Abstract
Objective
The purpose of this study was to evaluate the efficacy and safety of the low molecular weight heparin enoxaparin as anticoagulant in continuous veno-venous hemofiltration (CVVH) compared with unfractionated heparin.
Design
Prospective randomized controlled crossover study.
Setting
Medical and Surgical Intensive Care Unit of a University Hospital.
Patients
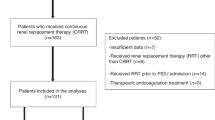
Forty consecutive adult medical and surgical ICU patients with normal anticoagulation parameters requiring CVVH.
Intervention
CVVH was performed with pre-filter fluid replacement at 2500 ml/h and blood flow rates of 180 ml/min. Heparin-treated patients received an initial pre-filter bolus of 30 IU/kg and a maintenance infusion at 7 units/kg h−1, titrated to achieve a systemic activated partial thromboplastin time (aPTT) of 40–45 s. Enoxaparin-treated patients received an initial pre-filter bolus of 0.15 mg/kg and a maintenance infusion starting at 0.05 mg/kg h−1, which was subsequently adjusted to maintain systemic anti-factor Xa activity (anti-Xa) at 0.25–0.30 IU/ml. Each patient received both regimens in a crossover design. Maximum treatment duration for each set was 72 h.
Results
Patients included had a mean APACHE II score of 22 (10–35). Thirty-seven patients completed both study arms. Mean filter life span was 21.7 h (± 16.9 h) for heparin and 30.6 h (± 25.3) for enoxaparin (p = 0.017, ANOVA for repeated measures). One major bleeding episode occurred during heparin as well as during enoxaparin treatment. Cost analysis showed average daily costs of 270 and 240 € for heparin and enoxaparin, respectively.
Conclusion
Enoxaparin can be safely used for anticoagulation during CVVH resulting in higher filter lifespan compared with unfractionated heparin.




Similar content being viewed by others
References
Ricci Z, Ronco C, D'Amico G, Felice R de, Rossi S, Bolgan I, Bonello M, Zamperetti N, Petras D, Salvatori G, Dan M, Piccinni P (2006) Practice patterns in the management of acute renal failure in the critically ill patient: an international survey. Nephrol Dial Transplant 21:690–696
Oudemans-van Straaten HM, Wester JP, Pont AC de, Schetz MR (2006) Anticoagulation strategies in continuous renal replacement therapy: can the choice be evidence based? Intensive Care Med 32:188–202
Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, Granger C, Ohman EM, Dalen JE (2001) Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest 119:64S–94S
Warkentin TE, Levine MN, Hirsh J, Horsewood P, Roberts RS, Gent M, Kelton JG (1995) Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractioned heparin. N Engl J Med 332:1330–1335
Anastassiades E, Ireland H, Flynn A, Lane DA, Curtis JR (1990) A low-molecular-weight heparin (Kabi 2165, 'Fragmin') in repeated use for haemodialysis: prevention of clotting and prolongation of the venous compression time in comparison with commercial unfractioned heparin. Nephrol Dial Transplant 5:135–140
Schrader J, Valentin R, Tonnis HJ, Hildebrand U, Stibbe W, Armstrong VW, Kandt M, Kostering H, Quellhorst E (1985) Low molecular weight heparin in hemodialysis and hemofiltration patients. Kidney Int 28:823–829
Bambauer R, Rucker S, Weber U, Kohler M (1990) Comparison of low molecular weight heparin and standard heparin in hemodialysis. ASAIO Trans 36:M646–M649
Deuber HJ, Schulz W (1991) Reduced lipid concentrations during four years of dialysis with low molecular weight heparin. Kidney Int 40:496–500
Elisaf MS, Germanos NP, Bairaktari HT, Pappas MB, Koulouridis EI, Siamopoulos KC (1997) Effects of conventional vs. low-molecular-weight heparin on lipid profile in hemodialysis patients. Am J Nephrol 17:153–157
