Abstract
Purpose
To investigate whether angiopoietin-2, von Willebrand factor (VWF) and angiopoietin-1 relate to surrogate indicators of vascular permeability, pulmonary dysfunction and intensive care unit (ICU) mortality throughout the course of septic shock.
Methods
In 50 consecutive mechanically ventilated septic shock patients, plasma angiopoietin-2, VWF and angiopoietin-1 levels and fluid balance, partial pressure of oxygen/inspiratory oxygen fraction and the oxygenation index as indicators of vascular permeability and pulmonary dysfunction, respectively, were measured until day 28.
Results
Angiopoietin-2 positively related to the fluid balance and pulmonary dysfunction, was higher in non-survivors than in survivors and independently predicted non-survival throughout the course of septic shock. VWF inversely related to the fluid balance and pulmonary dysfunction throughout the course of septic shock, was comparable between survivors and non-survivors and predicted non-survival on day 0 only. Angiopoietin-1 positively related to pulmonary dysfunction throughout the course, but did not differ between survivors and non-survivors.
Conclusions
In contrast to VWF, plasma angiopoietin-2 positively relates to fluid balance, pulmonary dysfunction and mortality throughout the course of septic shock, in line with a suggested mediator role of the protein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excessive and sustained activation of the endothelium resulting in increased vascular permeability is a crucial process during sepsis [1, 2]. In the lung, the loss of plasma fluid into the interstitial space leads to pulmonary oedema, injury and dysfunction associated with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) [1, 3]. Several clinical studies demonstrated that circulating levels of angiopoietin-2 (Ang-2) are elevated at the onset of critical illness in septic and non-septic patients with or at risk for ALI/ARDS, relate to vascular permeability and pulmonary dysfunction and are associated with intensive care unit (ICU) mortality [4–12]. It is not surprising that Ang-2 is a marker of those processes, since pre-formed Ang-2 can be released from the endothelial Weibel-Palade bodies during endothelial activation [13]. Another well-known marker of endothelial activation and dysfunction is von Willebrand factor (VWF), which is a major constituent of the Weibel-Palade body [13, 14]. We previously showed that Ang-2 and VWF levels are simultaneously enhanced in the plasma of ALI/ARDS or sepsis patients on admission to the ICU or onset of sepsis, suggesting that they are released together upon activation of the endothelium [12]. This may explain why both Ang-2 and VWF levels are associated with vascular permeability and pulmonary dysfunction [4–6, 8, 11, 12], even though VWF may not be directly involved in permeability [15, 16].
Experimental studies demonstrated that angiopoietin-1 (Ang-1) and Ang-2 bind to the endothelial Tie2 receptor [17–19]. Ang-1-induced activation of the Tie2 receptor results in vascular stabilisation [20–22]. Ang-2 provokes pulmonary inflammation and vascular leakage partly because of inhibition of the stabilising effect of Ang-1 by preventing Ang-1 from binding the Tie2 receptor [4, 5, 8, 10–12, 23, 24]. These experimental data together with clinical observations [4, 6, 7, 9, 11, 12] suggest that Ang-2 is not only a marker, but also a direct mediator in the pathogenesis of vascular permeability, pulmonary injury and dysfunction. This idea would be further reinforced if the relation between Ang-2, vascular permeability and pulmonary dysfunction persists throughout the course of critical illness in a homogeneous population of septic shock patients, more than VWF and Ang-1 levels. Up till now, the course and clinical correlates of Ang-2 have not been studied, and the predictive value of changes in Ang-2 during the course of septic shock for mortality is unknown. It has been hypothesised that the levels typically decrease in septic survivors and increase in septic patients that do not survive [5]. Only one study reported on the course of Ang-2 levels in multi-trauma patients [9], but clinical correlates were not studied.
