Abstract
Background
Nutritional care in patients with a severe head injury is of utmost importance, as nutritional deficiency can affect the outcomes in these patients. The purpose of this study was to assess the feasibility, and an outcome of performing bedside percutaneous endoscopic gastrostomy in severe head injury patients. This study was conducted in a tertiary care institute. Patients with head injury with a Glasgow coma scale score ≤ 8 were included. Among 50 patients, 25 patients underwent percutaneous endoscopic gastrostomy and 25 patients underwent open feeding gastrostomy, within 72 h to up to 3 weeks from admission.
Results
The commonest subset in the study population was between18 and 30 years age group. Among 50 patients 43 (86%) were men and 7 (14%) were women with the men to women ratio being 6:1. The mean operative time for performing PEG was 12.04 SD 3.72 min, whereas for open feeding gastrostomy was 96.8 SD 9.98 min which was statistically significant (P = 0.0001). The complication rate for the PEG subgroup was 24% and that for feeding gastrostomy was 56% which was statistically significant (P = 0.02).
Conclusions
Percutaneous endoscopic gastrostomy is a minimally invasive and time-saving procedure, which is superior to open feeding gastrostomy in terms of a prerequisite of anaesthesia, operating room, and few post-operative complications.
Similar content being viewed by others
Background
Trauma is the leading cause of morbidity and mortality in India and other developing countries (Epidemiology of traumatic brain injuries: Indian scenario 2017). Head injury patients with poor Glasgow coma scale (GCS) require early nutritional support along with other treatment for head injury for better outcomes. Parenteral and enteral are the preferred routes of initiation of nutrition. Patients with head injuries may require long-term nutritional support; parenteral nutrition is not cost-effective and is associated with the risk of infection. Conventionally enteral nutrition is initiated using nasogastric feed or performing open surgical gastrostomy or jejunostomy. Nasogastric tube feed owing to the possibility of aspiration cannot be used for the long term, and surgical creation of gastrostomy and jejunostomy requires general anaesthesia and operating room. Bedside percutaneous endoscopic gastrostomy (PEG) is a safe and effective solution for maintaining enteral nutrition in critical head injury patients. Bedside PEG procedures can safely and effectively overcome the problems associated with the other procedures. We present our result comparing bedside PEG versus the conventional open feeding procedure for head injury cases in a tertiary care institute.
Methods
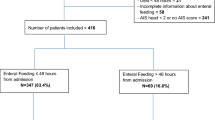
This study was conducted in tertiary care hospital from June 2015 to November 2017. This study was approved by Ethics committee for academic research projects (ECARP) PG Academic committee, T.N.Medical College & BYL Nair charitable hospital (ECARP/133). Patients with head injury and GCS score ≤ 8 were included (n = 50) in the study. Selected patients randomly divided in open feeding gastrostomy group (n = 25) and percutaneous endoscopic gastrostomy group (n = 25).
Inclusion criteria:
-
1.
Head injury patients with age > 18 years.
-
2.
Head injury patients with GCS score ≤ 8.
Exclusion criteria:
-
1.
Age < 18 years.
-
2.
Patient with a coagulation disorder.
-
3.
Patients with moderate to severe ascites.
-
4.
Patient with suspected peritonitis and gastric outlet obstruction.
All patients underwent feeding procedures within 72 h to up to 3 weeks from admission were included. In the surgical enteral nutrition group, a Stamm’s gastrostomy was performed under general anaesthesia in an operating room. A 20 or 22 French Foleys catheter was used for tube feeding. Percutaneous endoscopic gastrostomy procedures were performed bedside in the intensive care unit with all aseptic precautions using intravenous propofol and local anaesthesia with 2% lignocaine at the incision site. A Pull—through (Ponsky) technique for performing PEG was adapted (Ponsky and Gauderer 1981; Gauderer et al. 1980). A standard percutaneous endoscopic gastrostomy kit containing 24 French high-grade silicone tubes was used for the procedure. Both patient subgroup parameters were recorded, and outcomes were analysed.
