Abstract
Purpose
Anticoagulation during renal replacement therapy remains an important challenge for burn patients due to their high risk of bleeding. In this study we compared the efficacy and safety of citrate anticoagulation to heparin anticoagulation for hemodiafiltration (HDF) in severe burn patients, focusing on metabolic tolerance and handling of citrate.
Methods
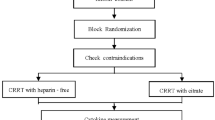
Retrospective observational study (January 2000–December 2007) at a university teaching hospital. Among 548 patients admitted with burns, 70 severe burn septic shock patients (median age 57.5 years, interquartile range 42–76 years; median burned surface area 40%, interquartile range 30–60%) who underwent HDF for more than 24 h were included.
Results
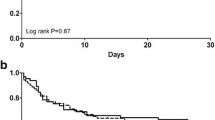
Of the 70 HDF patients, 31 at high risk of bleeding were treated with citrate and 39 with heparin, with a mortality rate of 70.9 and 71.8%, respectively. In continuous venovenous hemodiafiltration (CVVHDF), the filter survival was higher with citrate, and hemorrhagic complications were lower (0.035 vs. 0.145 episodes/day, respectively). During citrate CVVHDF [median delivered dialysis dose: 578.9 ml kg−1 day−1 (461.5–769.2 ml kg−1 day−1)] in catecholamine-supported patients (norepinephrine 0.53 μg kg−1 min−1), no metabolic derangements in pH, bicarbonates, Na+, K+, Ca++, and ionized calcium were observed. Systemic citratemia was within the normal range (<0.4 mmol/l) and was associated with a marked citrate removal in the effluent (5 patients, 36–60% of infused amount).
Conclusions
In septic shock burn patients, citrate for CVVHDF was efficient and safe, and superior to heparin for hemorrhagic complications and filter survival. Observed metabolic stability was most likely due to a marked loss of citrate in effluent volume and subsequent low total citrate load for the patient.


Similar content being viewed by others
References
Sheridan RL, Ryan CM, Yin LM, Hurley J, Tompkins RG (1998) Death in the burn unit: sterile multiple organ failure. Burns 24:307–311
Greenhalgh DG, Saffle JR, Holmes JH 4th, Gamelli RL, Palmieri TL, Horton JW, Tompkins RG, Traber DL, Mozingo DW, Deitch EA, Goodwin CW, Herndon DN, Gallagher JJ, Sanford AP, Jeng JC, Ahrenholz DH, Neely AN, O’Mara MS, Wolf SE, Purdue GF, Garner WL, Yowler CJ, Latenser BA; American Burn Association Consensus Conference on Burn Sepsis and Infection Group (2007) American Burn Association consensus conference to define sepsis and infection in burns. J Burn Care Res 28:776–790
Mustonen KM, Vuola J (2008) Acute renal failure in intensive care burn patients (ARF in burn patients). J Burn Care Res 29:227–237
Mariano F, Cantaluppi V, Stella M, Romanazzi GM, Assenzio B, Cairo M, Biancone L, Triolo G, Ranieri VM, Camussi G (2008) Circulating plasma factors induce tubular and glomerular alterations in septic burn patients. Crit Care 12:R42
Mariano F, Gangemi EN, Stella M, Tedeschi L, Gregoretti C, Triolo G (2009) Burns and acute renal failure. In: Ronco C, Bellomo R, Kellum JA (eds) Critical care nephrology, 2nd edn. Philadelphia, WB Saunders, pp 312–316
Davies MP, Evans J, McGonigle RJS (1994) The dialysis debate: acute renal failure in dialysis patients. Burns 20:71–73
Hubsher J, Olshan AR, Schwartz AB, Zoranski B, DeClement F, Bendlin A, Hensell D, Brezin JH, Krevolin LE, Chinitz JL (1986) Continuous arteriovenous hemofiltration for the treatment of anasarca and acute renal failure in severely burned patients. ASAIO Trans 32:401–404
Gueugniaud PY (1999) Apport de l’hemodiafiltration continue au traitement des bruleès graves. In: Journois D (ed) Hemofiltration continue. Elsevier, Paris, pp 209–219
Weksler N, Chorni I, Gurman G, Roy-Shapira A (1997) Improved survival with continuous veno-venous hemofiltration in nonoliguric burned septic patients [Abstract]. Blood Purif 15:137
Abdel-Rahman EM, Moorthy AV, Helgerson RB et al (1997) ARF requiring dialysis in patients with burns: 16 years’ experience in one center [abstract]. J Am Soc Nephrol 8:121A
Leblanc M, Thibeault Y, Querin S (1997) Continuous hemofiltration and hemodiafiltration for acute renal failure in severely burned patients. Burns 23:160–165
Holm C, Horbrand F, von Donnersmarck GH, Muhlbauer W (1999) Acute renal failure in severely burned patients. Burns 25:171–178
Tremblay R, Ethier J, Querin S, Beroniade V, Falardeau P, Leblanc M (2000) Veno-venous continuous renal replacement therapy for burned patients with acute renal failure. Burns 26:638–643
Hladlik M, Tymonova J, Zaoral T, Kadicik M, Adamkova M (2001) Treatment by continuous renal replacement therapy in patients with burns injuries. Acta Chir Plast 43:21–25
Mariano F, Tetta C, Stella M, Biolino P, Miletto A, Triolo G (2004) Regional citrate anticoagulation in critically ill patients treated with plasma filtration and adsorption. Blood Purif 22:313–319