The aims of our study were (1) to investigate whether Ang-2, VWF and Ang-1 relate to surrogate indicators of vascular permeability and pulmonary dysfunction throughout the course of septic shock and (2) to study the course of Ang-2, VWF and Ang-1 levels in survivors and non-survivors and their predictive value for ICU mortality. Therefore, we measured plasma levels of Ang-2, VWF and Ang-1, and recorded fluid balance as surrogate indicator of vascular permeability [25–28] and partial pressure of oxygen in arterial blood/inspiratory oxygen fraction (P aO2/F iO2), oxygenation index [29], pulmonary compliance and ventilator-dependency [30] as surrogate indicators of pulmonary dysfunction, respectively, throughout the course of septic shock.
Materials and methods
The local ethics committee approved this observational study and waived the need for informed consent. Fifty consecutive mechanically ventilated critically ill patients with community or ICU-acquired septic shock admitted to the ICU of the Radboud University Medical Centre (Nijmegen, The Netherlands) between January 2005 and September 2007 were included within 12 h after meeting septic shock criteria. Sepsis was defined by two or more of the following: abnormal body temperature (<36 or >38.5°C), tachycardia (>90/min), tachypnea [>20/min or partial pressure of CO2 in arterial blood (PaCO2) <32 mmHg], abnormal white blood cell counts (<4 or >12 × 109/l) and a microbiologically proven or clinically evident source of infection [29]. Septic shock was defined as sepsis complicated by acute circulatory failure characterised by persistent arterial hypotension unexplained by other causes [31]. Hypotension was defined by systolic arterial pressure <90 mmHg or mean arterial pressure (MAP) <70 mmHg for at least 1 h despite adequate fluid resuscitation or requirement of vasopressor support to maintain MAP [31]. ICU-acquired sepsis was defined as sepsis developing after 2 days in the ICU. The origin of septic shock was defined by clinical signs and symptoms and positive local and/or blood cultures. Patients were pressure-controlled or volume-controlled (after surgery) ventilated with a Galileo (Hamilton Medical AG; Rhäzüns, Switserland) or a Servo ventilator (Maquet, Inc.; Bridgewater, NJ). Patients with ALI/ARDS were pressure-controlled ventilated with a tidal volume (V t) aiming not to exceed 8 ml/kg and resulting in an end-tidal CO2 concentration between 4 and 5%, using an O2–air mixture with a F iO2 of 40% and a positive end-expiratory pressure (PEEP) of 5 cmH2O (inspiration:expiration 1:2) or more, when needed, guided by P aO2 (>60 mmHg). Patients were followed until death or discharge from the hospital. The 28-day ICU mortality, total ICU mortality and hospital mortality were recorded. Patients were treated by intensive care physicians not involved in the study according to institutional guidelines. Platelets were infused when the platelet count had dropped below 10–20 × 109/l, possibly as a result of diffuse intravascular coagulation, and when there were foci with a bleeding tendency.
On the inclusion day (day 0), demographics and clinical data were recorded including the Acute Physiology and Chronic Health Evaluation (APACHE) II score. The number of failing organs was scored. On day 0, day 7 ± 1 days, day 14 ± 2 days and day 28 ± 3 days, arterial blood samples were obtained for determinations of pH, P aO2 and P aCO2, white blood cell counts and creatinine. The respiratory frequency, tidal volume (V t), F iO2, plateau pressure (P plat), mean airway pressure (P mean) and PEEP were taken from the ventilator. The oxygenation index, which is a measure of oxygenation impairment for the intensity of mechanical ventilation, was calculated from (P mean × F iO2 × 100)/P aO2 [29]. Total respiratory dynamic compliance was calculated from V t/(plateau pressure-PEEP). Ventilator-free days were defined as follows: ventilator-free days = 0 if the patient dies before ICU day 28; ventilator-free days = 28 − x if the patient is successfully weaned from mechanical ventilation within 28 days, where x is the number of days spent on mechanical ventilation; ventilator-free days = 0 if the patient requires mechanical ventilation for 28 days or more [30]. Days at which a patient was ventilator-dependent were recorded. ALI and ARDS were characterised by P aO2/F iO2 ≤300 or ≤200 mmHg, respectively, and absence of clinical evidence of left atrial hypertension and congestive heart failure, according to the American European Consensus Criteria [32]. Vasopressor/inotropic treatment and body temperature were recorded. The fluid balance was calculated by dividing total fluid input minus total fluid output by the pre-ICU patient weight in kilograms [25–28]. Circulating Ang-2, VWF and Ang-1 were measured as described in the electronic supplementary material (ESM). The statistical analysis is described in the ESM.