Jeffrey RF, Khan AA, Douglas JT, Will EJ, Davison AM (1993) Anticoagulation with low molecular weight heparin (Fragmin) during continuous hemodialysis in the intensive care unit. Artif Organs 17:717–720
Pont AC de, Oudemans-van Straaten HM, Roozendaal KJ, Zandstra DF (2000) Nadroparin versus dalteparin anticoagulation in high-volume, continuous venovenous hemofiltration: a double-blind, randomized, crossover study. Crit Care Med 28:421–425
Reeves JH, Cumming AR, Gallagher L, O'Brien JL, Santamaria JD (1999) A controlled trial of low-molecular-weight heparin (dalteparin) versus unfractioned heparin as anticoagulant during continuous venovenous hemodialysis with filtration. Crit Care Med 27:2224–2228
Joannidis M, Kountchev J, Grote A, Bellmann R, Mayr AJ, Wiedermann CJ (2004) Unfractioned versus low-molecular-weight heparin(enoxaparin) for anticoagulation in CVVH. Intensive Care Med 30:S155 (Abstract)
Lemaire F, Bion J, Blanco J, Damas P, Druml C, Falke K, Kesecioglu J, Larsson A, Mancebo J, Matamis D, Pesenti A, Pimentel J, Ranieri M (2005) The European Union Directive on Clinical Research: present status of implementation in EU member states' legislations with regard to the incompetent patient. Intensive Care Med 31:476–479
Aguilar D, Goldhaber SZ (1999) Clinical uses of low-molecular-weight heparins. Chest 115:1418–1423
Levine MN, Planes A, Hirsh J, Goodyear M, Vochelle N, Gent M (1989) The relationship between anti-factor Xa level and clinical outcome in patients receiving enoxaparine low molecular weight heparin to prevent deep vein thrombosis after hip replacement. Thromb Haemost 62:940–944
Ireland H, Lane DA, Curtis JR (1984) Objective assessment of heparin requirements for hemodialysis in humans. J Lab Clin Med 103:643–652
Warkentin TE, Greinacher A (2004) Heparin-induced thrombocytopenia: recognition, treatment, and prevention: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126:311S–337S
Mayr AJ, Dunser M, Jochberger S, Fries D, Klingler A, Joannidis M, Hasibeder W, Schobersberger W (2002) Antifactor Xa activity in intensive care patients receiving thromboembolic prophylaxis with standard doses of enoxaparin. Thromb Res 105:201–204
Jochberger S, Mayr V, Luckner G, Fries DR, Mayr AJ, Friesenecker BE, Lorenz I, Hasibeder WR, Ulmer H, Schobersberger W, Dunser MW (2005) Antifactor Xa activity in critically ill patients receiving antithrombotic prophylaxis with standard dosages of certoparin: a prospective, clinical study. Crit Care 9:R541–R548
van de Wetering J, Westendorp RG, van der Hoeven JG, Stolk B, Feuth JD, Chang PC (1996) Heparin use in continuous renal replacement procedures: the struggle between filter coagulation and patient hemorrhage. J Am Soc Nephrol 7:145–150
Martin PY, Chevrolet JC, Suter P, Favre H (1994) Anticoagulation in patients treated by continuous venovenous hemofiltration: a retrospective study. Am J Kidney Dis 24:806–812
Kozek-Langenecker SA, Kettner SC, Oismueller C, Gonano C, Speiser W, Zimpfer M (1998) Anticoagulation with prostaglandin E1 and unfractioned heparin during continuous venovenous hemofiltration. Crit Care Med 26:1208–1212
Tan HK, Baldwin I, Bellomo R (2000) Continuous veno-venous hemofiltration without anticoagulation in high-risk patients. Intensive Care Med 26:1652–1657
Vargas HO, von Heymann C, Lipps M, Ziemer S, Ronco C, Neumayer HH, Morgera S, Welte M, Kox WJ, Spies C (2001) Hirudin versus heparin for anticoagulation in continuous renal replacement therapy. Intensive Care Med 27:673–679
