Abstract
Objective
The organizational structure of health care facilities has been shown to affect outcome in critically ill patients. We evaluated the association between structures, treatments and outcomes in a large cohort of critically ill patients.
Design
Prospective multicentre cohort study.
Patients and setting
A total of 26,186 patients consecutively admitted to 31 intensive care units (ICUs) in Austria from January 1998 through December 2000.
Measurements and results
The ICUs were divided into three groups according to the size and function of the hospital: community hospitals and specialized trauma centers (group A); central referral hospitals (group B); and teaching hospitals (group C). Group C patients exhibited a significantly higher risk-adjusted mortality (O/E ratio). Although severity of illness at admission in groups B and C was similar, group C patients received significantly more invasive diagnostic and therapeutic interventions throughout their ICU stay: For 7 of 10 invasive interventions identified, odds ratios for group C vs group B patients were significantly increased, even after adjustment for age, gender, severity of illness and reason for admission (odds ratios 1.2–13.1; all 95% CIs >1). Risk-adjusted multivariate analysis confirmed that six of these invasive interventions were independently associated with mortality. Furthermore, nurse-to-patient ratios did not differ between groups, leading to a significantly increased nursing workload in group C ICUs.
Conclusions
Several invasive interventions were independently associated with increased mortality. Our results provide strong evidence that this association was responsible in part for the increased risk-adjusted mortality in group C patients.
Similar content being viewed by others
Introduction
Intensive care medicine is a relatively young specialty, originating and growing in the second half of the twentieth century. It is believed that no more than 10–20% of all treatments and interventions performed in intensive care units (ICUs) have been proved effective by scientific evidence. Other issues are less relevant if the care being provided is ineffective or harmful; thus, evaluating the effectiveness and efficiency of our therapies must be a top priority in intensive care research.
Besides patient-related factors, such as age, chronic disease status and severity of illness at admission, several studies have provided evidence that the organizational structure of ICUs affects outcome [1]. For example, Bastos et al. [2] showed that the amount of technology in the ICU influences risk-adjusted outcome, at least in Brazil: the less technology available, the higher the risk-adjusted mortality. Furthermore, several studies have highlighted the importance of nursing staff. Amaravadi et al. [3] evaluated 35 centres for the effect of the nurse-to-patient ratio on outcome of patients undergoing esophagectomy: A ratio of <1:2 (i.e. one nurse caring for more than two patients) was significantly associated with an increased incidence of complications. The same investigators confirmed these results for patients undergoing abdominal aortic surgery [4, 5] and hepatectomy [6]. In the UK [7] a strong association was found between occupancy rate and outcome in critically ill infants: patients admitted at higher occupancy rates exhibited a dramatically increased risk-adjusted mortality.
These results suggest that differences in structures and treatments between centres may have a profound effect on outcome of critically ill patients. The aim of this study was thus to evaluate the association between structures, treatment and outcome in a large cohort of critically ill patients in Austrian ICUs.
Materials and methods
Database
Data were collected by the Austrian Center for Documentation and Quality Assurance in Intensive Care Medicine (ASDI), a nonprofit organization that has established an intensive care database and benchmarking project [8, 9]. The prospectively collected data included sociodemographic data, such as age, gender and chronic conditions; the reason for admission, which was recorded according to a predefined list of medical and surgical diagnoses [10]; severity of illness, as measured by the Simplified Acute Physiology Score II (SAPS II [11]); numbers and severity of organ dysfunction, as measured by the Logistic Organ Dysfunction system (LOD [12]); level of provided care, as measured by the Simplified Therapeutic Intervention Scoring System (TISS-28) [13]; length of ICU and hospital stay; and outcome data, including survival status at ICU and hospital discharge.
Data collection for the benchmarking project is continuous. The number of participating ICUs varies from year to year, because participants sometimes lack time and resources to assess important data. Forty-one ICUs were initially included in the data collection for this study, but 10 participated only temporarily and were removed from the database before analysis; thus, data on all patients consecutively admitted to 31 Austrian ICUs from 1 January 1998 to 31 December 2000 were included in this study. The ICUs were divided into three groups according to the size and function of the hospital: group A (community hospitals and specialized trauma centres) had <300 beds (n=13); group B (central referral hospitals) had 300–599 beds (n=10); and group C (teaching hospitals) had ≥600 beds (n=8). Twenty-four ICUs were in anaesthesiology departments and 7 were in medical departments. It is important to note that all Austrian ICUs use a closed-policy approach, i.e. each ICU has a designated medical director and intensive care physicians covering the ICU around the clock.