Results
Patient characteristics
Patients were grouped as ICU survivor or non-survivor (Table 1, ESM Table 1). All ICU non-survivors, except one (death on day 68), died before ICU day 28. Five ICU survivors died in the hospital at a median 24 (range 2–60) days after discharge from the ICU. ICU survivors and non-survivors were comparable with respect to baseline demographics and with respect to clinical characteristics, except for APACHE II score and hospital stay, which were higher and shorter, respectively, in non-survivors compared to survivors. Twenty-two survivors and 14 non-survivors suffered from ALI/ARDS (Table 1). Haemodynamic, biochemical and respiratory characteristics are reported in the ESM.
Angiopoietin and VWF levels, fluid balance and pulmonary dysfunction
Patients had higher Ang-2 and VWF levels on day 0 [median (interquartile range) 2,350 (1,400–4,280) pg/ml and 289 (166–411)% of reference, respectively] than controls [113 (27–287) pg/ml, P < 0.001 and 93 (87–113)% of reference, P < 0.001, respectively]. Patients had lower Ang-1 levels on day 0 [330 (114–1,020) pg/ml] than controls [2,407 (969–3,730) pg/ml, P < 0.001]. Ang-2 levels related positively to the fluid balance throughout the course of septic shock after exclusion of one non-survivor who had extremely high Ang-2 levels (β = 0.20, P = 0.043 in GEE, r = 0.30, P = 0.005). Furthermore, Ang-2 levels related to indicators of pulmonary dysfunction throughout the course of septic shock, as demonstrated by an inverse relation with the P aO2/F iO2 ratio (β = −0.25, P < 0.001 in GEE; r = −0.25, P = 0.012), a positive relation with the oxygenation index (β = 0.37, P < 0.001 in GEE; r = 0.26, P = 0.017), a weak inverse relation with the compliance (β = −0.09, P = 0.004 in GEE; r = −0.05, P = 0.645) and a positive relation with ventilator-dependency (P = 0.043 in GEE). In contrast, VWF inversely related to the fluid balance (β = −0.21, P = 0.045 in GEE; r = −0.27, P = 0.014), positively related to the compliance (β = 0.21, P = 0.011 in GEE; r = 0.17, P = 0.134) and did not relate to the other respiratory variables throughout the course of septic shock. Ang-1 levels did not relate to the fluid balance, but related to indicators of pulmonary dysfunction throughout the course of septic shock, as demonstrated by an inverse relation with the P aO2/F iO2 ratio (β = −0.26, P = 0.022 in GEE; r = −0.21, P = 0.034) and a positive relation with the oxygenation index (β = 0.37, P = 0.005 in GEE; r = 0.28, P = 0.014) throughout the course of septic shock. The fluid balance related to indicators of pulmonary dysfunction throughout the course of septic shock, as demonstrated by an inverse relation with the P aO2/F iO2 ratio (β = −0.24, P < 0.001 in GEE; r = −0.29, P = 0.006), a positive relation with the oxygenation index (β = 0.22, P = 0.006 in GEE; r = 0.22, P = 0.068) and an inverse relation with the compliance (β = −0.26, P = 0.006 in GEE; r = −0.29, P = 0.014).
The course of the angiopoietin and VWF levels in survivors and non-survivors
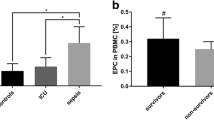
Ang-2 levels were higher in non-survivors than in survivors throughout the course of septic shock (Fig. 1). Ang-2 levels decreased in survivors from day 0 to the last ICU day, while they did not change in non-survivors (Figs. 1, 2). The course of VWF levels differed between survivors and non-survivors (Fig. 1), since VWF levels increased in survivors from day 0 to the last ICU day, while they did not change in non-survivors (Fig. 2). Ang-2 levels related to VWF levels on day 0, but the relation was lost throughout the course of septic shock (Fig. 3). Ang-1 levels were comparable between survivors and non-survivors (Fig. 1) and did not change from day 0 to the last ICU day (Fig. 2). The predictive value of angiopoietin and VWF levels for ICU mortality is described in the ESM.
