patients refused admission to intensive-care units. Lancet 350:7–11
Frisho-Lima P, Gurman G, Schapira A, Porath A (1994) Rationing critical care-what happens to patients who are not admitted? Theor Surg 9:208–211
Garrouste-Orgeas M, Montuclard L, Timsit JF, Misset B, Christias M, Carlet J (2003) Triaging patients to the CIU: a pilot study of factors influencing admission decision and outcome. Intensive Care Med 29:774–781
Singer DE, Carr PL, Mulley AG, Thibault GE (1983) Rationing intensive care-physician responses to a resource shortage. N Engl J Med 309:1155–1160
Sinuff T, Kahnamoui K, Cook DJ, Luce JM, Levy MM, Ethics Values, Rationing in Critical Care Task Force (2004) Rationing critical care beds: a systematic review. Crit Care Med 32:1588–1597
Iapichino G, Corbella D, Minelli C, Mills GH, Artigas A, Edbooke DL, Pezzi A, Kesecioglu J, Patroniti N, Baras M, Sprung CL (2010) Reasons for refusal of admission to intensive care and in impact on mortality. Intensive Care Med 36:1772–1779
Nouira S, Roupie E, El Atrouss S, Durand-Zaleski I, Brun-Buisson C, Lemaire F, Abroug F (1998) Intensive care use in a developing country: a comparison between a Tunisian and French Unit. Intensive Care Med 24:1144–1151
Nouira S, Belghith M, Elatrous S, Jaafoura M, Ellouzi M, Boujdaria R, Gahbiche M, Bouchoucha S, Abroug F (1998) Predictive value of severity scoring systems: comparison of four models in Tunisia adult intensive care units. Crit Care Med 26:852–859
Topeli A, Laghui F, Tobin M (2005) Effect of closed unit policy and appointing an intensivist in a developing country. Crit Care Med 33:299–306
Parikh CR, Kamad DR (1999) Quality, cost and outcome of intensive care in a public hospital in Bombay, India. Crit Care Med 27:1754–1759
Abidi K, Belayachi J, Derras Y, Khayari ME, Dendane T, Madani N, Khoudri I, Zeggwagh AA, Abouqal R (2011) Eosinopenia, an early marker of increased mortality in critically ill medical patients. Intensive Care Med 37:1136–1142
Akkaoui M, Abidi K, Belayachi G et al (2009) Rate and modality of withdrawing and withholding of life-sustaining therapy in Moroccan medical intensive care Unit (Abstract). SRLF
Acknowledgments
We thank I. Khoudri, MD, for assistance with and reviewing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. Louriz and K. Abidi contributed equally to the work.
Rights and permissions
About this article
Cite this article
Louriz, M., Abidi, K., Akkaoui, M. et al. Determinants and outcomes associated with decisions to deny or to delay intensive care unit admission in Morocco. Intensive Care Med 38, 830–837 (2012). https://doi.org/10.1007/s00134-012-2517-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2517-0