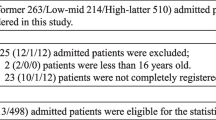
A total of 29,249 patients were admitted to the 31 ICUs during the study period. For patients who were admitted more than once (n=1374), only the first admission was included. Patients who were <18 years of age (n=648), those with records that lacked an entry in the field “hospital outcome” (n=303) and those without a valid SAPS II score (n=738) were excluded. Since no additional interventions were performed, the need for informed consent was waived by the institutional review board.
Outcome measures
To check for a possible effect of organizational structures on outcome, we used additional questionnaires to evaluate available resources in three areas: hospital services; ICU facilities; and ICU nursing staff. Hospital services included such resources as transportable X-ray, computed tomography, angiography, echocardiography, blood bank, in-house laboratory and operating rooms. The ICU facilities included number of available beds and per-bed availability of ICU devices necessary to provide organ support: mechanical ventilation; invasive haemodynamic monitoring; and renal replacement therapy. The ICU nursing staff was evaluated with the use of three indices. The nurse-to-patient ratio, i.e. the number of beds assigned to one nurse, was calculated according to a formula published by Moreno and Miranda [14]. The efficient use of nursing personnel was evaluated through the work-utilization ratio—the ratio of the produced workload to the available workload in the ICU [14]. Occupancy rate was calculated as the percentage of occupied beds per day [15].
To check for a possible effect of treatment on outcome, we identified ten procedures and interventions from the TISS-28 that are invasive and could possibly harm a patient: mechanical ventilation; single and multiple vasoactive medication; peripheral arterial catheterization; pulmonary artery catheterization; central venous line; renal replacement therapy; intracranial pressure measurement; single specific intervention in the ICU; and multiple specific interventions in the ICU. Although other TISS-28 items might also influence outcome, they are not regarded as generally invasive and/or comparable for all patients; e.g. a “diagnostic intervention outside the ICU” might harm an unstable cardiovascular or respiratory patient who needs a high level of organ support but be harmless for an extubated patient who is awaiting discharge to the normal ward.
Data quality
To assess the reliability of data collection, we sent an independent observer to each unit to obtain SAPS II data from the clinical charts of a random sample of patients. Variance-component analyses with the random factors “units”, “patients within units” and “observers within units” were performed (SAS, procedure varcomp) as described previously [8]. To assess the completeness of the documentation, we calculated the number of missing parameters for the SAPS II score.
The quality of the recorded data was satisfactory with respect to both completeness of records and interrater variability. The median number of missing parameters necessary for the calculation of the SAPS II was 0 (interquartile range 0–2). Interrater quality control indicated an overall excellent grade of agreement: for all tested variables, practically no deviations between the observers were detected, the contribution to the variability being less than 1%. Further details have been reported elsewhere [16].
Statistical analysis
Statistical analysis was performed using the SAS system (version 8e). For tests of statistical significance, the Kruskal-Wallis test was used to compare quantitative variables between hospitals of different size. The chi-square test and Fisher exact test were used when appropriate. A p value <0.05 was considered significant. Unless otherwise specified, descriptive results are expressed as median and first and third quartiles. Observed-to-expected (O/E) mortality ratios were calculated by dividing the number of observed deaths per group by the number of SAPS II-predicted deaths per group. The 95% confidence intervals (CIs) were calculated according to a formula described by Hosmer and Lemeshow [17].
We used linear regression analysis to evaluate the impact of nursing staff availability and hospital size (as a possible proxy for resource availability) on outcome. Each treatment centre was entered as a single observation (n=18 ICUs from groups B and C). The ICUs were weighted according to the number of patients they had admitted. Risk-adjusted hospital mortality per ICU (O/E ratio) was used as the dependent variable. Independent variables were nurse-to-patient ratio, work-utilization ratio and occupancy rate. Hospital size (groups B and C) was also entered. Other structural parameters for which no differences between groups and no association with outcome could be found were not included (see Results).
Logistic regression analysis was used to further explore the effect of invasive procedures on outcome in group B and group C patients. Each patient was entered as a single observation. To exclude case mix factors as possible confounders, we adjusted the model for age, gender, severity of illness and reason for admission. Vital status at hospital discharge (hospital mortality) was used as the dependent variable. Procedures and interventions from the TISS-28 that were previously identified as invasive were entered as independent variables, using binary coding to indicate whether a specific intervention was performed at least once during the ICU stay. In all regression analyses, a p value <0.05 was considered significant.