The course of angiopoietin and VWF levels in survivors and non-survivors. Median and interquartile range of a circulating angiopoietin-2 (Ang-2; pg/ml), b von Willebrand factor (VWF; % of reference) and c angiopoietin-1 (Ang-1) levels (pg/ml) in plasma of intensive care unit (ICU) survivors (open circle) and ICU non-survivors (filled circle) on day 0, 1, 2, 4 and 7. Days 14, 21 and 28 are not shown because of low numbers, but are included in the analysis. a Ang-2 levels tended to be higher in non-survivors than in survivors throughout the course of septic shock (P = 0.199 for survivor vs. non-survivor and P = 0.028 for interaction between day and survivor vs. non-survivor). One non-survivor had extremely high Ang-2 levels: day 0 125,100 pg/ml; day 1 149,000 pg/ml; day 2 114,300 pg/ml; day 4 115,550 pg/ml and day 7 116,800 pg/ml. Therefore, the upper limit of interquartile range at day 7 is 88,263 pg/ml. Analysis without this non-survivor yields a P = 0.039 for survivor versus non-survivor and P = 0.016 for the interaction between day and survivor versus non-survivor. b VWF levels did not differ between survivors and non-survivors throughout the course of septic shock (P = 0.545 for survivor vs. non-survivor and P = 0.218 for interaction between day and survivor vs. non-survivor). c Ang-1 levels did not differ between survivors and non-survivors throughout the course of septic shock (P = 0.189 for survivor vs. non-survivor and P = 0.070 for interaction between day and survivor vs. non-survivor)
Angiopoietin and VWF levels on day 0 and the last ICU day in survivors and non-survivors. Individual levels and box plot of a circulating angiopoietin-2 (Ang-2; pg/ml), b von Willebrand factor (VWF; % of reference) and c angiopoietin-1 (Ang-1) levels (pg/ml) on day 0 and the last intensive care unit (ICU) day in ICU survivors and ICU non-survivors. Values in boxes are at 25th percentile, median and 75th percentile; whiskers are 10th and 90th percentile. a Ang-2 levels decreased from day 0 to the last ICU day in survivors (*P = 0.0033, n = 35 pairs), while they did not change in non-survivors (P = 0.3910, n = 15 pairs). Data not shown: Day 0 survivor: 25,090 pg/ml; day 0 non-survivor: 17,980 and 125,100 pg/ml; last ICU day non-survivor: 12,050 and 116,800 pg/ml; 90th percentile of non-survivors day 0: 60,828 pg/ml; 90th percentile of non-survivors last ICU day: 53,950 pg/ml. b VWF levels increased from day 0 to the last ICU day in survivors (*P = 0.0057, n = 35 pairs) and did not change in non-survivors (P = 0.5070, n = 14 pairs). c Ang-1 levels did not differ between day 0 and the last ICU day in survivors (P = 0.1044, n = 35 pairs) or non-survivors (P = 0.7612, n = 14 pairs)
The relation between Ang-2 and VWF levels. Angiopoietin-2 (Ang-2) levels (pg/ml) positively related to von Willebrand factor (VWF) levels (% of reference) at day 0 (filled circle, r = 0.45, P = 0.001, black line). Ang-2 levels throughout the course of septic shock did not relate to VWF levels (open circle day 1, day 2, day 4, day 7, day 14, day 21 and day 28, r = 0.10, P = 0.1190, dotted line)
Discussion
This study demonstrates that circulating Ang-2 positively relates to the fluid balance, pulmonary dysfunction and mortality throughout the course of septic shock. This is in line with the suggested mediator role of Ang-2 in those patients. In contrast, VWF was not positively related to the fluid balance and pulmonary dysfunction and predicted mortality only at the day of ICU admission, suggesting that VWF plays a marker role only in the early phase of septic shock. Indeed, circulating VWF and Ang-2 were related at day 0, but not throughout the course of septic shock.
