Abstract
Objective
Lung tissue deposition of intravenous ceftazidime administered either continuously or intermittently was compared in ventilated piglets with experimental bronchopneumonia.
Design
Prospective experimental study
Animals
Eighteen anesthetized and ventilated piglets
Interventions
Bronchopneumonia was produced by the intrabronchial inoculation of Pseudomonas aeruginosa characterized by an impaired sensitivity to ceftazidime (MIC 16 mg/l). Ceftazidime was administered either through a continuous infusion of 90 mg/kg per 24 h after a bolus of 30 mg/kg or by an intermittent infusion of 30 mg/kg per 8 h.
Measurements and results
Piglets were killed 24 h after the initiation of continuous ceftazidime (n = 6), and 1 h (peak, n = 6) and 8 h (trough, n = 6) after the third dose following intermittent administration. Lung tissue concentrations of ceftazidime, measured by HPLC, and lung bacterial burden were assessed on multiple postmortem lung specimens. During continuous administration ceftazidime lung tissue concentrations were 9.7 ± 3.8 μg/g. Following intermittent administration peak and trough lung tissue concentrations were, respectively, 7.1 ± 2.4 μg/g and 0.6 ± 1 μg/g. Lung bacterial burden was different after continuous and intermittent administration (median 7.103 vs. 4.102 cfu/g).
Conclusions
Continuous infusion of ceftazidime maintained higher tissue concentrations than intermittent administration.
Similar content being viewed by others
Introduction
Because of its high incidence in mechanically ventilated patients, ventilator-associated pneumonia affects length and cost of stay in intensive care units [1, 2]. Pseudomonas aeruginosa and other Gram-negative enteric bacilli, often multiresistant to antibiotics, are the most frequent causative micro-organisms [3]. Ceftazidime is a cephalosporin with a high activity against a wide spectrum of bacterias including P. aeruginosa. As with others β-lactams and unlike aminoglycosides, the bactericidal activity does not further increase when tissue concentrations largely exceed minimum inhibitory concentrations (MIC) [4]. The major determinant of antibacterial efficacy is the time during which the antibiotic concentration at the site of infection remains equal or slightly above the MIC. Theoretically the use of a continuous infusion of ceftazidime should offer the advantage of maintaining bactericidal tissue concentrations in the infected lung parenchyma. In clinical practice the bactericidal efficacy is assessed from ceftazidime plasma levels. Pharmacokinetic profile, however, may differ between the site of infection and the plasmatic compartment since the cephalosporins have been reported to achieve modest concentrations in the tracheobronchial tree [5]. Therefore it is of interest to assess whether the use of a continuous infusion of ceftazidime allows an increased deposition within the infected lung parenchyma and optimize the pharmacodynamic profile.
In a model of anesthetized piglets receiving mechanical ventilation, experimental bronchopneumonia was produced by the intrabronchial inoculation of a solution of P. aeruginosa partially resistant to ceftazidime. The aim of the study was to assess whether lung tissue concentrations are greater with continuous intravenous administration than with intermittent administration. Multiple lung specimens were collected to compare the concentrations of ceftazidime achieved in the infected lung and the antibacterial activity.
Methods
Animal preparation and bronchial inoculation
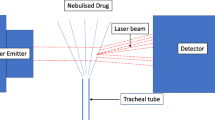
Twenty-four Largewhite-Landrace piglets (21 ± 2 kg) were anesthetized, orotracheally intubated, and mechanically ventilated in the prone position in the experimental ICU [6, 7, 8]. An intramuscular injection of 1 g ceftriaxone (Roche, Neuilly sur seine, France) was adminstered 24 h before the experiments to prevent the tracheobronchial colonization by commensal bacteria such as Pasteurella species and the onset of early ventilator-acquired pneumonia. The femoral artery was cannulated for pressure monitoring and blood sampling. Using fiberoptic bronchoscopy a suspension containing 106 cfu/mlP. aeruginosa was selectively inoculated in both middle (20 ml each) and lower lobes (30 ml each). The MIC of the inoculated strain for ceftazidime was 16 mg/l. The piglets were then ventilated with a fixed tidal volume of 15 ml/kg and no positive end-expiratory pressure. Hemodynamic parameters, airway pressures, and blood gases were determined every 3 h. All animals were treated according to the guidelines of the Department of Experimental Research of Lille University and the Guide for the Care and use of Laboratory Animals (NIH publication no. 93–23, revised 1985).
