Abstract
Objective
Multiple studies in sepsis have demonstrated that elevated troponin is associated with poor outcome. The elevated troponin in this situation is thought to be secondary to microthrombi. We hypothesized that recombinant human activated protein C (APC) treatment would improve outcomes in severe sepsis patients who have elevated troponin.
Methods
Patients with severe sepsis by consensus criteria in a university ICU were divided into a troponin elevated group (cTnI+) and a normal troponin (cTnI−) group. Outcome was compared using Fisher's exact test. APACHE II and MODS were calculated by standard methods.
Patients
We identified 105 patients with severe sepsis and troponin measured, of which 48 (46%) were in the cTnI+ group. The two groups were similar in terms of age and other comorbid conditions.
Results
APACHE II (28 ± 8 vs. 25 ± 8) was slightly higher and MODS (11 ± 4 vs. 9 ± 3) was significantly higher in the cTnI+ group. Mortality was 52% (25/48) in cTnI+ group and 30% (17/57) in cTnI− group. Mortality was 30% in cTnI+ patients treated with APC and 72% in untreated cTnI+ patients.
Conclusions
Patients with severe sepsis who have elevated troponin have increased mortality. In patients with severe sepsis who have elevated troponin, treatment with APC improves outcome. Further study is needed to determine whether troponin can serve as a simple, readily available marker to identify which patients with severe sepsis will benefit from APC.
Similar content being viewed by others
Introduction
Cardiac troponins are regulatory proteins of the thin actin filaments of the cardiac muscle [1]. Myocardial cell injury results in the release of cardiac troponin I (cTnI) and cardiac troponin T which differ from troponin isoforms from skeletal muscle and are thus highly sensitive and specific biomarkers of myocardial injury [1, 2]. The exact mechanism leading to an elevated troponin in patients with sepsis remains uncertain. Several studies have shown that flow-limiting coronary artery disease is excluded in the majority of patients with elevated troponin [3–5].
It has been speculated that myocardial injury from microvascular thrombosis plays a role in troponin release in septic patients [6]. Other proposed mechanisms which may contribute to the myocardial release of cTnI include alterations in membrane permeability at the level of myocyte cell membrane, prolonged hypotension, shock state, cardiomyocyte apoptosis, and the use of inotropic agents [3, 7–10]. The elevation in cardiac troponin levels in patients with sepsis, severe sepsis, or septic shock has been shown to indicate left ventricular dysfunction and convey a poor prognosis [3, 5, 11–13].
Activated protein C (APC) is a serine protease that inhibits coagulation factors Va and VIIIa, subsequently blocking the generation of thrombin. Both plasminogen activator inhibitor (PAI-1) and activated thrombin-activatable fibrinolysis inhibitor (TAFI) are inhibitors of the fibrinolytic system [14]. APC also exhibits profibrinolytic activity by neutralizing PAI-1 and/or by decreasing activation of TAFI by limiting thrombin generation [15, 16]. In addition to its role in coagulation, there is evidence APC exhibits direct anti-inflammatory properties independent of its antithrombotic effects as demonstrated by decreased levels of interleukin 6 in patients with severe sepsis [17]. We hypothesized that patients with severe sepsis and an elevated cTnI who were treated with APC would have significant benefit in terms of mortality [18].
Methods and materials
This was a retrospective study of patients with severe sepsis in whom troponin was measured. Patients were identified by review of a larger database of patients with severe sepsis admitted to the intensive care units (ICU) of the Oklahoma University Medical Center or the Oklahoma City Veteran Affairs Medical Center. This database was developed to study the clinical course of severe sepsis and its response to therapy. Therefore we excluded patients who were moribund, those who were “do not resuscitate”, or whose status was postcardiopulmonary resuscitation and patients with significant premorbid conditions such as metastatic cancer or Childs-Pugh class III liver disease which might influence their response or the decision to continue aggressive therapy. All patients were prospectively identified within 24 h of organ failure and informed consent for the inclusion of clinical information without identifying personal links in the database was obtained from the patient or their legal representative. The study was approved by the institutional review board. Patients were included in this study if troponin was measured within the first 3 days of ICU admission.