Experimental data [5, 19, 23] together with several observations in patient studies [4–9, 11, 12, 25] suggest that Ang-2 is a mediator in the pathogenesis of pulmonary vascular permeability and injury. This hypothesis is reinforced by several aspects of the present study. First, the relation between circulating Ang-2 and the fluid balance or pulmonary dysfunction persisted throughout the course of septic shock. Second, this longitudinal relation was Ang-2-specific, since VWF, which is also considered a marker of endothelial activation and dysfunction, did not reflect a positive fluid balance and pulmonary dysfunction. Third, the relation was observed within a relatively homogeneous group of septic patients with high Ang-2 levels and severe vascular permeability and pulmonary dysfunction, while previous studies focused on heterogeneous populations [4–7, 10–12]. In those heterogeneous populations, Ang-2, vascular permeability and pulmonary dysfunction may be related due to a group effect, because non-septic patients have low Ang-2 levels and moderate vascular permeability or pulmonary dysfunction, while septic patients have high Ang-2 levels and severe vascular permeability or pulmonary dysfunction. Nevertheless, in vivo Ang-2 blocking studies are necessary to formally confirm the mediator role of Ang-2.
Ang-2 levels at day 0 and throughout the course had independent predictive value for 28 day survival, in accordance with a previous study [10], since patients with Ang-2 levels <3,066 pg/ml had longer survival duration than patients with Ang-2 levels ≥3,066 pg/ml, independent of the APACHE II score. Nevertheless, these cutoff values were selected post-hoc and should be validated prospectively. It has been proposed previously that circulating Ang-2 levels may better predict mortality of critically ill patients than the APACHE II score [7, 11]. For instance, Siner et al. [11] reported that there were no deaths among patients with Ang-2 levels less than 10,000 pg/ml, despite a predicted mortality of 16% based on the median APACHE II score. Indeed, the combination of Ang-2 and the APACHE II score had more predictive value than the APACHE II score alone. In our patient group, we did not observe a sharp increase in Ang-2 levels towards the day of death as was described for one patient by Parikh et al. [5]. Ang-2 was continuously higher in non-survivors compared to survivors. Interestingly, Ang-2 levels in survivors, which were already lower throughout the course, decreased from day 0 to the last ICU day. In this light, Ang-2 levels above a certain threshold may mediate the development of endothelial activation and dysfunction, associated with pulmonary dysfunction and mortality. Surprisingly, Ang-1 levels also positively related to pulmonary dysfunction. Nevertheless, Ang-1 levels in our septic shock patients were still much lower than Ang-1 levels in healthy controls according to the literature [10, 12], suggesting that the low Ang-1 levels did not offset the effects of high Ang-2 levels. Indeed, the Ang-2/Ang-1 ratio did not relate to the fluid balance or pulmonary dysfunction and mortality (data not shown).
VWF levels related inversely to the fluid balance and positively to the pulmonary compliance throughout the course of septic shock. This finding is in accordance with studies that did not find a predictive value for the development of ALI/ARDS [33, 34], while other studies reported that VWF levels at the onset of critical illness predicted the development of ALI/ARDS and related to pulmonary permeability [12, 35]. It is unclear how these differences can be explained, but the predictive value of VWF might depend on the time at which the samples were taken during the course of sepsis or ALI/ARDS. Indeed, VWF had predictive value for mortality early in the course of sepsis and ALI/ARDS (day 0), as reported by most [15, 16, 33, 35], but not all prior studies [36], but lost its predictive value on the subsequent days. Although VWF may thus have an important early prognostic role, the data do not suggest a direct pathogenetic role of the factor, in contrast to Ang-2.
In our study, increased Ang-2 and VWF levels were related on day 0 as reported before [8, 12], suggesting that they were released together from the endothelial Weibel-Palade body, but not on the subsequent days. There are several explanations for the observed loss of relation between Ang-2 and VWF levels. First, the synthesis and subsequent storage of Ang-2 and VWF in de Weibel-Palade bodies may become differently regulated throughout the course of disease, so that the ratio between Ang-2 and VWF changed. Second, Ang-2 may not only be released from the Weibel-Palade body, but also by constitutive secretion from the cytoplasm. Indeed, Ang-2 is uniformly distributed in the cytoplasm of endothelial cells in the absence of VWF [13]. Third, the binding or consumption of VWF may be increased in more severely ill patients, for example, during diffuse intravascular coagulation.