Lim W, Dentali F, Eikelboom JW, Crowther MA (2006) Meta-analysis: low-molecular-weight heparin and bleeding in patients with severe renal insufficiency. Ann Intern Med 144:673–684
Brophy DF, Wazny LD, Gehr TW, Comstock TJ, Venitz J (2001) The pharmacokinetics of subcutaneous enoxaparin in end-stage renal disease. Pharmacotherapy 21:169–174
Chow SL, Zammit K, West K, Dannenhoffer M, Lopez-Candales A (2003) Correlation of antifactor Xa concentrations with renal function in patients on enoxaparin. J Clin Pharmacol 43:586–590
Becker RC, Spencer FA, Gibson M, Rush JE, Sanderink G, Murphy SA, Ball SP, Antman EM (2002) Influence of patient characteristics and renal function on factor Xa inhibition pharmacokinetics and pharmacodynamics after enoxaparin administration in non-ST-segment elevation acute coronary syndromes. Am Heart J 143:753–759
Nagge J, Crowther M, Hirsh J (2002) Is impaired renal function a contraindication to the use of low-molecular-weight heparin? Arch Intern Med 162:2605–2609
Gerlach AT, Pickworth KK, Seth SK, Tanna SB, Barnes JF (2000) Enoxaparin and bleeding complications: a review in patients with and without renal insufficiency. Pharmacotherapy 20:771–775
Cestac P, Bagheri H, Lapeyre-Mestre M, Sie P, Fouladi A, Maupas E, Leger P, Fontan B, Massip P, Montastruc JL (2003) Utilisation and safety of low molecular weight heparins: prospective observational study in medical inpatients. Drug Safety 26:197–207
Thorevska N, Amoateng-Adjepong Y, Sabahi R, Schiopescu I, Salloum A, Muralidharan V, Manthous CA (2004) Anticoagulation in hospitalized patients with renal insufficiency: a comparison of bleeding rates with unfractioned heparin vs. enoxaparin. Chest 125:856–863
Spinler SA, Inverso SM, Cohen M, Goodman SG, Stringer KA, Antman EM (2003) Safety and efficacy of unfractioned heparin versus enoxaparin in patients who are obese and patients with severe renal impairment: analysis from the ESSENCE and TIMI 11B studies. Am Heart J 146:33–41
Dodds A, Nicholls M (1983) Haematological aspects of renal disease. Anaesth Intensive Care 11:361–368
Fiaccadori E, Maggiore U, Clima B, Melfa L, Rotelli C, Borghetti A (2001) Incidence, risk factors, and prognosis of gastrointestinal hemorrhage complicating acute renal failure. Kidney Int 59:1510–1519
Martel N, Lee J, Wells PS (2005) Risk for heparin-induced thrombocytopenia with unfractioned and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood 106:2710–2715
Ronco C, Bellomo R, Homel P, Brendolan A, Dan M, Piccinni P, La Greca G (2000) Effects of different doses in continuous veno-venous haemofiltration on outcomes of acute renal failure: a prospective randomised trial. Lancet 356:26–30
Bouman CS, Oudemans-van Straaten HM, Tijssen JG, Zandstra DF, Kesecioglu J (2002) Effects of early high-volume continuous venovenous hemofiltration on survival and recovery of renal function in intensive care patients with acute renal failure: a prospective, randomized trial. Crit Care Med 30:2205–2211
DuBose TD Jr, Warnock DG, Mehta RL, Bonventre JV, Hammerman MR, Molitoris BA, Paller MS, Siegel NJ, Scherbenske J, Striker GE (1997) Acute renal failure in the 21st century: recommendations for management and outcomes assessment. Am J Kidney Dis 29:793–799
Acknowledgements
The study drug enoxaparin (Lovenox) was supplied at no charge by Aventis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Joannidis, M., Kountchev, J., Rauchenzauner, M. et al. Enoxaparin vs. unfractionated heparin for anticoagulation during continuous veno-venous hemofiltration: a randomized controlled crossover study. Intensive Care Med 33, 1571–1579 (2007). https://doi.org/10.1007/s00134-007-0719-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0719-7