Patients were considered to have preexisting coronary artery disease, hypertension, and diabetes mellitus based on history at presentation. Patients were considered to have chronic renal insufficiency if they had a baseline creatinine greater than 2 mg/dl prior to presentation. Severe sepsis was defined by the presence of organ dysfunction in a patient with two or more systemic inflammatory response syndrome criteria and a documented or presumed infection which is consistent with consensus conference criteria [19]. Organ failures were cardiovascular, defined as systolic blood pressure lower than 90 mmHg for at least 1 h after adequate fluid resuscitation and/or the need for vasopressors to maintain a systolic blood pressure above 90 mmHg; respiratory failure, as defined by a PaO2/FIO2 ratio less than 300 and the presence of diffuse pulmonary infiltrates on chest radiography; renal failure was urine output less than 0.5 ml/kg per hour for 2 h or more; disseminated intravascular coagulation was diagnosed by the criteria of the International Society on Thrombosis and Hemostasis for overt DIC [20], metabolic by the presence of a lactate level higher than 3 mmol/l.
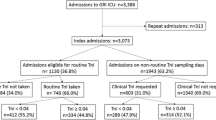
The study included 105 patients who had severe sepsis and troponin measured. Patients were divided into two groups depending on the presence or absence of an elevated troponin; those who had an elevated troponin during the first 72 h of admission to the ICU were considered as troponin positive (cTnI+, n = 48) and those who did not as troponin negative (cTnI−, n = 57). The cTnI+ group was subdivided into according to whether they received therapy with APC (APC+, n = 23, APC−, n = 25). The groups were similar in terms of age and comorbid illness (Tables 1, 2). Administration of APC (drotrecogin alfa activated) was at the discretion of the primary team except in the case of 15 patients who were part of the Recombinant Human Activated Protein C Worldwide Evaluation in Severe Sepsis (PROWESS) trial. Severity of disease was quantified by the Acute Physiology and Chronic Health Evaluation II (APACHE II) score and Multiple Organ Dysfunction Score (MODS) which was determined on the day of admission to ICU using the most abnormal values observed during that 24-h period [21, 22]. All electrocardiograms and echocardiograms were reviewed by an investigator blinded to the patient's clinical status. The primary outcome measure was mortality in ICU; lengths of stay in the ICU and hospital as well as 28-day survival were secondary outcome measures.
Laboratory
For the measurement of cTnI venous blood was collected in a lithium-heparin container. The samples are allowed to clot before centrifugation. cTnI was measured with the ADVIA centaur cTnI assay (Bayer) which is a two site sandwich immunoassay using direct chemiluminometric technology. In accord with consensus conference recommendations, values higher than 0.4 ng/ml were considered indicative of cardiac injury [23].
Statistical analysis
For normally distributed data Student's t test was applied while the Mann–Whitney test was utilized to analyze nonparametric data. Noncontinuous variables were analyzed by use of 2 × 2 tables and Fisher's exact test. Data are presented as mean ± SD or median and interquartile range (IQR) for nonnormally distributed data. Values of p < 0.05 (two-tailed) were considered statistically significant. Variables found to be significant in univariate analysis were entered into a multivariate logistic regression model to evaluate the effect of an elevated troponin on mortality. A similar statistical model was used in troponin positive subjects to evaluate the relationship between APC use and risk of death in this group of patients. Cumulative survival rates in sepsis patients with elevated troponin depending on whether they received APC are presented by Kaplan–Meier diagram, and differences among groups were tested by the log-rank test. The calculations were performed with JMP4 Software (SAS, Cary, N.C., USA) and the Kaplan–Meier survival curves were constructed utilizing the NCSS software (NCSS.com).