Study design and drug regimens
Ceftazidime (Fortum, Glaxo SmithKline-Beecham, Marly le Roi, France) was administered 24 h after bacterial inoculation either as a continuous infusion of 90 mg/kg over 24 h preceded by a single injection of 30 mg/kg over 30 min (continuous group, n = 6) or as an intermittent injection (intermittent group, n = 12) of 30 mg/kg every 8 h infused over 30 min. Blood samples were then collected 30 min and 2, 4, 8, 16, and 24 h after the initiation of therapy (continuous group), and 30 min and 1, 1.5, 2, 3, 4, 6, and 8 h after each intermittent infusion (intermittent group). Urine samples were collected every 8 h. Animals were treated during a 24-h period, at the end of which the animals were killed immediately in the continuous group, and 1 h (peak concentrations, n = 6) or 8 h after the last administration (trough concentrations, n = 6) in the intermittent group. Six nontreated inoculated animals (control group) were ventilated during the same period of time to assess spontaneous lung tissue bacterial burden.
Killing and postmortem analysis
Immediately after killing exsanguination was performed by direct cardiac puncture, and the lungs were exposed through a cervicothoracic incision. Five “subpleural” specimens were excised from upper, middle, and lower lobes. Each specimen was divided in two contiguous blocks. On the first cryomixed and homogenized block ceftazidime tissue concentrations were measured by high-pressure liquid chromatography [9] with correction for contaminating blood [10]. On the second block quantitative lung tissue bacterial burden was measured according to standard method [11, 12]. Specimens were aseptically weighed using a Mettler PM 2000 (Mettler-Toledo, Versailles, France). The tissue sample was homogeneized (Masticator IUL, SA Instruments, Barcelona, Spain) in brain-heart medium (1 ml/g), and aliquots of the original homogenate (100 μl) were platted on purple lactose agar, 5% blood Colombia agar, 5% blood agar to which nalidixic acid (40 mg/l) was added and “chocolate agar” with bacitracine (30 U/ml). Tenfold dilutions of the homogenate were platted to obtain the numeration and to avoid the carry-over phenomenon of the antibiotic. Counts of each identified bacterial species were expressed in colony-forming units per gram of tissue for each lung specimen. Median and interquartile range (IQR) of P. aeruginosa counts in all lung specimens were calculated. The second block was used for histological examination. Bronchopneumonic lesions characterizing each secondary pulmonary lobule were classified into three categories as previously recommended [13, 14]: healthy, mild, and severe bronchopneumonia.
Pharmacokinetic analysis
Plasma and urine ceftazidime concentrations were measured by high-performance liquid chromatography. The total area under the plasma drug concentration-time curve was calculated using the trapezoidal rules including all experimental data points.
Statistical analysis
Ceftazidime lung tissue concentrations (whose distribution was normal using the Kolmogorov–Smirnov test) and their regional distribution were analyzed using two-way analysis of variance for one grouping factor (intermittent or continuous) and one within factor (lung segment). Relationships between ceftazidime lung tissue concentrations and the histological grade of bronchopneumonia were analyzed using the Mann-Whitney test. Lung tissue bacterial burden in the continuous, intermittent, and control groups was compared using the Kruskall-Wallis test followed by Dunn's test. Statistical analysis was performed using Statview 5.0 (SAS Institute, Cary, N.C., USA). The level of statistical significance was set at p< 0.05.