Our study has several limitations. First, the relation between Ang-2 and a positive fluid balance or pulmonary dysfunction was relatively modest (r = 0.25–0.30), suggesting that the positive fluid balance and pulmonary dysfunction are only partly due to increased Ang-2 levels. Indeed, it has been reported that Ang-2 sensitizes the endothelium to inflammatory stimuli rather than acting alone in the vascular system [37]. Second, it was not feasible to measure the pulmonary vascular permeability in a more direct manner with the pulmonary leak index method as we did in our previous study [12]. Instead, we studied the relation with fluid balance as surrogate indicator of vascular permeability. The data suggest that differences and changes in fluid balance were not confounded by differences and changes in renal function as can be judged, albeit imperfectly, from serum creatinine levels. Therefore, changes in the fluid balance are likely explained, at least in part, by changes in vascular permeability, even though not reflecting pulmonary vascular permeability directly. However, it is likely that the systemic and pulmonary vascular endothelium are simultaneously activated, since both are exposed to circulating inflammatory mediators. Furthermore, the fluid balance related to the P aO2/F iO2 ratio and the oxygenation index, and we confirmed that a positive fluid balance is related to a worse outcome in ALI and septic shock [26, 27], suggesting that a positive fluid balance includes pulmonary injury-induced oedema. Third, the plasma levels of Ang-2, VWF and Ang-1 and the difference in Ang-2 levels between survivors and non-survivors may have been underestimated due to fluid resuscitation and plasma dilution. This indicates that the difference in plasma levels of the measured proteins may be even greater and the relation with the fluid balance and pulmonary dysfunction even stronger. Fourth, in multivariate analysis, APACHE II score and Ang-2, but not fluid balance, P aO2/F iO2 ratio, oxygenation index, PEEP and Ang-1 at day 0 remained significantly predictive factors of ICU mortality. Nevertheless, the value of this analysis is limited in our relatively small group of 50 patients.
In conclusion, in contrast to VWF levels, increased Ang-2 levels relate to a positive fluid balance and pulmonary dysfunction throughout the course of septic shock. While VWF levels only predict ICU mortality early in the course of septic shock, Ang-2 levels do so throughout the course. Pharmacological blockade of Ang-2 during the course of septic shock might reduce the degree of vascular permeability and pulmonary dysfunction and should be pursued in future studies for outcome benefits.
References
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150
Aird WC (2003) The role of the endothelium in severe sepsis and multiple organ dysfunction syndrome. Blood 101:3765–3777
Groeneveld ABJ (2002) Vascular pharmacology of acute lung injury and acute respiratory distress syndrome. Vascul Pharmacol 39:247–256
Orfanos SE, Kotanidou A, Glynos C, Athanasiou C, Tsigkos S, Dimopoulou I, Sotiropoulou C, Zakynthinos S, Armaganidis A, Papapetropoulos A, Roussos C (2006) Angiopoietin-2 is increased in severe sepsis: correlation with inflammatory mediators. Crit Care Med 35:199–206
Parikh SM, Mammoto T, Schultz A, Yuan HT, Christiani D, Karumanchi SA, Sukhatme VP (2006) Excess circulating angiopoietin-2 may contribute to pulmonary vascular leak in sepsis in humans. PLoS Med 3:356–370
Giuliano JS Jr, Lahni PM, Harmon K, Wong HR, Doughty LA, Carcillo JA, Zingarelli B, Sukhatme VP, Parikh SM, Wheeler DS (2007) Admission angiopoietin levels in children with septic shock. Shock 28:650–654