Results
The 105 patients who had troponin measured were more severely ill as reflected by a higher APACHE II (27 ± 8 vs. 25 ± 8, p = 0.07), MODS (10 ± 4 vs. 8 ± 3, p < 0.01), and pressor use (71% vs. 50%, p < 0.01) than the 111 who did not have troponin measured, but the frequency of coronary artery disease (12% vs. 7%) did not differ significantly. Patients in the cTnI+ group had slightly higher APACHE II scores, and there was a significant difference in their MODS. In the cTnI+ group the median troponin level was 2.6 ng/ml (range 0.45–127). The APC+ and APC− groups were similar in terms of APACHE II and MODS (Table 2).
Electrocardiograms were routinely performed on ICU admission. Electrocardiogram changes suggestive of ischemia including newly inverted or peaked T-waves, flat or down-sloping S-T segment depression, or S-T segment elevation were noted in 9 cTnI+ and 5 cTnI− patients ( p = 0.2). Four cTnI+ patients were treated with APC while five were not. Echocardiograms were obtained to evaluate cardiac function generally within 48 h of admission to ICU. Echocardiography was performed in 24 cTnI+ and 27 cTnI− patients. Global hypokinesis was noted in 3 cTnI− and 6 cTnI+ patients ( p = 0.2); two of the latter were treated with APC. Three cTnI+ and 4 cTnI− patients ( p = 1.0) had wall motion abnormalities suggestive of ischemia. One of the cTnI+ patients with a wall motion abnormality was treated with APC.
Outcome
The primary endpoint in this study was mortality in the ICU. ICU mortality in cTnI+ group was 25 of 48 (52%) compared to 17 of 57 (30%) in the cTnI− group ( p = 0.03). The 28-day mortality was also higher in cTnI+ patients (58% vs. 38%, p = 0.02). However, the ICU and hospital lengths of stay in these patients were similar. The median lengths of stay in the ICU were 9 days (IQR 4–18) and 8 days (IQR 4–16) in the cTnI+ and cTnI− groups, respectively ( p = 0.9). The median lengths of stay in the hospital were 15 days (IQR 6–25) and 16 days (IQR 8–24) in the cTnI+ and cTnI− groups, respectively ( p = 0.4).
Overall ICU mortality in the overall series of 105 patients was 40%: 36% in the APC+ group and 44% in the APC− group. This benefit of APC on mortality was due to its effect in the group with an elevated troponin (Fig. 1). Restricting our observations to those patients with an elevated troponin, ICU mortality in the APC+ group was 7 of 23 (30%) compared to 18 of 25 (72%) in the APC− group ( p = 0.008). This survival benefit persisted at 28 days (35% vs. 72% mortality, p < 0.05; Fig. 2). In contrast, in patients with normal troponin ICU mortality was slightly but not significantly higher, 10 of 27 (37%) vs. 7 of 30 (23%), in those who received APC treatment ( p = 0.1). The 28-day mortality figures in patients with normal troponin were 37% and 30% in APC+ and APC− patients, respectively. When we restricted our analysis to patients with APACHE II scores of 25 or higher, septic shock, and culture-positive sepsis (Table 3), we found that the pattern of a higher mortality in cTnI+ patients that was reduced by APC therapy persisted.
Univariate analysis of survivors and nonsurvivors in the entire group demonstrated that age, APACHE II score, MODS and troponin status were significantly associated with mortality. These significant variables and the dichotomous dependent variable (alive vs. dead) were examined in a multivariate logistic regression model. An elevated troponin level remained a significant independent predictor of mortality when adjusted for age and disease severity (odds ratio 2.64, 95% confidence interval 1.06–6.73, p = 0.03). Within the cTnI+ group those who died had higher APACHE and MODS scores and were less likely to be treated with APC than were survivors. When these variables were introduced into a multivariate logistic regression analysis in which the dependent variable was mortality (alive vs. dead), a significant increase in risk of death was seen in patients who did not receive APC (odds ratio 3.84, 95% confidence interval 1.08–8.3, p = 0.04).
