Abstract
Objective
Central venous oxygen saturation (ScvO2) in initial resuscitation is included in the Surviving Sepsis Campaign guidelines. ScvO2 monitoring has also been suggested to be comparable to mixed venous oxygen saturation (SvO2) for clinical purposes. The aim of our study was to assess the correlation and agreement of ScvO2 and SvO2 and compare ScvO2–SvO2 difference to lactate, oxygen-derived and hemodynamic parameters in early septic shock in ICU after initial resuscitation.
Design and setting
Prospective clinical study with 16 patients with septic shock at two university hospital ICUs. A dose of norepinephrine over 0.1 μg/kg/min was required for inclusion.
Measurements and results
Five paired ScvO2 and SvO2 samples at 6-h intervals, altogether 72 samples, were collected during 24 h. The mean SvO2 was below the mean ScvO2 at all time points. Bias of difference was 4.2% and 95% limits of agreement ranged from –8.1% to 16.5%. The difference correlated significantly to CI and DO2.
Conclusions
The difference between paired ScvO2 and SvO2 varies highly. Therefore, SvO2 may not be estimated on the basis of ScvO2 in treatment of septic shock after resuscitation period in ICU.
Similar content being viewed by others
Introduction
Early goal-directed therapy (EGDT), aiming at central venous oxygen saturation (ScvO2) over 70% during the first 6 h, has been shown to reduce mortality among patients with severe sepsis and septic shock [1], and the use of ScvO2 in initial resuscitation has been applied also to sepsis guidelines [2]. While ScvO2 is an excellent tool in the resuscitation period of shock, there is still controversy as to whether it is a suitable parameter for follow-up afterwards during ICU treatment.
Mixed venous oxygen saturation (SvO2) is commonly used to monitor patient hemodynamics in ICUs. SvO2 predicts mortality in sepsis [3, 4], although there is no clear evidence of its value as a treatment target. Instead of SvO2, ScvO2 monitoring has been suggested to be useful for clinical purposes [5, 6]. This is mainly based on the fact that low ScvO2 indicates even lower SvO2, and that the trends of ScvO2 generally agree with those of SvO2 [6, 7, 8]. However, most studies that have investigated the relationship of ScvO2 and SvO2 in critically ill patients have shown marked differences between the two, with ScvO2 being higher than SvO2 [9, 10, 11, 12]. Individual values in shock state may differ up to 18–22% [6, 10, 12]. In fact, none of the previous studies confirms ScvO2 either as an independent predictor of mortality or as a measure to guide the treatment after initial resuscitation phase.
Our assumption is that an acceptable level of ScvO2 during ICU treatment, when ScvO2 is mostly normal or elevated, is not straightforward, and ScvO2 cannot be used as a surrogate of SvO2 or as a target in the treatment of septic shock after the resuscitation period. Although this difference has been evaluated in a few previous investigations (Table 1), no study has assessed its value in a homogeneous group of early severe septic shock defined as a moderate need of norepinephrine to maintain adequate perfusion pressure. The aim of our study was to evaluate the correlation and agreement of ScvO2 and SvO2 and also compare the ScvO2–SvO2 difference to lactate, oxygen-derived and hemodynamic parameters during early severe septic shock in ICU after initial resuscitation.
Materials and methods
Our prospective study was conducted in two Finnish ICUs from November 2004 to June 2005 after approval by the local ethics committees. Sixteen patients with septic shock fulfilling the criteria set by the APCCP/SCCM Consensus Conference [13] – known or suspected infection with systemic inflammatory response syndrome, sepsis-induced hypotension, and need for vasopressor after adequate fluid resuscitation – were included. Norepinephrine dose over 0.1 μg/kg/min for maintaining mean arterial blood pressure over 65 mmHg was required for inclusion. Standard management of septic shock included fluid resuscitation and the use of norepinephrine as the primary vasopressor and dobutamine as the primary inotrope according to the SCCM sepsis guidelines [2]. The treatment targets were mean arterial pressure (MAP) over 65 mmHg, pulmonary artery occlusion pressure (PAOP) of 12–16 mmHg, and SvO2 over 65%. All patients required ventilator treatment. Propofol or midazolam infusions combined with fentanyl were used for sedation.