Results
Clinical and pathological findings
Table 1 shows clinical and cardiorespiratory data at baseline, 24 h after bacterial inoculation, and 24 h after the first ceftazidime administration. Animals experienced a progressive and significant deterioration in gas exchange and respiratory mechanics. The proportion of secondary pulmonary lobules with severe bronchopneumonia demonstrated by microscopic examination of lung biopsy samples was 54% in the control group, 59% in the continuous group, 51% in the intermittent group (NS).
Lung deposition of ceftazidime and plasma pharmacokinetics
Peak, trough (intermittent group), and steady state (continuous group) lung tissue concentrations of ceftazidime are displayed in Fig. 1. The mean trough level in the intermittent group was 0.6 ± 1 vs. 9.7 ± 4 μg/g in the continuous group. The regional distribution of lung tissue concentrations showed no significant differences within the infected lung parenchyma. As illustrated in Fig. 2, ceftazidime lung tissue concentrations did not differ significantly in healthy lung segments and in segments with severe or mild bronchopneumonia. The mean concentration-time curves for each of the regimens are displayed in Fig. 3. The areas under the serum concentration-time curve in the intermittent and continuous groups were, respectively, 670 ± 52mg/l and 820 ± 70 mg/l per hour (NS). The tissue to plasma partition coefficients were 22 ± 5% in the intermittent group (peak level) and 17 ± 6% the continuous group (NS).
Lung tissue concentrations of cefatzidime measured at steady state 24 h after the initiation of therapy (continuous infusion group, black bars, n = 6), 1 h (light gray bars, n = 6), or 8 h (dark gray bars, n = 6) after the third infusion of 30 mg/kg per 8 h. Ceftazidime lung tissue concentrations were measured on lung specimens representative of each lobe. In the lower lobe specimens were sampled from dependent (segment 8), nondependent (segment 6), and posterocaudal (segment 10) lung regions. Data are expressed as mean ± SD
Ceftazidime (CAZ) lung tissue concentrations according to the histological grade of bronchopneumonia characterizing lung segments in the continuous infusion group (dark bars, n = 6) or at the peak level in the intermittent infusion group (gray bars, n = 6). Concentrations did not differ significantly according to the grade of bronchopneumonia
Time profiles of mean ceftazidime plasma concentrations following the administration of a continuous infusion of 90 mg/kg per day preceded by a bolus dose of 30 mg/kg (filled circles, n = 6) or the intermittent intravenous infusion of 30 mg/kg per 8 h (open circles, n = 12). Data are expressed as mean ± SD
Antibacterial efficiency of continuous and intermittent ceftazidime administration
As displayed in Fig. 4, P. aeruginosa bacterial counts did not differ significantly between lung specimens from the continuous group (median 7.103 cfu/g, IQR 0–106) and those sampled in the intermittent infusion group either at peak (median 4.102 cfu/g, IQR 0–8.10) or trough levels (median 2.102 cfu/g, IQR 0–4.103). Bacterial burden in the control group was significantly higher (median 2.104 cfu/g, IQR 6.102–5.106, p< 0.05).
Lung bacterial burden (expressed in colony forming units per gram) of P. aeruginosa (minimal inhibitory concentration to ceftazidime 16 mg/l) in lung segments collected at steady state 24 h after the initiation of ceftazidime therapy either by continuous (n = 6) or intermittent infusion (“peak”: killing 1 h after the last intravenous dose, n = 6; “trough”: killing 8 h after the last intravenous dose, n = 6) or 48 h after the bacterial inoculation in the untreated control group. Each symbol refers to a single lung specimen. Lung bacterial burden of lung segments is significantly lower in the treated groups than in the control group (p < 0.05). No significant difference is observed between lung segments sampled in animals of the continuous and intermittent infusion groups
Discussion
This study performed in anesthetized and ventilated piglets with bronchopneumonic lungs shows that a ceftazidime continuous infusion of 90 mg/kg per day provides steady-state lung tissue concentrations 16 times greater than the trough concentrations following an intermittent infusion of 30 mg/kg three times a day. Following intermittent ceftazidime infusion peak tissue concentrations were in the range of steady-state concentrations obtained by the continuous infusion. Although these concentrations were far above the MIC of sensitive P. aeruginosa, they were below the MIC of the inoculated strain (16 μg/ml) in most lung segments. Despite a partial reduction in lung bacterial burden observed in treated animals there was no difference in terms of lung bacterial killing between the two regimens of administration.