APC treatment had no apparent effect on ICU and hospital length of stay. Both were similar in patients with normal or elevated troponin. The median lengths of stay in the ICU were 8 days (IQR 4–14) and 10 days (IQR 2–21) in the APC+ and the APC− groups, respectively ( p = 0.8), while the median lengths of stay in the hospital were 17 days (IQR 8–25) and 10 days (IQR 4–21) in the APC+ and the APC− groups, respectively ( p = 0.09).
Discussion
In the present study of 105 patients with severe sepsis who had cardiac troponin measured there was significant higher mortality in the group of patients who had elevated troponin. Also of note is that patients with elevated troponin in our study had APACHE II scores which were slightly higher and the MODS were significantly elevated compared to the group with normal troponin. This is consistent with previous studies which indicated that an elevated troponin reflects a higher severity of disease [3, 13], the presence of myocardial dysfunction [5, 11, 13, 24], and a worse prognosis [5, 12, 13, 25].
It is unlikely that the elevated troponins observed in the present study were due solely to coronary artery disease. Even though 17% of patients had a history of coronary artery disease, the electrocardiographic changes observed were nonspecific, and only three patients in the elevated troponin group had wall motion abnormalities identified by echocardiography. A similar frequency of electrocardiographic and echocardiographic abnormalities was observed in our patients with normal troponin levels. This is consistent with the study by Ver Elst et al. [3] who observed elevated troponin in one-half of their 46 patients with septic shock but found that the myocardial changes at autopsy were nonspecific in six of seven nonsurvivors with an elevated troponin and similar to those noted in four of five troponin-negative patients who died. Ammann and colleagues [4] also noted elevated troponins in a group of patients with severe sepsis but excluded coronary disease in the majority by stress echocardiography, coronary angiography, or autopsy. It has been speculated that the elevated troponin is due to microthrombi secondary to sepsis [6]. In a subsequent study Ammann et al. [5] observed higher levels of tumor necrosis factor α and interleukin 6 in patients with elevated troponin and suggested that these mediators also play a role in troponin release. Individually, tumor necrosis factor α and interleukin 1β each caused significant concentration-dependent depression of maximum extent and peak velocity of myocyte shortening in vitro. In combination, tumor necrosis factor α and interleukin 1β induced depression of myocardial cell contractility at substantially lower concentrations consistent with a synergistic effect [26]. Interleukin 6 also causes significant myocardial depression in vitro. Removal of interleukin 6 from serum samples of patients with meningococcemia and from supernatants of inflammatory cells stimulated by meningococci in vitro abolished the negative inotropic activity. Furthermore, the serum concentrations of interleukin 6 strongly predicted degree of myocardial dysfunction and severity of disease in children with meningococcal septic shock [27].
APC treatment of patients with elevated troponin was associated with significant reduction in mortality from 72% to 30% in our study. Yan and colleagues [14] demonstrated that 63 of 70 (90%) of patients who met the standard clinical criteria for severe sepsis had significantly reduced protein C levels. During severe sepsis a combination of protein C consumption, protein S inactivation, and reduction in activity of the activation complex by oxidation, cytokine-mediated downregulation, and proteolytic release of the activation components sets in motion conditions that would favor an acquired defect in the protein C pathway which in turn favors microvascular thrombosis, increased leukocyte adhesion, and increased cytokine formation [28]. A phase 3 randomized controlled trial (PROWESS) involving 1,690 patients showed an absolute reduction in the relative risk of death from all causes at 28 days of 6.1% [17]. A subgroup analysis performed with APACHE II quartiles showed that most of the reduction in mortality occurred among patients receiving APC with APACHE II scores in the third and fourth quartiles, representing those with the most severe disease [29]. In the ADDRESS trial which was a randomized, placebo-controlled, blinded trial of APC involving adult patients with severe sepsis who were at low risk of death (as defined by APACHE II scores < 25 or single-organ failure) 28-day mortality and in-hospital mortality were statistically the same in the group receiving APC and the control group, and the rate of serious bleeding was similar to that in the PROWESS trial [30]. Thus APC benefits the more severely affected sepsis patient.