An arterial catheter and a four-lumen pulmonary artery catheter (PAC) with introducer (7.5 F Paceport Oximetry TD Catheter with AMC Thromboshield 780HF75, Edwards Lifesciences LCC, Irvine, CA, USA) were inserted for hemodynamic monitoring. A typical wedge pressure tracing with the balloon inflated and chest X-ray confirmed the correct placement of the catheter in the zone-3 position. The correct location of the introducer tip in the superior vena cava (SVC) was confirmed with chest X-ray. For the measurements, SvO2 samples were simultaneously drawn slowly from the distal port of the unwedged PAC, ScvO2 samples from the side port of the introducer and arterial samples via the arterial catheter. The side port of the introducer instead of the proximal port of the PAC was chosen for more reliable placement in the SVC.
Baseline samples were drawn immediately after patient inclusion and every 6 h thereafter up to 24 h. Altogether five paired ScvO2 and SvO2 samples were obtained for each patient unless the patient expired or because of technical reasons. Blood gas analyses were performed and oxygen saturations were determined photospectrometrically with a CO oximeter (Ciba-Corning 850 and 855, Medfield, MA, USA). Hemodynamic measurements were performed immediately after blood sampling. Cardiac output (CO) was determined with thermodilution method by injecting 10 ml of isotonic saline through proximal port of PAC. Ice-cold solution was used if cardiac index (CI) was found to be below 2.5 l/min/m2. CI was computed by dividing CO by the patient's body surface area. Three to five measurements were obtained and averaged. Oxygen extraction rates (O2ER), oxygen delivery (DO2) and oxygen consumption (VO2) were calculated by using standard formulas. Arterial plasma lactate level was measured with a photometric method.
Statistical analysis
To evaluate the agreement between ScvO2 and SvO2, bias (systematic error) was determined by the method described by Bland and Altman [14], where bias is expressed as the mean of the differences between paired values (Δ[ScvO2–SvO2]). Ninety-five percent limits of agreement were calculated. Correlation between ScvO2 and SvO2 was determined with intraclass correlation, and comparison of saturation values in different time points and according to different levels of ScvO2 was performed with the nonparametric Friedman test. The normality of continuous variables was tested with the Kolmogorow–Smirnov test. Δ[ScvO2–SvO2] was compared to common hemodynamic and perfusion variables with Spearman correlation for assessing possible factors affecting to the ScvO2–SvO2 gradient.
Results
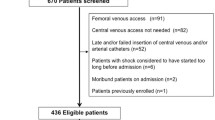
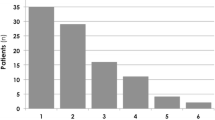
Altogether 72 paired blood samples were obtained from 16 patients with septic shock. Patient characteristics are shown in Tables 2 and 3. The source of sepsis was pneumonia in six cases (38%), peritonitis in six (38%), meningitis in one (6%), pyelonephritis in one (6%), and undetermined or unknown in two cases (13%). Five patients (31%) had positive blood culture. The first blood samples were taken 5.0 h (range 2.8–14.0 h) after ICU admission and 8.5 h (3.3–12.6 h) after onset of severe sepsis. One patient died within 24 h. Five paired samples were missed due to technical reasons. The hospital mortality was 38% (6 of 16).
Simultaneous values of ScvO2 and SvO2 are shown in Fig. 1. The intraclass correlation of paired ScvO2 and SvO2 was highly significant (intraclass correlation coefficient 0.89, 95%CI 0.82–0.93, p < 0.001). Mean SvO2 was below mean ScvO2 at all time points (Fig. 2). The agreement between ScvO2 and SvO2 by Bland–Altman plot is presented in Fig. 3, where the bias of difference is 4.2% and 95% limits of agreement were –8.1% to 16.5%. The Bland–Altman plots at each time point separately showed bias of difference from 1.9% to 5.6% (95% limits of agreement ranging from –14.1% to –5.2% to 14.5%–17.9%). These are shown in the Electronic Supplementary Material (ESM, S.F1–F5) as well as the individual oximetric and hemodynamic values during study (ESM, S.T1). Δ[ScvO2–SvO2] correlated inversely to CI (p = 0.036) (Fig. 4) and to DO2 (p = 0.007), but no correlation to other measured variables or to dose of norepinephrine was detected (Table 4).
No significant change was found in average Δ[ScvO2–SvO2] over time (Fig. 2), but Δ[ScvO2–SvO2] was dependent on the level of ScvO2 when values of < 60%, 60–70%, 70–80% and > 80% were analyzed separately. The mean Δ[ScvO2–SvO2] values were 5.2%, 1.5%, 2.9% and 8.1%, respectively. This showed statistical significance (p = 0.003).