Results
Data from 26,186 patients admitted to the 31 ICUs during the study period were included in the analysis (Table 1). Most of the ICUs admitted both medical and surgical patients. In group B, more patients were admitted after medical procedures (and fewer after surgical procedures) than in the other two groups (Table 1).
Organizational structures
Group A (the smallest) hospitals had significantly fewer services available than group B and group C hospitals: they were less likely to have the capability to perform angiography, less likely to have a blood bank and less likely to have a central in-house laboratory (Table 2). There was no significant difference in services between group B and group C hospitals. No differences between the three groups were found with respect to equipment available in the ICU (Table 2).
The nurse-to-patient ratio was not significantly different between the three groups (Table 3). The work-utilization ratio increased significantly from group A to group C (Table 3). Furthermore, ICUs located in group C hospitals exhibited a significantly higher occupancy rate (Table 3). No differences between the three groups were found with respect to availability of intensive care specialists and physicians in intensive care training (data not shown).
Patients and treatments
Patients admitted to ICUs in group A presented with fewer organ dysfunctions and a lower severity of illness at admission, compared with patients admitted to group B and group C ICUs. Despite a similar severity of illness between group B and group C patients, patients in group C received a significantly higher level of care (Table 1). This difference was due to the more frequent use of invasive monitoring and organ support measures. All TISS-28 items that were identified as being invasive and thus potentially harmful were applied to patients in group C ICUs significantly more often (odds ratios 1.2–13.1; all 95% CIs >1 [Table 4]). To exclude differences in case mix as the reason for the difference in use of invasive procedures, we recalculated odds ratios after adjusting for age, gender, severity of illness at admission and reason for admission. After these adjustments, 7 of the 10 odds ratios remained significant. Corresponding unadjusted and adjusted odds ratios are given in Table 4.
Group C patients also had significantly higher ICU and hospital mortality rates, compared with groups A and B. Even after adjustment for the severity of illness, hospital mortality remained significantly higher in group C: O/E ratios were 0.88 (0.84–0.92), 0.83 (0.80–0.87) and 0.99 (0.96–1.02) for groups A, B and C, respectively (Fig. 1). To check for an artefact (lack of prognostic accuracy of the SAPS II), we further evaluated O/E ratios using a customized model for the Austrian ICU population [18], which did not alter the results (data not shown).
Multivariate analysis
In the multivariate linear regression analysis of the ICU-specific variables, neither the nursing staff factors (nurse-to-patient ratio, work-utilization ratio, occupancy rate) nor the hospital group were significantly associated with outcome (data not shown).
Logistic regression analysis (each patient individually entered) revealed that six items were significantly associated with mortality (Table 5): renal replacement therapy; intracranial pressure measurement; pulmonary artery catheterization; multiple vasoactive medication; central venous line; and multiple specific interventions in the ICU. Mechanical ventilation was not significantly associated with mortality but showed a tendency in that direction [P=0.07; odds ratio 1.18 (range 0.99–1.40)].
Discussion
To our knowledge, this is the largest cohort study to date to evaluate the association between organizational structures, treatments and outcomes in critically ill patients. Our reason for dividing ICUs into groups of hospital size was to compare ICUs at a similar level of available resources and function. Group A hospitals deliver a narrow spectrum of medical care to the local community and have limited resources. Referral hospitals (group B) provide a broader spectrum of medical care and are thus better equipped. Teaching hospitals (group C) offer all medical services and are thus not only the largest but also the best equipped. One might therefore expect that ICUs in group C hospitals would be the most capable of providing a high quality of intensive care and therefore have the most positive impact on the outcome of their patients.
None of the ICU facilities or hospital services was associated with outcome in univariate analysis. This finding is not surprising in a central European country with a relative abundance of health care resources; however, what was surprising was that ICU patients in group C hospitals received significantly more diagnostic and therapeutic interventions per patient and per day. This was despite the fact that their severity of illness at admission was no different from that of patients in group B (Table 1); odds ratios for patients treated in group C ICUs to undergo invasive procedures were greatly increased for all ten interventions studied. Even after adjustment for age, gender, severity of illness and reason for admission, 7 of the 10 interventions were still applied significantly more often to patients in group C (Table 4).