Plasma pharmacokinetics and ceftazidime lung deposition
Both modes of administrations were designed to reproduce similar conditions encountered in patients treated by ceftazidime. In the continuous infusion group mean plasma concentrations were in the same range as those measured in critically ill patients receiving a continuous ceftazidime infusion at a daily dose of 85 mg/kg [15]. In the intermittent infusion group the peak and trough plasma concentrations were also in agreement with those found in critically ill patients receiving a bolus injection of 30 mg/kg [16]. The present study confirms that continuous infusion is superior to intermittent infusion for optimizing lung deposition: lung tissue concentrations at the site of infection remained above MIC of sensitive P. aeruginosa (approx. 4 μg/ml), a critical condition for ensuring bacterial killing [4]. In the intermittent infusion group 1 hour after each administration lung tissue concentrations ranged between 8 and 10 μg/g, and plasma concentrations were 35 ±6 mg/l. Assuming that lung tissue concentrations decreased to below 4 μg/g when plasma concentrations were lower than 4 μg/ml, it can be assumed from the plasma pharmacokinetics profile (Fig. 3) that lung tissue concentration remained below the MIC of sensitive P. aeruginosa for at least 50% of the period between injections, a pharmacodynamic profile not providing an efficient bacterial killing.
Two previous studies have investigated lung deposition of ceftazidime administered either continuously or intermittently in spontaneously breathing rats with noninfected lungs [17, 18]. These experimental studies reported lung/plasma ratios higher than those obtained in the present study following continuous ceftazidime administration: 72 ±12% after the continuous administration of 30 mg/kg over 30 min [17] and 44 ± 9% after the continuous administration of 15 mg/kg per hour [18] vs. 25 ± 9% in the present study. Pharmacokinetic differences between infected piglets and noninfected rats may explain these discrepancies as well as the lack of correction for blood contamination in the two rat studies.
In patients with noninfected lungs peak ceftazidime concentrations measured in the bronchial mucosa 1 h after a single intramuscular administration of 1 g were of 8.2 ± 4.2 μg/g [19] vs. 7.1 ± 2.4 μg/g in the present study. Studies performed in patients with pneumonia generally report antibiotic concentrations measured in bronchial secretions [20] or epithelial lining fluid [15]. These sampling techniques can be easily performed in ventilated patients, represent a true estimate of the antibiotic concentration in interstitial fluid, but have the potential for over- or underestimating lung tissue concentrations due to the difficulty of evaluating accurately the dilution factor.
Methodological limitations
Our model of experimental pneumonia closely mimics human ventilator-associated pneumonia. As in critically ill patients [13, 14], lung infection was predominant in caudal and dependent parts of the lung [14, 21], consisted of infectious lesions with varying degrees of severity coexisting within the same lung segment, was induced by a bronchial inoculation resulting in a massive bronchiolar obstruction by purulent plugs, and was caused by a frequently observed bacteria, P. aeruginosa, with an impaired sensitivity to ceftazidime. Clinically, a progressive deterioration in gas exchange, respiratory mechanics, and arterial pressure was observed after 48 h of mechanical ventilation attesting of the severity of the bronchopneumonia. Histologically, lung injury was focally distributed; infected secondary pulmonary lobules coexisted with noninfected aerated lobules with a clear delineation by interlobularsepta.
A partially resistant strain of P. aeruginosa was inoculated in the present study to induce pneumonia. The necessary preexperiment administration of ceftriaxone aimed at preventing ventilator-acquired pneumonia caused by Pasteurella spp. [22] also would have inevitably prevented lung infection caused by the inoculation of a sensitive strain of P. aeruginosa. The bronchial inoculation of a strain characterized by a MIC around 8 μg/ml, however, would have been more appropriate to show differences in bacterial killing between the two modes of ceftazidime administration. Unfortunately, such a strain, necessarily of human origin and characterized by a high stability (enzymatic mechanism of resistance), could not be isolated in our laboratory.