Changes in ScvO2 and SvO2 were parallel in 55% (95% CI 41%–69%) of two successive measurements (both measurements changed at the same time to the same direction compared with previous measurements, ESM S.F6).
Discussion
Our study showed that in early severe septic shock, despite a statistically significant correlation, the agreement of ScvO2 and SvO2 is not adequate. For clinical use this variability makes the accurate conception of the values difficult. Δ[ScvO2–SvO2] was not dependent on the time point of treatment but the difference varied according to the level of ScvO2, being greatest in very low and high values. Low oxygen delivery and cardiac output led to increased difference between ScvO2 and SvO2. In addition, for clinical decisions it is noteworthy that ScvO2 and SvO2 changed in the same direction in only 55% of cases.
ScvO2 is a mixture of venous blood from the upper body, while SvO2 reflects the flow-weighted oxygen balance of the whole body. In early shock, despite its etiology, both saturation values are commonly decreased and thus ScvO2 has been shown to be excellent in emergency departments to detect a shock in emergency situations [15, 16, 17, 18]. ScvO2 reflects accurately hypovolemia, which is common in septic patients first presenting in ED [19, 20]. The EGDT study showed that ScvO2 is useful in guiding the resuscitation of early septic shock targeting to ScvO2 over 70% during the first 6 h in ED [1]. However, whether we can extrapolate this goal to patients who are treated after the resuscitation period in ICUs is not clear at all.
In the study conducted by Reinhart et al., evaluating critically ill patients during an average of 56 h with continuous measurement of ScvO2, over 87% of the values of nonsurvivors and 95% of those of survivors were over 70% [6]. According to our opinion this may suggest that ScvO2 of 70% as a treatment goal in septic shock after the resuscitation period is insensitive for the detection of tissue oxygen demand. In our previous study we showed that the area of SvO2 values under 70% in the first 24 h of treatment in ICU was a significant predictor of mortality independent of cardiac output or arterial saturation [4]. Because Δ[ScvO2–SvO2] varies extensively, the estimation of adequacy of SvO2 on the basis of ScvO2 level seems impossible. In general, this pronounced variability is in agreement with other studies, although inclusion criteria similar to our study have not been used, and also non-septic critically ill patients have been included in most of them. Table 1 shows the degree of bias and limits of agreement (ranging from –18 to +21%) of paired SvO2 and ScvO2 in previous studies. However, there is only indirect evidence that the use of SvO2 to guide the treatment is beneficial either. Pölönen and colleagues found reduced hospital stay and morbidity with SvO2-targeted goal-oriented postoperative treatment after cardiac surgery [21], but using SvO2 as a treatment goal has not improved outcome in prospective trial [22].
The gradient between SvO2 and ScvO2 depends on the oxygen consumption and the amount of blood flow in various organs between the upper and the lower body. We found a reversed correlation of Δ[ScvO2–SvO2] to CI and DO2. Distribution of blood flow in low-flow condition away from renal, splanchnic and mesenteric circulation toward cerebral and myocardial perfusions are likely to explain this phenomenon. The significant differences in CI and DO2I depending on the difference between ScvO2 and SvO2 were also noted by Turnaoglu and colleagues [9], and the correlation between SvO2 and ScvO2 in general has been poorer in hypodynamic shock [12, 23]. In sepsis, the possible reasons for Δ[ScvO2–SvO2] also include increased oxygen consumption in the hepatosplanchnic region and mixing of the less saturated blood from the coronary sinus in the right atrium, which both decrease the SvO2, while decreased cerebral oxygen uptake during sedation increases ScvO2.
Tissue hypoxia in the splanchnic area is considered to be an important cofactor in the pathogenesis of multiple organ failure in sepsis [24], and inadequate regional perfusion in the hepatosplanchnic area may also influence the outcome [25]. Hepatic venous saturation may be highly depressed in sepsis, and perfusion is even further influenced by the use of vasoactive treatment [26, 27, 28]. The hypoperfusion within the hepatosplanchnic region may persist even after the early correction of hypovolemia when global hemodynamic variables appear adequate [29, 30]. Regional hypoperfusion is not detected accurately with SvO2 measurement [26, 27], but theoretically it is better detected with SvO2 than with ScvO2. To the best of our knowledge, the relationship between oximetric values from hepatic vein or inferior vena cava and ScvO2 have been investigated only in one study. In this study the difference was more pronounced between inferior vena cava and ScvO2 than for SvO2, but the patient population was small [12]. Nearly 20% of abrupt changes over 10% of SvO2 cannot be detected with ScvO2 in severe sepsis or septic shock [31], and 33% of sudden changes of SvO2 cannot be explained by therapeutic interventions or alterations in hemodynamic measurements. These differences are probably caused by fluctuations in tissue oxygen demands in hepatosplanchnic region [32].