Results
In the present study, 50 patients with severe head injury needing feeding procedures were analysed. Patients underwent open feeding gastrostomy (n = 25) and the other patients a bedside PEG (n = 25) randomly. Both the groups were similar in demographic deposition and head injury severity. Male preponderance was seen, in both groups as in our country males tend to undertake more outdoor activities and there is an increased incidence of alcohol consumption among males. (Table 1).
Patients with head injuries were classified depending on their GCS score. Most of the head injury patients had a GCS score of 5–7. There was no statistically significant difference in the GCS and time interval between admission and patients undergoing either procedure. The mean operative time for PEG was 12.04 SD 3.72 min, whereas for open feeding gastrostomy it was 96.8 SD9.98 min, which was statistically significant (P = 0.0001). The complication rate for PEG was 24%, and that for open feeding gastrostomy was 56%, which was also statistically significant (P = 0.02). The most common complication was surgical site infection in 12% of cases. Other complications were tube blockage in 8% cases, Peristomal leakage in 6% cases, inadvertent tube removal in 4% cases, gastrostomy site bleeding in 4% cases, a buried bumper syndrome in 2% cases, and peritonitis in 2% cases (Table 2).
Discussion
Head injury leads to increased metabolic rate, which increases the nutritional demand (Foley et al. 2008). Activation of the neuroendocrine system results in metabolic disturbances like high catabolism, hyperglycemia, and high proteolysis (Shu et al. 2000). Commencement of early nutritional support alleviates such conditions. Early enteral feeding helps to prevent gut mucosal atrophy, ileus, bacterial translocation, and early sepsis (Alverdy et al. 1985; Deitch et al. 1987, 1990). Early enteral feeding should begin as soon as the patient is hemodynamically stable. The calorie intake should be 30–35 kcal /kg/ body wt and protein content of 1.5–2.5gm/kg/ body weight (Mahapatra 2019). Nutrition to head injury patients can be provided by the parenteral or enteral route, with the latter being more physiological. The enteral route is preferred due to the reduced risk of hyperglycemia, infection, and it is cost-effective. The traditional approach for enteral feeding was by nasogastric tube or surgically placed gastrostomy tubes. Patients who are unable to tolerate gastric feeding may benefit from post-pyloric feeding by nasojejunal tube or surgical feeding jejunostomy. Nasally inserted fine bore devices for feeding are safe and easy to insert, however malposition, clogging, and dislodgment are common complications. Up to 50% of nasoenteric feeding tubes get dislodged eventually in agitated or inadequately sedated patients (Young et al. 1987). Also, prolonged use of nasoenteric feeding devices is associated with the risk of sinusitis and aspiration pneumonia. In head injury patient requiring long-term enteral nutrition, more secure access is needed in the form of surgical gastrostomy or jejunostomy. These procedures are carried out under anaesthesia and necessitate laparotomy in an operating room. Surgical procedures carry the risk of complications and are not suitable in patients with a high risk of anaesthesia. Percutaneous endoscopic gastrostomy was introduced in 1980 as an alternative to laparotomy, for the placement of a gastrostomy tube by using an endoscope (Gauderer et al. 1980). This can be accomplished at the bedside without the need for general anaesthesia and operating room. PEG is particularly well tolerated by patients who are high-risk candidates for general anaesthesia and surgery. Bedside PEG is safe, easy to perform, has low morbidity, and is successful in over 95% of patients (Grant 1988). In our study, complication rate for PEG was 24%, and that for open feeding gastrostomy was 56%, which was comparable to study conducted by Grant J P, similarly in our study mean operative time for PEG was 12.04 min, whereas for open feeding gastrostomy it was 96.8 min, which was comparable to study done by Grant (1988). However, coagulopathy, peritonitis, gastric outlet obstruction, and sepsis were contraindications for PEG (Rahnemai-Azar et al. 2014).