Chung KK, Lundy JB, Matson JR, Renz EM, White CE, King BT, Barillo DJ, Jones JA, Cancio LC, Blackbourne LH, Wolf SE (2009) Continuous venovenous hemofiltration in severely burned patients with acute kidney injury: a cohort study. Crit Care 13:R62
Housinger TA, Brinkerhoff C, Warden GD (1993) The relationship between platelet count, sepsis, and survival in pediatric burn patients. Arch Surg 128:65–66
Monchi M, Berghmans D, Ledoux D, Canivet JL, Dubois B, Damas P (2004) Citrate vs. heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med 30:260–265
Kutsogiannis DJ, Gibney RT, Stollery D, Gao J (2005) Regional citrate versus systemic heparin anticoagulation for continuous renal replacement in critically ill patients. Kidney Int 67:2361–2367
Tolwani AJ, Prendergast MB, Speer RR, Stofan BS, Wille KM (2006) A practical citrate anticoagulation continuous venovenous hemodiafiltration protocol for metabolic control and high solute clearance. Clin J Am Soc Nephrol 1:79–87
Oudemans-van Straaten HM, Bosman RJ, Koopmans M, van der Voort PH, Wester JP, van der Spoel JI, Dijksman LM, Zandstra DF (2009) Citrate anticoagulation for continuous venovenous hemofiltration. Crit Care Med 37:545–552
Mariano F, Tetta C, Ronco C, Triolo G (2006) Is there a real alternative anticoagulant to heparin in continuous treatments? Expert Rev Med Devices 3:5–8
Dries DJ (2009) Management of burn injuries—recent developments in resuscitation, infection control and outcomes research. Scand J Trauma Resusc Emerg Med 17:14–27
Kramer L, Jordan B, Druml W, Bauer P, Metnitz PGH, for the Austrian Epidemiologic Study on Intensive Care, ASDI Study Group (2007) Incidence and prognosis of early hepatic dysfunction in critically ill patients—a prospective multicenter study. Crit Care Med 35:1099–1104
Martin PY, Chevrolet JC, Suter P, Favre H (1994) Anticoagulation in patients treated by continuous venovenous hemofiltration: a retrospective study. Am J Kidney Dis 24:806–812
De Pont AJ, Oudemans-van Straaten HM, Roozendaal KJ, Zandstra DF (2000) Nadroparin vs dalteparin anticoagulation in high volume, continuous venovenous hemofiltration: a double-blind, randomized, crossover study. Crit Care Med 28:421–425
Uchino S, Fealy N, Baldwin I, Morimatsu H, Bellomo R (2003) Pre-dilution vs. post-dilution during continuous veno-venous hemofiltration: impact on filter life and azotemic control. Nephron Clin Pract 94:c94–c98
Möllering H, Gruber W (1966) Determination of citrate with citrate lyase. Anal Biochem 17:369–376
Chadha V, Garg U, Warady BA, Alon US (2002) Citrate clearance in children receiving continuous venovenous renal replacement therapy. Pediatr Nephrol 17:819–824
Ahmad S, Yeo K, Jensen WM, Landicho D, Gregory B, Moritz J, Kenny M (1990) Citrate anticoagulation during in vivo simulation of slow hemofiltration. Blood Purif 8:177–182
Morgera S, Scholle C, Voss G, Haase M, Vargas-Hein O, Krausch D, Melzer C, Rosseau S, Zuckermann-Becker H, Neumayer HH (2004) Metabolic complications during regional citrate anticoagulation in continuous venovenous hemodialysis: single-center experience. Nephron Clin Pract 97:c131–c136
Joannidis M, Kountchev J, Rauchenzauner M, Schusterschitz N, Ulmer H, Mayr A, Bellmann R (2007) Enoxaparin vs. unfractionated heparin for anticoagulation during continuous veno-venous hemofiltration: a randomized controlled crossover study. Intensive Care Med 33:1571–1579
Ferguson REH, Critchfield A, LeClaire A, Ajkay N, Vasconez HC (2005) Current practice of thromboprophylaxis in the burn population: a survey study of 84 US burn centers. Burns 31:964–966
Faucher LD, Conlon KM (2007) Practice guidelines for deep venous thrombosis prophylaxis in burns. J Burn Care Res 28:661–663
Morgera S, Schneider M, Slowinski T, Vargas-Hein O, Zuckermann-Becker H, Peters H, Kindgen-Milles D, Neumayer HH (2009) A safe citrate anticoagulation protocol with variable treatment efficacy and excellent control of the acid-base status. Crit Care Med 37:2018–2024
Kramer L, Bauer E, Joukhadar C, Strobl W, Gendo A, Madl A, Gangl A (2003) Citrate pharmacokinetics and metabolism in cirrhotic and noncirrhotic critically ill patients. Crit Care Med 31:2450–2455
Meier-Kriesche HU, Gitomer JJ, Finkel KW, DuBose T (2001) Increased total to ionized calcium ratio during continuous venovenous hemodialysis with regional citrate anticoagulation. Crit Care Med 29:748–752
Hetzel GR, Taskaya G, Sucker C, Hennersdorf M, Grabensee B, Schmitz M (2006) Citrate plasma levels in patients under regional anticoagulation in continuous venovenous hemofiltration. Am J Kidney Dis 48:806–811
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mariano, F., Tedeschi, L., Morselli, M. et al. Normal citratemia and metabolic tolerance of citrate anticoagulation for hemodiafiltration in severe septic shock burn patients. Intensive Care Med 36, 1735–1743 (2010). https://doi.org/10.1007/s00134-010-1909-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1909-2