It has been previously demonstrated that inflammation potentiates the penetration of intravenous antibiotics within infected meninges [23], vitreous cavity [24], or bronchopneumonic lungs [25, 26]. Surprisingly, lung deposition of ceftazidime was similar in lung segments with severe grades of bronchopneumonia and in noninfected lung segments or segments with mild forms of bronchopneumonia. This unexpected result may be purely artifactual. Lung tissue concentrations were measured after homogenization of tissue samples. As ceftazidime does not penetrate into cells, the extracellular antibiotic content was likely diluted in the intracellular content, and therefore the measured tissue concentrations were all the more underestimated as the infiltration of alveolar spaces by polymorphonuclear cells was massive. Assessing increased ceftazidime lung deposition would have required the measurement of extracellular concentrations of the antibiotic, which can be evaluated by dosing the antibiotic in epithelial lining fluid.
Antibacterial effects
Twenty-four hours after initiation of ceftazidime therapy, which is likely a period of treatment not long enough to fully assess the antibacterial effect of a time-dependent antibiotic, the growth of P. aeruginosa strains in the different lung segments was significantly inhibited, without difference between the two regimens: 25% of the lung specimens were sterile after intermittent infusion, 30% after continuous infusion, and 10% in the untreated control group (p< 0.05). This result is surprising since ceftazidime lung tissue concentrations measured in the different lung segments remained always below 16 μg/ml, the MIC of the inoculated P. aeruginosa. If, as stated above, the technique of lung homogenization tended to underestimate interstitial concentrations of ceftazidime, it is possible that peak tissue concentrations obtained after the last bolus of ceftazidime in the intermittent group (and likely following the initial bolus in the continuous infusion group) were above MIC in some lung segments, resulting in inhibition of bacterial growth. The likely underestimation of interstitial ceftazidime lung tissue concentrations by the lung homogenization technique also may lead to an underestimation of lung/plasma ratios and a false estimation of the time during which lung tissue concentrations remained above MIC.
An experimental model of pneumonia caused by sensitive Klebsiella pneumoniae observed a significant enhancement of bacterial killing in rats treated by a continuous infusion of ceftazidime compared to those treated by an intermittent infusion [27, 28]. In contrast, in an experimental rabbit model of endocarditis caused by strains of P. aeruginosa producing an inducible cephalosporinase no significant bacterial killing could be obtained either by a continuous or an intermittent ceftazidime infusion [29]. In an invitro infection model in which the concentrations were only one to three times the MIC of a resistant strain, incomplete bacterial killing was observed [30]. These experimental studies clearly indicate that bacterial killing in the infected tissue requires trough serum concentrations at least equal to 4 × MIC. Such bactericidal concentrations are more easily maintained by continuous than by intermittent ceftazidime infusion.
Several clinical studies in humans have reported continuous infusion of ceftazidime to be more efficient than intermittent infusion [31]. The present study shows that continuous infusion provides high lung tissue concentrations that remain stable over time. However, ceftazidime tissue concentrations were not high enough to kill partially resistant P. aeruginosa. Further studies are required to assess whether increasing the dose or changing the route of administration for nebulization may provide efficient bacterial killing.