Gallagher DC, Parikh SM, Balonov K, Miller A, Gautam S, Talmor D, Sukhatme VP (2008) Circulating angiopoietin 2 correlates with mortality in a surgical population with acute lung injury/adult respiratory distress syndrome. Shock 29:656–661
Ganter MT, Cohen MJ, Brohi K, Chesebro BB, Staudenmayer KL, Rahn P, Christiaans SC, Bir ND, Pittet JF (2008) Angiopoietin-2, marker and mediator of endothelial activation with prognostic significance early after trauma? Ann Surg 247:320–326
Giamarellos-Bourboulis EJ, Kanellakopoulou K, Pelekanou A, Tsaganos T, Kotzampassi K (2008) Kinetics of angiopoietin-2 in serum of multi-trauma patients: correlation with patient severity. Cytokine 44:310–313
Kumpers P, Lukasz A, David S, Horn R, Hafer C, Faulhaber-Walter R, Fliser D, Haller H, Kielstein JT (2008) Excess circulating angiopoietin-2 is a strong predictor of mortality in critically ill medical patients. Crit Care 12:R147
Siner JM, Bhandari V, Engle KM, Elias JA, Siegel MD (2009) Elevated serum angiopoietin-2 levels are associated with increased mortality in sepsis. Shock 31:348–353
Van der Heijden M, Van Nieuw Amerongen GP, Koolwijk P, Van Hinsbergh VWM, Groeneveld ABJ (2008) Angiopoietin-2, permeability oedema, occurrence and severity of ALI/ARDS in septic and non-septic critically ill patients. Thorax 63:903–909
Fiedler U, Scharpfenecker M, Koidl S, Hegen A, Grunow V, Schmidt JM, Kriz W, Thurston G, Augustin HG (2004) The Tie-2 ligand angiopoietin-2 is stored in and rapidly released upon stimulation from endothelial cell Weibel-Palade bodies. Blood 103:4150–4156
Rondaij MG, Bierings R, Kragt A, Van Mourik JA, Voorberg J (2006) Dynamics and plasticity of Weibel-Palade bodies in endothelial cells. Arterioscler Thromb Vasc Biol 26:1002–1007
Ware LB, Conner ER, Matthay MA (2001) von Willebrand factor antigen is an independent marker of poor outcome in patients with early acute lung injury. Crit Care Med 29:2325–2331
Ware LB, Eisner MD, Thompson BT, Parsons PE, Matthay MA (2004) Significance of von Willebrand factor in septic and nonseptic patients with acute lung injury. Am J Respir Crit Care Med 170:766–772
Eklund L, Olsen BR (2006) Tie receptors and their angiopoietin ligands are context-dependent regulators of vascular remodeling. Exp Cell Res 312:630–641
Maisonpierre PC, Suri C, Jones PF, Bartunkova S, Wiegand SJ, Radziejewski C, Compton D, McClain J, Aldrich TH, Papadopoulos N, Daly TJ, Davis S, Sato TN, Yancopoulos GD (1997) Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science 277:55–60
Scharpfenecker M, Fiedler U, Reiss Y, Augustin HG (2005) The Tie-2 ligand angiopoietin-2 destabilizes quiescent endothelium through an internal autocrine loop mechanism. J Cell Sci 118:771–780
Mammoto T, Parikh SM, Mammoto A, Gallagher D, Chan B, Mostoslavsky G, Ingber DE, Sukhatme VP (2007) Angiopoietin-1 requires p190 RhoGAP to protect against vascular leakage in vivo. J Biol Chem 282:23910–23918
McCarter SD, Mei SH, Lai PF, Zhang QW, Parker CH, Suen RS, Hood RD, Zhao YD, Deng Y, Han RN, Dumont DJ, Stewart DJ (2007) Cell-based angiopoietin-1 gene therapy for acute lung injury. Am J Respir Crit Care Med 175:1014–1026
Witzenbichler B, Westermann D, Knueppel S, Schultheiss HP, Tschope C (2005) Protective role of angiopoietin-1 in endotoxic shock. Circulation 111:97–105
Bhandari V, Choo-Wing R, Lee CG, Zhu Z, Nedrelow JH, Chupp GL, Zhang X, Matthay MA, Ware LB, Homer RJ, Lee PJ, Geick A, de Fougerolles AR, Elias JA (2006) Hyperoxia causes angiopoietin 2-mediated acute lung injury and necrotic cell death. Nat Med 12:1286–1293
Van der Heijden M, Van Nieuw Amerongen GP, Chedamni S, Van Hinsbergh VWM, Groeneveld ABJ (2009) The angiopoietin-Tie2 system as a therapeutic target in sepsis and acute lung injury. Expert Opin Ther Targets 13:39–53