In our set up due to the superiority of the percutaneous endoscopic gastrostomy placement, it has replaced most traditional open feeding gastrostomy procedures, unless it is planned simultaneously during craniotomy in same anaesthesia setting. Another aspect of bedside PEG is cost-effectiveness in comparison to open surgical feeding procedures however, that aspect was beyond the scope of the present study since both procedures were performed free of cost for patients treated at our institution.
Conclusions
Nutrition is a somewhat neglected aspect in the management of head injury patients. The traditional forms of enteral nutrition are associated with procedure-related issues. Percutaneous endoscopic gastrostomy is a minimally invasive and time-saving procedure; which is superior to open feeding gastrostomy in terms of necessity of anaesthesia, operating room, and post-operative complications.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Abbreviations
- GCS:
-
Glasgow coma Scale
- PEG:
-
Percutaneous endoscopic gastrostomy
References
Alverdy J, Chi HS, Sheldon GF (1985) The effect of parenteral nutrition on gastrointestinal immunity The importance of enteral stimulation. Ann Surg 202:681–684
Deitch EA, Winterton J, Li M, Berg R (1987) The gut as a portal of entry for bacteremia. Role of protein malnutrition. Ann Surg 205:681–692
Deitch EA, Ma WJ, Ma L, Berg RD, Specian RD (1990) Protein malnutrition predisposes to inflammatory-induced gut-origin septic states. Ann Surg 211:560–567 (discussion 560–567)
Epidemiology of traumatic brain injuries: Indian scenario (2017) Available from: https://www.researchgate.net/publication/11574079. Accessed 15 Nov 2017
Foley N, Marshall S, Pikul J, Salter K, Teasell R (2008) Hypermetabolism following moderate to severe traumatic acute brain injury: a systematic review. J Neurotrauma 25(12):1415–1431. https://doi.org/10.1089/neu.2008.0628
Gauderer MW, Ponsky JL, Izant RJ (1980) Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatric Surg 15:872–875
Grant JP (1988) Comparison of percutaneous endoscopic gastrostomy with stamm gastrostomy from the department of surgery, Duke University Medical Center, Durham, North Carolina. Ann Surg 207(5):598–603
Mahapatra A (2019) Role of nutrition in head injury patient. Acta Sci Nutr Health 3(9):111–114
Ponsky JL, Gauderer MWL (1981) Percutaneous endoscopic gastrostomy: a non operative technique for feeding gastrostomy. Gastrointest Endosc 27:9–11
Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT (2014) Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol 20(24):7739–7751
Shu YY, Gao SF, Che LH (2000) The risk factors of hypoproteinemia secondary to acute brain injury. J Chin Crit Care Med 12(5):308–309
Young B, Ott L, Twyman D et al (1987) The effect of nutritional support on outcome from severe head injury. J Neurosurg 67:668–676
Acknowledgements
Author would like to thank all staff members of trauma intensive care unit for their valuable support and faculty members of surgery department for guidance.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Material preparation, data collection done by HS, RW, and AA. MS and SS analysed and interpreted data. The first draft of the manuscript was written by SS and DB. All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics and consent to participate
This study was approved by Ethics committee for academic research projects (ECARP) PG Academic committee, T.N.Medical College & BYL Nair charitable hospital (ECARP/133). All the procedures performed in this study involving patients were approved by institutional ethics committee for academic research projects and performed in accordance with the ethical standards laid down in ICH- GCP (1996), Indian GCP (2001) and ICMR guideline for biomedical research in human participant (2006). Waiver of consent to collect clinical data was obtained from institutional Ethics committee for academic research projects (ECARP) PG academic committee, T.N.Medical College & BYL Nair charitable hospital.
Consent for publication
Waiver of consent to collect clinical data and publication was obtained from institutional ethics committee for academic research projects (ECARP) PG academic committee, T.N.Medical College & BYL Nair charitable hospital.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Balsarkar, D., Shaikh, H., Suryawanshi, S. et al. Analysis of feasibility and outcome of bedside percutaneous endoscopic gastrostomy versus open feeding gastrostomy in head injury patients. Bull Natl Res Cent 46, 161 (2022). https://doi.org/10.1186/s42269-022-00855-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42269-022-00855-4