Evaluation of the work-utilization ratio in our study revealed that the availability of nursing staff did not differ significantly between the three groups (Table 3). As a net result, a nurse in a group C ICU generated approximately 30% more TISS-28 points than a nurse in groups A or B.
To further explore these results, we used a case mix-adjusted multivariate approach. The results of the patient-centred analysis proved the association of the invasive procedures with outcome: six interventions were significantly associated with mortality (Table 5), and one intervention (mechanical ventilation) narrowly missed being significant. How can we explain these results?
Several recent studies have shown that interventions carry inherent risks which possibly influence outcome. For example, central venous lines (CVL), although often regarded as a simple, routine procedure, are known to cause a variety of potentially life-threatening complications [19]. These complications can be related to either the insertion or the use of CVL [20, 21]. Bacteraemia occurs in approximately 1% of cases (amounting to approximately 50,000 cases each year in the United States), with an attributable mortality of 10–20% [22, 23]. Pulmonary artery catheterization is an invasive measure with acknowledged risks [19]. The demonstration of a worse instead of a better outcome for patients treated with pulmonary artery catheterization in at least one study [24] has led to an ongoing discussion of the effectiveness and efficiency of this procedure [25, 26].
It was recently demonstrated that patients receiving renal replacement therapy (RRT) have significantly increased mortality rates when compared with matched control subjects [16]. This excess mortality might be attributable not only to acute renal failure, but also to the treatment itself: RRT has a profound effect on the antioxidant state of critically ill patients by depleting nutritional antioxidants and by generating radical oxygen species in the extracorporeal circuit [27, 28]. Moreover, the activation of several physiological cascade systems results in an inflammatory reaction that induces protein catabolism and compromises immunocompetence [29]. All these phenomena can increase morbidity and, therefore, mortality.
Mechanically ventilated patients have a high risk of developing complications, such as ventilator-associated pneumonia (VAP). A recent consensus conference estimated that the incidence of VAP, using a clinical definition, is approximately 7 cases per 1000 ventilator days [30]. Moreover, although the mortality attributable to VAP has not been firmly established, some investigators believe that these patients have a two to ten times higher risk of death compared with patients not on mechanical ventilation [31]. An international multicentre study found that survival in mechanically ventilated adult patients depended not only on patient-related factors but also on factors related to patient management and the development of complications [32]: successful noninvasive ventilation significantly reduced the risk of death (odds ratio 0.46).
A relationship between nursing workload and deteriorating ICU performance [3, 33] has been demonstrated in several studies. Nurses who are assigned a higher workload have less time for routine activities, and hygienic tasks often suffer under these conditions. A reduction in nursing staff to below critical levels is associated with an increased number of bloodstream infections from CVL [34]. Moreover, reduced nurse staffing is also associated with increased rates of pneumonia and septicaemia [3, 4, 5].
Although univariate analysis of our data showed work utilization ratio and occupancy rate to be significantly different between groups (and highest in group C), none of these parameters reached statistical significance in the multivariate analysis. There are several possible explanations for this: on one hand, our results could provide evidence that the inherent risk of the invasive procedures under study is more important than the increased nursing workload. On the other hand, it is very likely that the number of observations in the ICU-based linear regression analysis (n=18) was just too small to detect existing differences.
The question arises as to whether the increased severity-adjusted mortality in group C could be an artefact. SAPS II has been shown to lack prognostic accuracy when applied to populations other than the one from which it was derived [35, 36]. We have shown, however, that medical reasons for admission have a higher severity-adjusted mortality than surgical reasons for admission [18]. In our study, group B ICUs had a much higher incidence of medical admissions than did group C (Table 1). If case-mix differences influenced our O/E ratios, we would expect group B to have a higher severity-adjusted mortality than group C. Our data show exactly the opposite, which renders our results even more reliable.
In addition, multivariate analysis allowed us to adjust for a majority of what constitutes case mix: we were able to rule out the influence of age, gender, severity of illness at admission and reason for admission. We can therefore virtually exclude the possibility that our results were influenced by differences in case mix of patients between the three groups. Of course, we cannot fully exclude the possibility that other confounding variables might have influenced the difference in O/E ratios between groups. Nevertheless, it is important that the (patient-based) association between interventions and outcome remained highly significant throughout all analyses. Our results thus provide strong evidence that this association was at least partly responsible for the increased risk-adjusted mortality in group C patients.