References
Rubinstein E, Green M, Modan M, Amit P, Bernstein L, Rubinstein A (1989) The effects of nosocomial infections on the length and costs of hospital stay. J Antimicrob Chemother 9 [Suppl A]:93–100
Rouby JJ (1996) Nosocomial infection in the critically ill: the lung as a target organ. Anesthesiology 84:757–759
Cavallo JD, Leblanc F, Fabre R (2000) Surveillance of Pseudomonas aeruginosa sensitivity to antibiotics in France and distribution of beta-lactam resistance mechanisms: 1998 GERPB study. Pathol Biol (Paris) 48:472–477
Craig WA (1995) Interrelationship between pharmacokinetics and pharmacodynamics in determining dosage regimens for broad-spectrum cephalosporins. Diagn Microbiol Infect Dis 22:89–96
Cazzola M (1994) Problems and prospectives in the antibiotic treatment of lower respiratory tract infections. Pulm Pharmacol 7:139–152
Goldstein I, Bughalo MT, Marquette CH, Lenaour G, Lu Q, Rouby JJ (2001) Mechanical ventilation-induced air-space enlargement during experimental pneumonia in piglets. Am J Respir Crit Care Med 163:958–964
Goldstein I, Wallet F, Robert J, Becquemin MH, Marquette CH, Rouby J (2002) Lung tissue concentrations of nebulized amikacin during mechanical ventilation in piglets with healthy lungs. Am J Respir Crit Care Med 165:171–175
Goldstein I, Wallet F, Nicolas-Robin A, Ferrari F, Marquette CH, Rouby JJ (2002) Lung deposition and efficiency of nebulized amikacin during Escherichia coli pneumonia in ventilated piglets. Am J Respir Crit Care Med 166:1375–1381
Myers CM, Blumer JL (1983) Determination of ceftazidime in biological fluids by using high-pressure liquid chromatography. Antimicrob Agents Chemother 24:343–346
Dahlberg E (1983) Estimation of the blood contamination of tissue extracts. Anal Biochem 130:108–113
Baselski VS, el-Torky M, Coalson JJ, Griffin JP (1992) The standardization of criteria for processing and interpreting laboratory specimens in patients with suspected ventilator-associated pneumonia. Chest 102:571S-579S
Baselski VS, Wunderink RG (1994) Bronchoscopic diagnosis of pneumonia. Clin Microbiol Rev 7:533–558
Fabregas N, Torres A, El-Ebiary M, Ramirez J, Hernandez C, Gonzalez J, de la Bellacasa JP, de Anta J, Rodriguez-Roisin R (1996) Histopathologic and microbiologic aspects of ventilator-associated pneumonia. Anesthesiology 84:760–771
Rouby JJ, Martin De Lassale E, Poete P, Nicolas MH, Bodin L, Jarlier V, Le Charpentier Y, Grosset J, Viars P (1992) Nosocomial bronchopneumonia in the critically ill. Histologic and bacteriologic aspects. Am Rev Respir Dis 146:1059–1066
Boselli E, Breilh D, Rimmele T, Poupelin JC, Saux MC, Chassard D, Allaouchiche B (2004) Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med 30:989–991
Gomez CM, Cordingly JJ, Palazzo MG (1999) Altered pharmacokinetics of ceftazidime in critically ill patients. Antimicrob Agents Chemother 43:1798–1802
Miglioli PA, Xerri L, Palatini P (1991) Influence of the mode of intravenous administration on the penetration of ceftazidime into tissues and pleural exudate of rats. Pharmacology 43:242–246
Granero L, Chesa-Jimenez J, Torres-Molina F, Peris JE (1998) Distribution of ceftazidime in rat tissues. Biopharm Drug Dispos 19:473–478
Cazzola M, Gabriella Matera M, Polverino M, Santangelo G, De Franchis I, Rossi F (1995) Pulmonary penetration of ceftazidime. J Chemother 7:50–54
Byl B, Baran D, Jacobs F, Herschuelz A, Thys JP (2001) Serum pharmacokinetics and sputum penetration of amikacin 30 mg/kg once daily and of ceftazidime 200 mg/kg/day as a continuous infusion in cystic fibrosis patients. J Antimicrob Chemother 48:325–327
Wermert D, Marquette CH, Copin MC, Wallet F, Fraticelli A, Ramon P, Tonnel AB (1998) Influence of pulmonary bacteriology and histology on the yield of diagnostic procedures in ventilator-acquired pneumonia. Am J Respir Crit Care Med 158:139–147
