Abstract
Objective
There is reluctance to use glutamine-containing i. v. nutrition for neurosurgical patients, as this may result in elevated intracerebral glutamate levels, which are thought to be associated with neuronal injury and cell swelling, causing an increase in ICP and an unfavourable outcome. As general ICU patients benefit from i. v. glutamine supplementation in terms of reduced mortality and morbidity, neurosurgical patients might also be candidates for such treatment, if the possible relation between i. v. glutamine supplementation and a possible increase in cerebral glutamate could be sorted out.
Design and setting
The study protocol had a crossover design with a 24 h treatment period and a 24 h placebo period in random order. Treatment was a glutamine containing dipeptide, L-alanyl-L-glutamine 200 mg/ml, for 20 h; placebo was saline. The rate of infusion was 0.125 ml/kg/h, which is equal to 0.34 g/kg of glutamine over the 20 h period. Microdialysate was collected for analysis in 120 min portions. The flow through the microdialysis catheter was 0.3 μ l/min.
Subjects
Patients with severe head trauma (GCS ≤ 8; n = 15) on routine monitoring, including intracerebral microdialysis, were randomly assigned to treatment followed by placebo or placebo followed by treatment.
Measurements and results
Glutamine infusion increased plasma glutamine concentration by 30%, but not plasma glutamate concentration. Intracerebral glutamate was unaffected in median values and in all individual patients.
Conclusion
Intravenous glutamine in clinically relevant doses leaves cerebral glutamate unaffected. This opens the possibility of evaluating the effects of i. v. glutamine supplementation upon outcome for neurosurgical ICU patients.
Similar content being viewed by others
Introduction
Intravenous glutamine supplementation as part of nutrition to intensive care unit (ICU) patients improves outcome [1]. This is demonstrated in general ICU patients with intravenous feeding and in burn patients with enteral feeding combined with intravenous glutamine supplementation [2, 3, 4]. The background to these effects is primarily attributed to prevention of glutamine depletion, which occurs in several tissues of ICU patients [5, 6, 7]. Low plasma glutamine concentration at ICU admission is an independent prognostic factor for unfavourable outcome in ICU patients [8]. Although neurosurgical patients are a separate patient group, with similarities to and differences from general ICU patients, i. v. glutamine supplementation may also be beneficial for long-stay neurosurgical patients who require nutrition. So far there are no reports of adverse effects of glutamine supplementation given to general ICU patients [9]. For neurosurgical patients, however, there is a reluctance to administer glutamine supplementation because exogenous glutamine may cause an increase of plasma glutamate concentration, which in turn may lead to adverse effects through glutamate accumulation in the brain. Alternatively, elevated plasma glutamine concentrations may prevent glutamine clearance in the brain.
Glutamate is an excitatory neurotransmitter. There are glutamate receptors in the synapses between neurons. Glutamate is produced in the neurons and released into the synapses. Elimination is by re-uptake into neurons but most importantly through uptake into astrocytes, where glutamate is aminated into glutamine. Case reports have been published in which high concentrations of glutamate in the interstitial fluid adjacent to brain injury were found in neurosurgical patients [10, 11, 12, 13]. It has been suggested that a high concentration of glutamate may be associated with cerebral swelling and a high intracranial pressure (ICP). However, the mechanism behind the possible relation between high interstitial glutamate concentration and high ICP is still obscure [13, 14]. Nevertheless, there is a fear that exogenous glutamine supplementation may increase interstitial glutamate concentration intracerebrally in brain injury patients, resulting in detrimental effects upon outcome. It is beyond the scope of this study to clarify the background and the physiological implications of elevated glutamate concentration in interstitial fluid of the brain in neurosurgical patients. Rather, it confines itself to addressing the relation between exogenous i. v. glutamine administration and glutamate concentration in the brain.
The aim of the study was to determine whether a clinically relevant i. v. infusion of glutamine as part of a nutritional protocol would have any impact upon the interstitial glutamate concentration in the brain as sampled through intracerebral microdialysis. This was studied in head trauma patients with severe injury requiring ventilator treatment, ICP monitoring, and microdialysis monitoring. The study design was randomized crossover with intravenous glutamine versus placebo, and the primary outcome parameter was glutamate concentration in the microdialysate from an intracerebral catheter placed adjacent to the injured area.