APC has both anticoagulant properties and anti-inflammatory properties, and it therefore seems reasonable to speculate that if the elevated troponin is secondary to the combination of microthrombi formation and myocardial depression from inflammatory mediators such as tumor necrosis factor and interleukin 6 that the use of APC should mitigate these effects and lead to an improved outcome. This was observed in our patients with an elevated troponin. In contrast our patients with normal troponins did not benefit from APC. Based on their MODS as well as their response to APC it would be reasonable to argue that those patients were less sick than those in the cTnI+ group. This suggests that an elevated troponin is an early marker of dysfunction in coagulation due to sepsis, and that these are probably the patients who have acquired protein C deficiency.
A limitation of our study is it was a retrospective analysis of the subgroup of database patients who had troponin measurements, and the benefit associated with APC treatment was limited to the subgroup with elevated cTnI. Troponin was not systematically measured in all patients in our database, and slightly less than one-half the patients in our database had a troponin determination. The patients with cTnI measurements tended to be sicker and were more likely to be pressor dependent than those without cTnI measurements. While 3 of the 27 cTnI− patients did not have troponin measurements until after the start of APC therapy, 14 of 23 cTnI+ patients had their first troponin measurement after the start of APC. Thus while troponin should be measured early if it is to be used to identify high-risk patients who might benefit from APC use, it does not appear that APC treatment will produce false-negative values.
Although an inherent bias cannot be excluded in selecting patients for troponin measurements or APC therapy, the purpose of developing our database was to examine the course of severe sepsis and its response to treatment. Therefore patients with significant underlying conditions such as metastatic malignancy or Child-Pugh class III liver disease that might influence the decision to continue aggressive care were excluded. The cTnI+ patients who did not receive therapy tended to be older and were slightly sicker as reflected by APACHE II, but none of these differences were statistically significant. Nonetheless we cannot exclude the possibility that these differences contributed to the worse outcome in these patients.
Ideally the results of the present study should be confirmed in a prospective randomized placebo controlled trial. However, such a trial would raise ethical issues in light of the proven benefit of APC therapy in patients with severe sepsis and APACHE II scores higher than 25. Prospective examination of troponin levels in APC treated patients may confirm the utility of this measurement.
In summary, our study confirms previous work that indicates an elevated troponin is a prognostic marker in patients with sepsis indicating an increased mortality. In patients with severe sepsis and elevated troponin treatment with APC is associated with an improved outcome. Further studies are needed to determine whether an elevated troponin serves as a simple and readily available marker identifying those patients with severe sepsis who will benefit from treatment with APC.