Giuliano JS Jr, Lahni PM, Bigham MT, Manning PB, Nelson DP, Wong HR, Wheeler DS (2008) Plasma angiopoietin-2 levels increase in children following cardiopulmonary bypass. Intensive Care Med 34:1851–1857
Sakr Y, Vincent JL, Reinhart K, Groeneveld J, Michalopoulos A, Sprung CL, Artigas A, Ranieri VM (2005) High tidal volume and positive fluid balance are associated with worse outcome in acute lung injury. Chest 128:3098–3108
Alsous F, Khamiees M, DeGirolamo A, Moateng-Adjepong Y, Manthous CA (2000) Negative fluid balance predicts survival in patients with septic shock: a retrospective pilot study. Chest 117:1749–1754
Pickkers P, Sprong T, Eijk L, Van der Hoeven JG, Smits P, Deuren M (2005) Vascular endothelial growth factor is increased during the first 48 h of human septic shock and correlates with vascular permeability. Shock 24:508–512
Seeley E, McAuley DF, Eisner M, Miletin M, Matthay MA, Kallet RH (2008) Predictors of mortality in acute lung injury during the era of lung protective ventilation. Thorax 63:994–998
Schoenfeld DA, Bernard GR (2002) Statistical evaluation of ventilator-free days as an efficacy measure in clinical trails of treatments for acute respiratory distress syndrome. Crit Care Med 30:1772–1777
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31:1250–1256
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, LeGall JR, Morris A, Spragg R (1994) Report of the American–European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med 20:225–232
Kayal S, Jais JP, Aguini N, Chaudiere J, Labrousse J (1998) Elevated circulating E-selectin, intercellular adhesion molecule 1, and von Willebrand factor in patients with severe infection. Am J Respir Crit Care Med 157:776–784
Moss M, Ackerson L, Gillespie MK, Moore FA, Moore EE, Parsons PE (1995) von Willebrand factor antigen levels are not predictive for the adult respiratory distress syndrome. Am J Respir Crit Care Med 151:15–20
Rubin DB, Wiener-Kronish JP, Murray JF, Green DR, Turner J, Luce JM, Montgomery AB, Marks JD, Matthay MA (1990) Elevated von Willebrand factor antigen is an early plasma predictor of acute lung injury in nonpulmonary sepsis syndrome. J Clin Invest 86:474–480
Sabharwal AK, Bajaj SP, Ameri A, Tricomi SM, Hyers TM, Dahms TE, Taylor FB Jr, Bajaj MS (1995) Tissue factor pathway inhibitor and von Willebrand factor antigen levels in adult respiratory distress syndrome and in a primate model of sepsis. Am J Respir Crit Care Med 151:758–767
Fiedler U, Reiss Y, Scharpfenecker M, Grunow V, Koidl S, Thurston G, Gale NW, Witzenrath M, Rosseau S, Suttorp N, Sobke A, Herrmann M, Preissner KT, Vajkoczy P, Augustin HG (2006) Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation. Nat Med 12:235–239
Acknowledgments
We thank Jan van Bezu BSc., VU University Medical Centre, Amsterdam, The Netherlands, for excellent technical assistance. GpvNA was supported by The Netherlands Heart Foundation (The Hague, grant 2003T032). MvdH was supported by the European Society of Intensive Care Medicine (ECCRN Levi Montalcini Biomedical Sciences Award 2007). The funding sources had no involvement in the study design, the collection, analysis and interpretation of data, the writing of the report or the decision to submit the paper for publication.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
van der Heijden, M., Pickkers, P., van Nieuw Amerongen, G.P. et al. Circulating angiopoietin-2 levels in the course of septic shock: relation with fluid balance, pulmonary dysfunction and mortality. Intensive Care Med 35, 1567–1574 (2009). https://doi.org/10.1007/s00134-009-1560-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1560-y