Materials and methods
Patients in the neurosurgical ICU were eligible for the study. Inclusion criteria were severe head injury with Glasgow Coma Score (GCS) ≤ 8 with invasive ICP monitoring and microdialysis monitoring. Absence of informed consent was an exclusion criterion. The characteristics of the patients are given in Table 1. Informed consent was obtained from the legal representative of the patient (in all cases the next of kin), and the study protocol was approved by the Ethics Committee of Karolinska Institutet.
When positioning the microdialysis catheter in the brain we aimed for the penumbra zone surrounding a brain contusion, which has been shown to be highly vulnerable compared with normal brain tissue [11]. After placement of the microdialysis catheter (CMA70, 10 mm membrane, CMA Microdialysis, Stockholm) an intracerebral placement close to the injured area was documented by computer tomography (CT). A run-in period of at least 12 h before the start of the study commenced immediately after placement of the microdialysis catheter. The 48-h study period fell within the initial 4 days of ICU stay.
All patients were intubated and sedated on a pressure-controlled ventilator mode. This decision was taken when GCS was ≤ 8, according to the routines of the unit. The goal of the brain-protective therapy was to keep ICP below 20 mmHg. Patients were initially sedated using propofol. When prolonged sedation (> 4 days) was needed a switch to midazolam/morphine sedation was accomplished. During the study period, however, propofol or barbiturates were used for sedation. Patients received intravenous nutrition 24 h/day using separate components of amino acids (Vamin. Glucose, Fresenius-Kabi), fat (Vasolipid 20%, Braun) and glucose. The caloric target was 25 kcal/kg body weight (BW), and the fat emulsion provided not more than 40% of the total energy supply. The amino acid solution was administered according to BW (10 ml/kg/24 h), and it contained glutamate (9.0 g/l), but no glutamine.
The study protocol had a randomized crossover design with a 24-h treatment period and a 24-h placebo period in random order. Microdialysate was collected for analysis in 120-min portions. The flow through the microdialysis catheter was 0.3 μl/min. Glutamine was given as a glutamine-containing dipeptide, L-alanyl-L-glutamine 200 mg/ml (Dipeptiven, Fresenius-Kabi), at a rate of 0.125 ml/kg/h, which is equal to 0.34 g/kg of glutamine over a period of 20 h. Patients heavier than 90 kg received the dose for a patient of 90 kg. During the placebo period saline was given at the same infusion rate. Plasma samples were taken at the start and at the end of glutamine/placebo infusion. Amino acid concentrations in microdialysate and in plasma were analysed by high-performance liquid chromatography (HPLC) techniques [15].
Values are presented as medians and ranges, unless otherwise specified. Plasma and intracerebral concentrations were compared using the Mann–Whitney test for paired samples.
Results
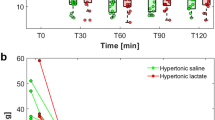
Plasma determinations of glutamine and glutamate demonstrated higher concentrations of glutamine during the infusion of glutamine-containing dipeptide (Fig. 1), than during the placebo infusion, which left the plasma glutamine concentration unaffected. The median (range) values for glutamine were 582 (298–1014) μ mol/l versus 383 (250–636) μmol/l, p < 0.05, at the end of the glutamine and placebo infusions respectively. For glutamate the plasma concentration during the glutamine and placebo infusions did not change significantly [272 (170–275) μmol/l versus 236 (163–309) μmol/l, NS] (Fig. 2). In addition, no individual patient showed more than a marginal increase in plasma concentration of glutamate during the glutamine infusion.
Plasma glutamine concentrations in head trauma patients given a L-alanyl-L-glutamine or b placebo over a period of 20 h. Filled symbols represent patients randomized to be given glutamine before placebo, while open symbols represent patients given placebo before glutamine. The bold line represents median values
Plasma glutamate concentrations in head trauma patients given a L-alanyl-L-glutamine or b placebo over a period of 20 h. Filled symbols represent patients randomized to be given glutamine before placebo, while open symbols represent patients given placebo before glutamine. The bold line represents median values
The concentrations of glutamate in microdialysate during the glutamine and placebo infusions are given in Fig. 3. The interindividual scatter in interstitial glutamate concentrations was considerable, but there was no change in the median value or in any individual patient during the treatment period or the control period. The glutamine concentrations in the microdialysate are given in Fig. 4. Also for glutamine, there were no changes in the median value or in any individual patient during the treatment period or the control period, although the plasma glutamine concentration increased during the treatment period.