Coronary venous oxygen saturation is very low in the normal situation due to the high oxygen extraction rate of the myocardium [33]. In sepsis, coronary blood flow is increased as a consequence of coronary vasodilatation while oxygen extraction remains high [34]. This leads to the elevation of Δ[ScvO2–SvO2] by the mixing of coronary venous blood of lower oxygen saturation in the right atrium.
The impact of coronary mixing was highlighted in a recent trial that detected a decrease not only in oxygen saturations but also in lactate concentrations when comparing samples from proximal and distal ports of PAC in critically ill patients. Because the lactate concentration in coronary venous blood is very low, unlike in inferior venous blood, the authors suggested that the decrease between ScvO2 and SvO2 originate from mixing the coronary blood, not the inferior venous blood. They concluded that the phenomenon might reflect changes in myocardial energy requirement [35]. Insufficient oxygen supply to the myocardium with respect to its metabolic needs may itself lead to diminished contractility and low output [36], which in turn may further increase Δ[ScvO2–SvO2].
A limitation of our study is small sample size. However, our patient group was homogeneous with regard to the severity and timing of septic shock. Concerning clinical decisions, not a statistically significant correlation but individual bias between the measurements is relevant, and therefore our results, a clear bias and wide limits of agreement between paired ScvO2 and SvO2, are of importance in septic shock. In correlation analysis, samples are pooled from several time points, which may have affected the results. However, we find that unlikely since the results are in accordance with previous findings.
In conclusion, both ScvO2 and SvO2 are low in early septic shock and are useful parameters in the detection of shock and during the resuscitation period. Later in the ICU treatment period, the difference between these two oxygen saturation parameters varies highly even with comparable vasoactive treatment. Therefore, SvO2 is not estimated on the basis of ScvO2. However, the usefulness of SvO2 itself in guiding the treatment in septic shock needs to be re-evaluated in a randomized trial using goal-oriented therapy and continuous measurements.
References
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, Ramsay G, Zimmerman JL, Vincent JL, Levy MM (2004) Surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med 32:858–873
Heiselman D, Jones J, Cannon L (1986) Continuous monitoring of mixed venous oxygen saturation in septic shock. J Clin Monit 2:237–245
Varpula M, Tallgren M, Saukkonen K, Voipio-Pulkki LM, Pettila V (2005) Hemodynamic variables related to outcome in septic shock. Intensive Care Med 31:1066–1071
Reinhart K, Bloos F (2005) The value of venous oximetry. Curr Opin Crit Care 11:259–263
Reinhart K, Kuhn HJ, Hartog C, Bredle DL (2004) Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med 30:1572–1578
Dueck MH, Klimek M, Appenrodt S, Weigand C, Boerner U (2005) Trends but not individual values of central venous oxygen saturation agree with mixed venous oxygen saturation during varying hemodynamic conditions. Anesthesiology 103:249–257
Tahvanainen J, Meretoja O, Nikki P (1982) Can central venous blood replace mixed venous blood samples? Crit Care Med 10:758–761
Turnaoglu S, Tugrul M, Camci E, Cakar N, Akinci O, Ergin P (2001) Clinical applicability of the substitution of mixed venous oxygen saturation with central venous oxygen saturation. J Cardiothorac Vasc Anesth 15:574–579
Edwards JD, Mayall RM (1998) Importance of the sampling site for measurement of mixed venous oxygen saturation in shock. Crit Care Med 26:1356–1360
Faber T (1995) Central venous versus mixed venous oxygen content. Acta Anaesthesiol Scand Suppl107:33–36
Lee J, Wright F, Barber R, Stanley L (1972) Central venous oxygen saturation in shock: A study in man. Anesthesiology 36:472–478
American College of Chest Physicians/Society of Critical Care Medicine consensus conference: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis (1992) Crit Care Med 20:864–874
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Rady MY, Rivers EP, Martin GB, Smithline H, Appelton T, Nowak RM (1992) Continuous central venous oximetry and shock index in the emergency department: use in the evaluation of clinical shock. Am J Emerg Med 10:538–541