Marquette CH, Wermert D, Wallet F, Copin MC, Tonnel AB (1999) Characterization of an animal model of ventilator-acquired pneumonia. Chest 115:200–209
Andes DR, Craig WA (1999) Pharmacokinetics and pharmacodynamics of antibiotics in meningitis. Infect Dis Clin North Am 13:595–618
Aguilar HE, Meredith TA, Shaarawy A, Kincaid M, Dick J (1995) Vitreous cavity penetration of ceftazidime after intravenous administration. Retina 15:154–159
Elman M, Goldstein I, Marquette CH, Wallet F, Lenaour G, Rouby JJ (2002) Influence of lung aeration on pulmonary concentrations of nebulized and intravenous amikacin in ventilated piglets with severe bronchopneumonia. Anesthesiology 97:199–206
Lamer C, de Beco V, Soler P, Calvat S, Fagon JY, Dombret MC, Farinotti R, Chastre J, Gibert C (1993) Analysis of vancomycin entry into pulmonary lining fluid by bronchoalveolar lavage in critically ill patients. Antimicrob Agents Chemother 37:281–286
Roosendaal R, Bakker-Woudenberg IA, van den Berg JC, Michel MF (1985) Therapeutic efficacy of continuous versus intermittent administration of ceftazidime in an experimental Klebsiella pneumoniae pneumonia in rats. J Infect Dis 152:373–378
Roosendaal R, Bakker-Woudenberg IA, van den Berghe-van Raffe M, Vink-van den Berg JC, Michel BM (1989) Impact of the dosage schedule on the efficacy of ceftazidime, gentamicin and ciprofloxacin in Klebsiella pneumoniae pneumonia and septicemia in leukopenic rats. Eur J Clin Microbiol Infect Dis 8:878–887
Robaux MA, Dube L, Caillon J, Bugnon D, Kergueris MF, Navas D, Le Conte P, Baron D, Potel G (2001) In vivo efficacy of continuous infusion versus intermittent dosing of ceftazidime alone or in combination with amikacin relative to human kinetic profiles in a Pseudomonas aeruginosa rabbit endocarditis model. J Antimicrob Chemother 47:617–622
Cappelletty DM, Kang SL, Palmer SM, Rybak MJ (1995) Pharmacodynamics of ceftazidime administered as continuous infusion or intermittent bolus alone and in combination with single daily-dose amikacin against Pseudomonas aeruginosa in an in vitro infection model. Antimicrob Agents Chemother 39:1797–1801
Nicolau DP, McNabb J, Lacy MK, Quintiliani R, Nightingale CH (2001) Continuous versus intermittent administration of ceftazidime in intensive care unit patients with nosocomial pneumonia. Int J Antimicrob Agents 17:497–504
Acknowledgements
The authors thank Jacqueline Gardillou for excellent secretariat assistance and Arnold Dive and Michel Pottier for preparation of the animals. The following members of the Experimental ICU Study Group participated in this study: C.H. Marquette, DHURE and INSERM U 416, University of Medicine, Lille, France; O. Petitjean and K. Louchahi, Department of Pharmacology, Avicenne Hospital, Bobigny, France; M.H. Becquemin, Explorations Fonctionelles Respiratoires UPRES 2397, Pitié-Salpêtrière Hospital and Université Paris VII, Paris, France; G. Lenaour, Department of Pathology, Pitié-Salpêtrière Hospital, Paris, France; P. Lechat, Department of Pharmacology, Pitié-Salpêtrière Hospital, Paris, France; P. Coriat, Department of Anesthesiology, Pitié-Salpêtrière Hospital, Paris, France; Q. Lu and Z. Maho, Réanimation Chirurgicale Pierre Viars, Pitié-Salpêtrière Hospital, Paris, France.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Cassio Girardi is a research fellow recipient of a scholarship provided by the Ministère Français des Affaires Etrangères (no. 315372 K)
Rights and permissions
About this article
Cite this article
Girardi, C., Tonnellier, M., Goldstein, I. et al. Lung deposition of continuous and intermittent intravenous ceftazidime in experimental Pseudomonas aeruginosa bronchopneumonia. Intensive Care Med 32, 2042–2048 (2006). https://doi.org/10.1007/s00134-006-0272-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0272-9