What can we learn from these findings? They can be viewed from both an individual and an epidemiological perspective. In an attempt to achieve the best outcome for their patients (individual perspective), physicians will often use a strategy to reduce the “maximum risk” as far as possible and therefore use available resources to whatever extent they think is necessary. In large hospitals, more resources are available and (until now) fewer restrictions have been applied, especially in the care of critically ill patients. As our results suggest (epidemiological perspective), such a strategy might, however, increase the “average risk” and thus there might be a level of invasive treatment beyond which the associated risks outweigh the benefits. We acknowledge, of course, that in everyday practice it is difficult to apply such statistically derived results to an individual patient. Nevertheless, when decisions about invasive treatments are to be made, intensivists should always consider both the possible benefits associated with an intervention and the associated risks. Although our results cannot be used to answer the question, “How much treatment is optimal?,” they should encourage practising intensivists to carefully consider the issues we have raised.
References
Miranda DR, Ryan DW, Schaufeli WB, Fidler V (eds) (1998) Organization and management of intensive care. In: Vincent JL (ed) Update in intensive care medicine, vol 29. Springer, Berlin Heidelberg New York
Bastos PG, Knaus WA, Zimmerman JE, Magalhaes A Jr, Sun X, Wagner DP (1996) The importance of technology for achieving superior outcomes from intensive care. Brazil APACHE III Study Group. Intensive Care Med 22:664–669
Amaravadi RK, Dimick JB, Pronovost PJ, Lipsett PA (2000) ICU nurse to patient ratio is associated with complications and resource use after esophagectomy. Intensive Care Med 26:1857–1862
Pronovost PJ, Jenckes MW, Dorman T, Garrett E, Breslow MJ, Rosenfeld BA, Lipsett PA, Bass E (1999) Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. J Am Med Assoc 281:1310–1317
Pronovost PJ, Dang D, Dorman T, Lipsett PA, Garrett E, Jenckes M, Bass EB (2001) Intensive care unit nurse staffing and the risk for complications after abdominal aortic surgery. Eff Clin Pract 4:199–206
Dimick JB, Swoboda S, Pronovost PJ Lipsett PA (2001) Effect of nurse-to-patient ratio in the intensive care unit on pulmonary complications and resource use after hepatectomy. Am J Crit Care 10:376–382
Tucker J for the UK neonatal staffing study group (2002) Patient volume, staffing, and workload in relation to risk-adjusted outcomes in a random stratified sample of UK neonatal intensive care units: a prospective evaluation. Lancet 359:99–107
Metnitz PGH, Vesely H, Valentin A, Popow C, Hiesmayr M, Lenz K, Krenn CG, Steltzer H (1999) Evaluation of an interdisciplinary data set for national ICU assessment. Crit Care Med 27:1486–1491
ASDI. http://www.asdi.ac.at
Metnitz PGH, Steltzer H, Popow C, Valentin A, Lenz K, Neumark J, Sagmüller G, Schwameis F, Urschitz M, Hiesmayr M (1997) Definition and evaluation of a documentation standard for intensive care medicine: the ASDI pilot project. Wien Klin Wochenschr 109:132–138
Le Gall JR, Lemeshow St, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. J Am Med Assoc 270:2957–2963
Le Gall JR, Klar J, Lemeshow S, Saulnier F, Alberti C, Artigas A, Teres D. (1996) The logistic organ dysfunction system. A new way to assess organ dysfunction in the intensive care unit. J Am Med Assoc 276:802–810
Miranda DR, De Rijk A, Schaufeli W (1996) Simplified therapeutic interventions scoring system: the TISS-28 items—results from a multicenter study. Crit Care Med 4:64–73
Moreno R, Miranda DR (1998) Nursing staff in intensive care in Europe. The mismatch between planning and practice. Chest 113:752–758
Ridley S, Rowan K (1997) Be wary of occupancy figures. Health Trends 29:100–105
Metnitz PGH, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, Le Gall JR, Druml W (2002) Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med 30:2051–2058
Hosmer DW, Lemeshow S (1995) Confidence interval estimates of an index of quality performance based on logistic regression models. Stat Med 14:2161–2172