Interstitial cerebral glutamate concentrations obtained via a microdialysis catheter placed adjacent to the injured area in head trauma patients given a L-alanyl-L-glutamine or b placebo over a period of 20 h. Filled symbols represent patients randomized to be given glutamine before placebo, while open symbols represent patients given placebo before glutamine. The bold line represents median values
Interstitial cerebral glutamine concentrations obtained via a microdialysis catheter placed adjacent to the injured area in head trauma patients given a L-alanyl-L-glutamine or b placebo over a period of 20 h. Filled symbols represent patients randomized to be given glutamine before placebo, while open symbols represent patients given placebo before glutamine. The bold line represents median values
Discussion
In patients with severe head trauma, i. v. administration of exogenous glutamine 20–25 g over a period of 20 h did not influence the glutamate concentration interstitially in the brain close to the injured area as assessed by microdialysis.
This finding was obtained in a well-defined group of neurosurgical patients with documented placement of their microdialysis catheters under well-characterized clinical conditions during the study period. Furthermore, measurements began only after a 12-h run-in period following placement of the catheter. The dose of glutamine administrated was in accord with the clinical recommendations given for general ICU patients [16], resulting in an increase in plasma glutamine concentrations from low to normal level in the majority of the patients (Fig. 1). This is in agreement with earlier studies [17], also with no influence upon plasma glutamate concentration (Fig. 2).
The normal interstitial concentration of glutamate in the brain is less than 10 μmol/l [12]. Among the patients studied, there was one clear outlier in interstitial glutamine concentration, and in addition four patients had clearly elevated concentrations of glutamate. However, these elevated levels of glutamate were totally independent of intravenous administration of glutamine, and they did not change over time. High interstitial glutamate concentrations in individual patients have been reported in most studies involving interstitial glutamate concentration measurements in brain injury patients [10, 11, 12, 13]. The mechanisms behind elevated glutamate concentrations interstitially in the brain as well as the pathophysiological interpretation of such elevated concentrations are beyond the scope of this study.
The recommendation to give exogenous i. v. glutamine supplementation to ICU patients rests on evidence that such administration is beneficial in terms of outcome [1], and that it does not cause any harm to the patients [9]. This is true for general ICU patients, and this study seems to show that intravenous glutamine administration to patients with severe head injury does not cause any adverse effects in terms of further elevation of the interstitial glutamate concentration in the brain. It must be emphasized that this finding was in patients with severe head trauma, and that the documentation of interstitial glutamate concentration is related to the placement of a catheter in the brain. Furthermore, the beneficial effect of glutamine is documented in studies of general ICU patients with multiple organ failure, a situation differing from that of the patients studied here. As the catabolic drive in brain injury patients is often even more pronounced than in general ICU patients with multiple organ failure, similar beneficial effects of i. v. glutamine can be postulated in neurosurgery patients, but no such study exists at present. The rationale for glutamine supplementation in ICU patients is the glutamine depletion in plasma and tissues [8, 9]. This has been demonstrated in general ICU patients, and the present study shows that similar plasma concentrations are also seen in patients with severe head trauma in the neuro-ICU (Fig. 1), which opens the possibility of evaluating the use of glutamine supplementation also in neuro-ICU patients requiring nutritional support.
The interstitial concentration of glutamine in the microdialysate was also unaffected by the i. v. infusion of glutamine, while there was an increase in plasma concentration by a median 30%. This demonstrates that the interstitial concentrations of the injured brain were not influenced by plasma concentrations, although the blood–brain barrier is known to be leaking in the area close to the injury [18]. As an elevated interstitial concentration of glutamine in the brain may influence the clearance of glutamate, the observed unaltered concentration of glutamine in the brain may also be interpreted as indicating that i. v. glutamine administration does not interfere with glutamate elimination. Plasma glutamine concentration is not known to correlate with the efflux of glutamine from the brain or any other glutamine-exporting tissue [19, 20].
In summary, exogenous i. v. glutamine administration to severe head trauma patients in the neuro-ICU was not associated with an elevation of interstitial glutamate concentration in the brain tissue adjacent to the injured area. This was true both for patients with normal intracerebral glutamate concentration and for patients with an elevated glutamate concentration. The results suggest it to be safe, in terms of intracerebral glutamate concentration, to use i. v. glutamine as a nutritional adjunct to head trauma patients. It also opens the possibility of studying the efficacy of i. v. glutamine supplementation in this group of patients.