References
Ammann P, Pfisterer M, Fehr T (2004) Raised cardiac troponins. BMJ 328:1028–1029
Gunnewiek JM, Van der Hoeven JG (2004) Cardiac troponin elevations among critically ill patients. Curr Opin Crit Care 10:342–346
Ver Elst KM, Spapen HD, Nguyen DN, Garbar C, Huyghens LP, Gorus FK (2000) Cardiac troponin I and T are biological markers of left ventricular dysfunction in septic shock. Clin Chem 46:650–657
Ammann P, Fehr T, Minder EI, Gunter C, Bertel O (2001) Elevation of troponin I in sepsis and septic shock. Intensive Care Med 27:965–969
Ammann P, Maggiorini M, Bertel O et al. (2003) Troponin as a risk factor for mortality in critically ill patients without acute coronary syndromes. J Am Coll Cardiol 41:2004–2009
Maeder M, Fehr T, Rickli H, Ammann P (2006) Sepsis-associated myocardial dysfunction: diagnostic and prognostic impact of cardiac troponins and natriuretic peptides. Chest 129:1349–1366
Piper HM, Schwartz P, Spahr R (1984) Early enzyme release from myocardial cells is not due to irreversible cell damage. J Mol Cell Cardiol 16:385–388
Wu AHB (2001) Increased troponin in patients with sepsis and septic shock: myocardial necrosis or reversible myocardial depression. Intensive Care Med 27:959–961
van Bockel E, Tulleken JE, Muller Kobold AC et al. (2003) Cardiac troponin I release and cytokine response during experimental human endotoxaemia. Intensive Care Med 29:1598–1600
Beranek JT (2002) Cardiomyocyte apoptosis contributes to the pathology of the septic shock heart. Intensive Care Med 28:218
Fernandes C Jr, Akamine N, Knobel E (1999) Cardiac troponin: a new serum marker of myocardial injury in sepsis. Intensive Care Med 25:1165–1168
Spies C, Haude V, Fitzner R et al. (1998) Serum cardiac troponin T as a prognostic marker in early sepsis. Chest 113:1055–1063
Metha NJ, Khan IA, Gupta V (2004) Cardiac troponin predicts myocardial dysfunction and adverse outcome in septic shock. Int J Cardiol 95:13–17
Yan SB, Helterbrand JD, Hartman DL, Wright TJ, Bernard GR (2001) Low levels of protein C are associated with poor outcome in severe sepsis. Chest 120:915–922
Bajzar L, Nesheim ME, Tracy PB (1996) The profibrinolytic effect of activated protein C in clots formed from plasma is TAFI-dependent. Blood 88:2093–2100
Vervloet MG, Thijs LG, Hack CE (1998) Derangements of coagulation and fibrinolysis in critically ill patients with sepsis and septic shock. Semin Thromb Hemost 24:33–44
Bernard GR, Vincent J-L, Laterre P-F (2001) Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med 273:1945–1949
John J, Awab A, Kinasewitz G, Norman D (2006) Activated protein C improves survival in severe sepsis patients with elevated troponin. Crit Care Med 34:A112
Levy MM, Fink MP, Marshall JC et al. (2003) 2001 SCCM/ESICMA/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31:1250–1256
Taylor FB Jr, Toh C-H, Hoots WK, Wada H, Levi M (2001) Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. J Thromb Haemost 86:1327–1330
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Marshall J, Cook DJ, Christou NV, Bernard GR, Sprung CL, Sibbald WJ (1995) Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 23:1638–1652
Alpert JS, Thygesen K, Antman E, Bassand JP (2000) Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 36:959–969
Wilder RL, Lafyatis R, Roberts AB et al. (1990) Transforming growth factor-b in rheumatoid arthritis. Ann NY Acad Sci 593:197–207
Arlati S, Brenna S, Prencipe L et al. (2000) Myocardial necrosis in ICU patients with acute non-cardiac disease: a prospective study. Intensive Care Med 26:31–37
Kumar A, Thota V, Dee L (1996) Tumor necrosis factor-a and interleukin-a-b are responsible for depression of in vitro myocardial cell contractility induced by serum from humans with septic shock. J Exp Med 183:949–958
Pathan N, Hemingway CA, Alizadeh AA (2004) Role of interleukin 6 in myocardial dysfunction of meningococcal septic shock. Lancet 363:203–209
Esmon CT (2003) The protein C pathway. Chest 124:26–32
Ely EW, Laterre P-F, Angus DC et al. (2003) Drotrecogin alfa (activated) administration across clinically important subgroups of patients with severe sepsis. Crit Care Med 31:12–19
Abraham E, Laterre P-F, Garg R (2005) Drotrecogin alfa (activated) for adults with severe sepsis and a low risk of death. N Engl J Med 353:1332–1341
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
John, J., Awab, A., Norman, D. et al. Activated protein C improves survival in severe sepsis patients with elevated troponin. Intensive Care Med 33, 2122–2128 (2007). https://doi.org/10.1007/s00134-007-0816-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0816-7