Ander DS, Jaggi M, Rivers E, Rady MY, Levine TB, Masura J, Gryzbowski M (1998) Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 82:888–891
Goldman RH, Klughaupt M, Metcalf T, Spivack AP, Harrison DC (1968) Measurement of central venous oxygen saturation in patients with myocardial infarction. Circulation 38:941–946
Scalea TM, Hartnett RW, Duncan AO, Atweh NA, Phillips TF, Sclafani SJ, Fuortes M, Shaftan GW (1990) Central venous oxygen saturation: a useful clinical tool in trauma patients. J Trauma 30:1539–1543
Madsen P, Iversen H, Secher NH (1993) Central venous oxygen saturation during hypovolaemic shock in humans. Scand J Clin Lab Invest 53:67–72
Perko G, Payne G, Linkis P, Jorgensen LG, Landow L, Warberg J, Secher NH (1994) Thoracic impedance and pulmonary atrial natriuretic peptide during head-up tilt induced hypovolaemic shock in humans. Acta Physiol Scand 150:449–454
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J (2000) A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg 90:1052–1059
Gattinoni L, Braggi L, Pelosi P, Latini R, Tognoni G, Pesentii A, Fumagalli R (1995) A trial of goal-oriented hemodynamic therapy on critically ill patients. N Engl J Med 333:1026–1031
Scheinman M, Brown M, Rapaport E (1969) Critical assessment of use of central venous oxygen saturation as a mirror of mixed venous oxygen in severely ill cardiac patients. Circulation 40:165–172
Ackland G, Grocott M, Mythen M (2000) Understanding gastrointestinal perfusion in critical care: so near, and yet so far. Crit Care 4:269–281
Marik PE (1993) Gastric intramucosal pH. A better predictor of multiorgan dysfunction syndrome and death than oxygen-derived variables in patients with sepsis. Chest 104:225–229
Meier-Hellmann A, Hannemann L, Specht M, Schaffartzik W, Spies C, Reinhart K (1994) The relationship between mixed venous and hepatic venous O2 saturation in patients with septic shock. Adv Exp Med Biol 345:701–707
Ruokonen E, Takala J, Uusaro A (1991) Effect of vasoactive treatment on the relationship between mixed venous and regional oxygen saturation. Crit Care Med 19:1365–1369
De Backer D, Creteur J, Silva E, Vincent JL (2003) Effects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: Which is best? Crit Care Med 31:1659–1667
Edouard AR, Degremont A-C, Duranteau J, Pussard E, Berdeaux A, Samii K (1993) Heterogeneous regional vascular responses to simulated transient hypovolemia in man. Intensive Care Med 20:414–420
Oud L, Haupt MT (1999) Persistent gastric intramucosal ischemia in patients with sepsis following resuscitation from shock. Chest 115:1390–1396
Martin C, Auffray JP, Badetti C, Perrin G, Papazian L, Gouin F (1992) Monitoring of central venous oxygen saturation versus mixed venous oxygen saturation in critically ill patients. Intensive Care Med 18:101–104
Krafft P, Steltzer H, Hiesmayr M, Klimscha W, Hammerle AF (1993) Mixed venous oxygen saturation in critically ill septic shock patients: the role of defined events. Chest 103:900–906
Schremmer B, Dhainaut JF (1990) Regulation of myocardial oxygen delivery. Intensive Care Med 16:S157–S163
Dhainaut JF, Huyghebaert MF, Monsallier JF, Lefevre G, Dall'Ava-Santucci J, Brunet F, Villemant D, Carli A, Raichvarg D (1987) Coronary hemodynamics and myocardial metabolism of lactate, free fatty acids, glucose, and ketones in patients with septic shock. Circulation 75:533–541
Gutierrez G, Chawla LS, Seneff MG, Katz NM, Zia H (2005) Lactate concentration gradient from right atrium to pulmonary artery. Critical Care 9:R425–R429
Schremmer B, Dhainaut JF (1990) Regulation of myocardial oxygen delivery. Intensive Care Med 16:157–163
Chawla LS, Zia H, Gutierrez G, Katz NM, Seneff MG, Shah M (2004) Lack of equivalence between central and mixed venous oxygen saturation. Chest 126:1891–1896
Acknowledgements
The study was supported by EVO grant from Helsinki University Hospital.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Varpula, M., Karlsson, S., Ruokonen, E. et al. Mixed venous oxygen saturation cannot be estimated by central venous oxygen saturation in septic shock. Intensive Care Med 32, 1336–1343 (2006). https://doi.org/10.1007/s00134-006-0270-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0270-y