References
Novak F, Heyland DK, Avenell A, Drover JW, Su X (2002) Glutamine supplementation in serious illness: a systematic review of the evidence. Crit Care Med 30:2022–2029
Griffiths RD, Jones C, Palmer TEA (1997) Six-month outcome of critically ill patients given glutamine supplemented parenteral nutrition. Nutrition 13:295–302
Goeters C, Wenn A, Mertes N, Wempe C, Van Aken H, Stehle P, Bone HG (2002) Parenteral L-alanyl-L-glutamine improves six month outcome in critically ill patients. Crit Care Med 30:2032–2037
Wischmeyer PE, Lynch J, Liedel J, Wolfson R, Riehm J, Gottlieb L, Kahana M (2001) Glutamine administration reduces Gram-negative bacteremia in severely burned patients: a prospective, randomized, double-blind trial versus isonitrogenous control. Crit Care Med 29:2075–2080
Roth E, Funovic J, Mühlbacker F, Schemper M, Mauritz W, Sporn P, Fritsch A (1982) Metabolic disorders in severe abdominal sepsis: glutamine deficiency in skeletal muscle. Clin Nutr 1:25–42
Gamrin L, Essén P, Andersson K, Hultman E, Nilsson E, Wernerman J (1997) Longitudinal changes of biochemical parameterin muscle during critical illness. Metabolism 46:756–762
Ahlman B, Ljungqvist O, Persson B, Bindslev L, Wernerman J (1995) Intestinal amino acid content in critically ill patients. J Parenteral Enteral Nutr 19:272–278
Oudemans-van Straaten HM, Bosman RJ, Treskes M, van der Spoel HJ, Zandsra DF (2001) Plasma glutamine depletion and patient outcome in acute ICU admissions. Intensive Care Med 27:84–90
Wernerman J (2004) Suggestions for present and future use of parenteral glutamine. Clin Nutr Suppl 1:37–42
Hlatky R, Valadka AB, Goodman JC, Contant CF, Robertson CS (2004) Patterns of energy substrates during ischemia measured in the brain by microdialysis. J Neurotrauma 21:894–906
Stahl N, Schalen W, Ungerstedt U, Nordstrom CH (2003) Bedside biochemical monitoring of the penumbra zone surrounding an evacuated acute subdural haematoma. Acta Neurol Scand 108:211–215
Reinstrup P, Stahl N, Mellergard P, Uski T, Ungerstedt U, Nordstrom CH (2000) Intracerebral microdialysis in clinical practice: baseline values for chemical markers during wakefulness, anesthesia, and neurosurgery. Neurosurgery 47:701–709
Marion DW, Puccio A, Wisniewski SR, Kochanek P, Dixon CE, Bullian L, Carlier P (2002) Effect of hyperventilation on extracellular concentrations of glutamate, lactate, pyruvate, and local cerebral blood flow in patients with severe traumatic brain injury. Crit Care Med 30:2619–2625
Mendelowitsch A, Sekhar LN, Wright DC, Nadel A, Miyashita H, Richardson R, Kent M, Shuaib A (1998) An increase in extracellular glutamate is a sensitive method of detecting ischaemic neuronal damage during cranial base and cerebrovascular surgery. An in vivo microdialysis study. Acta Neurochir 140:349–355
Kedenburg CP (1971) A lithium buffer system for accelerated single-column amino acid analysis in physiological fluids. Anal Biochem 40:35–42
Griffiths RD (2001) The evidence for glutamine use in the critically ill. Proc Nutr Soc 60:1–8
Tjäder I, Rooyackers O, Forsberg A-M, Vesali VR, Garlick PJ, Wernerman J (2004) Effects of skeletal muscle of intravenous glutamine supplementation in ICU patients. Intensive Care Med 30:266–275
Todd NV, Graham DI (1990) Blood–brain barrier damage in traumatic brain contusions. Acta Neurochir Suppl 51:296–299
Svedjeholm R, Svensson S, Ekroth R, Milocco I, Nilsson F, Vinnars E, Wernerman J (1990) Trauma metabolism and the heart; studies of heart and leg amino acid flux after cardiac surgery. Thorac Cardiovasc Surg 38:1–5
Vesali RF, Klaude M, Rooyackers O, Tjäder I, Barle H, Wernerman J (2002) Longitudinal pattern of glutamine/glutamate balance across the leg in long-stay intensive care unit patients. Clin Nutr 21:505–514
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berg, A., Bellander, B.M., Wanecek, M. et al. Intravenous glutamine supplementation to head trauma patients leaves cerebral glutamate concentration unaffected. Intensive Care Med 32, 1741–1746 (2006). https://doi.org/10.1007/s00134-006-0375-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0375-3