Metnitz PGH, Vesely H, Valentin A, Lang T, Le Gall JR (2000) Ratios of observed to expected mortality are affected by differences in case mix and quality of care. Intensive Care Med 26:1466–1472
Latto IP, Shang Ng W, Jones PL, Jenkins B (2000) Percutaneous central venous and arterial catheterisation, 3rd edn. Saunders, Philadelphia
Polderman KH, Girbes ARJ (2002) Central venous catheter use. Part 1: Mechanical complications. Intensive Care Med 28:1–17
Polderman KH, Girbes ARJ (2002) Central venous catheter use. Part 2: Infectious complications. Intensive Care Med 28:18–28
Charalambous C, Swoboda S, Dick J, Perl T, Lipsett P (1998) Risk factors and clinical impact of central line infections in the surgical intensive care unit. Arch Surg 133:1241–1246
Pittet D, Tarara D, Wenzel RP (1994) Nosocomial bloodstream infection in critically ill patients. Excess length of stay, extra costs, and attributable mortality. J Am Med Assoc 271:1598–1601
Connors AF Jr, Speroff T, Dawson NV, Thomas C, Harrell FE Jr, Wagner D, Desbiens N, Goldman L, Wu AW, Califf RM, Fulkerson WJ Jr, Vidaillet H, Broste S, Bellamy P, Lynn J, Knaus WA (1996) The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. J Am Med Assoc 276:889–897
Vieillard-Baron A, Girou E, Valente E, Brun-Buisson C, Jardin F, Lemaire F, Brochard L (2000) Predictors of mortality in acute respiratory distress syndrome. Focus on the role of right heart catheterization. Am J Respir Crit Care Med 161:1597–1601
Bernard GR, Sopko G, Cerra F et al. (2000) Pulmonary artery catheterization and clinical outcomes: National Heart, Lung, and Blood Institute and Food and Drug Administration workshop report. Consensus Statement. J Am Med Assoc 283:2568–2572
Druml W (1999) Metabolic aspects of continuous renal replacement therapies. Review. Kidney Int Suppl 72:S56–S61
Metnitz PGH, Fischer M, Bartens C, Steltzer H, Lang T, Druml W (2000) Impact of acute renal failure on antioxidant status in multiple organ failure. Acta Scand Anaesth 44:236–240
Cohen G, Haag-Weber M, Hörl WH (1997) Immune dysfunction in uremia. Kidney Int Suppl 62:79–82
Humay RD (2002) Statement of the 4th International Consensus Conference in Critical Care on ICU-Acquired Pneumonia, Chicago, Illinois. Intensive Care Med 28:1521–1536
Rello J, Paiva JA, Baraibar J, Barcenilla F, Bodi M, Castander D, Correa H, Diaz E, Garnacho J, Llorio M, Rios M, Rodriguez A, Sole-Violan J (2001) International conference for the development of consensus on the diagnosis and treatment of ventilator-associated pneumonia. Chest 120:955–970
Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, Benito S, Epstein SK, Apezteguia C, Nightingale P, Arroliga AC, Tobin MJ (2002) Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. J Am Med Assoc 287:345–355
Tarnow-Mordi WO, Hau C, Warden A, Shearer AJ (2000) Hospital mortality in relation to staff workload: a 4-year study in adult intensive-care unit. Lancet 356:185–189
Fridkin SK, Pear SM, Williamson TH, Galgiani JN, Jarvis WR (1996) The role of understaffing in central venous catheter-associated bloodstream infections. Infect Control Hosp Epidemiol 17:150–158
Moreno R, Apolone G, Reis Miranda D (1998) Evaluation of the uniformity of fit of general outcome prediction models Intensive Care Med 24:40–47
Metnitz PGH, Valentin A, Vesely H, Alberti C, Lang T, Lenz K, Steltzer H, Hiesmayr M (1999) Prognostic performance and customization of the SAPS II: results of a multicenter Austrian study. Intensive Care Med 25:192–197
Acknowledgements
We thank P. Bauer, Chairman of the Department of Medical Statistics, University of Vienna, Vienna, Austria, for his invaluable help. We thank furthermore the members of the ASDI study group and their respective study coordinators in each ICU.
Author information
Authors and Affiliations
Corresponding author
Additional information
An editorial regarding this article can be found in the same issue (http://dx.doi.org/10.1007/s00134-004-2202-z)
Rights and permissions
About this article
Cite this article
Metnitz, P.G.H., Reiter, A., Jordan, B. et al. More interventions do not necessarily improve outcome in critically ill patients. Intensive Care Med 30, 1586–1593 (2004). https://doi.org/10.1007/s00134-003-2154-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2154-8