Abstract
Background
Intensivists play an essential role in improving the outcomes of critically ill patients in intensive care units (ICUs). The transition of ICU physician staffing from low-intensity ICUs (elective intensivist or no intensivist consultation) to high-intensity ICUs (mandatory intensivist consultation or a closed ICU) improves clinical outcomes. However, whether a transition from high-intensity to low-intensity ICU staffing affects ICU outcomes and quality of care remains unknown.
Methods
A retrospective observational study was conducted to examine the impact of high- versus low-intensity staffing models on all-cause mortality in a suburban secondary community hospital with 400 general beds and 8 ICU beds. The ICU was switched from a high-intensity staffing model (high-former period) to low-intensity staffing in July 2019 (low-mid period) and then back to high-intensity staffing in March 2020 (high-latter period). Patients admitted from the emergency department, general ward, or operating room after emergency surgery were enrolled in these three periods and compared, balancing the predicted mortality and covariates of the patients. The primary outcome was all-cause mortality analyzed using hazard ratios (HRs) from Cox proportional hazards regression. An interrupted time-series analysis (ITSA) was also conducted to evaluate the effects of events (level change) and time.
Results
There were 962 eligible admissions, of which 251, 213, and 498 occurred in the high-former, low-mid, and high-latter periods, respectively. In the matched group (n = 600), the all-cause mortality rate comparing the high-former period with the low-mid period showed an HR of 0.88 [95% confidence interval (CI), 0.56, 1.39; p = 0.58] and that comparing the high-latter period with the low-mid period showed an HR of 0.84 [95% CI, 0.54, 1.30; p = 0.43]. The result for comparison between the three periods was p = 0.80. ITSA showed level changes of 4.05% [95% CI, -13.1, 21.2; p = 0.63] when ICU staffing changed from the high-former to the low-mid period and 1.35% [95% CI, -13.8, 16.5; p = 0.86] when ICU staffing changed from the low-mid to the high-latter period.
Conclusion
There was no statistically significant difference in all-cause mortality among the three ICU staffing periods. This study suggests that low-intensity ICU staffing might not worsen clinical outcomes in the ICU in a medium-sized community hospital. Multiple factors, including the presence of an intensivist, other medical staff, and practical guidelines, influence the prognosis of critically ill patients.
Similar content being viewed by others
Introduction
Intensivists play an essential role in managing intensive care units (ICUs) and delivering high-quality intensive care. High-intensity intensivist staffing improves the quality of critical care and contributes to better clinical outcomes in terms of mortality, duration of mechanical ventilation, and length of ICU stay (LOS) [1, 2]. According to the Society of Critical Care Medicine's guidelines for ICU admission, discharge, and triage in the United States [3] and the Leapfrog standards for critical care [4], ICUs should be staffed by intensivists who can coordinate and manage the care of critically ill patients. Further, ICU facility standards require the presence of a doctor who primarily works in the ICU.
Although the crucial functions of intensivists are widely recognized, there are not sufficient qualified intensivists to staff all ICUs in Japan [5]. At Otsu City Hospital, ICU physicians had comprised board-certified intensivist(s) for more than a decade; however, there was a temporary change in ICU physician staffing over the past few years. It was unclear whether the prognosis and quality of intensive care would decrease or remain unchanged once intensivists were absent in ICU management. It is impossible to directly compare the two situations of ICU management with and without intensivists using randomized controlled trials because random assignment of patients to the care of either intensivists or in-hospital physicians from other specialties is neither practical nor ethical [2]. To overcome this difficulty, our study combined matching to balance covariates [6] and an interrupted time-series analysis (ITSA) [7] to evaluate the clinical effect of transitioning between high-intensity and low-intensity staffing on mortality.
Methods
Ethical approval and consent to participate
This study was approved by the ethics committee of Otsu City Hospital (approval number 23; approval date, June 18, 2020). This study was conducted under the Declaration of Helsinki as a statement of ethical principles for medical research developed by the World Medical Association and STROBE reporting guidelines. The need for informed consent was waived by the ethics committee of Otsu City Hospital due to the retrospective nature of the study.
Data
The patients were admitted to the ICU from the emergency department, general ward, or operating room after emergency surgery. Exclusion criteria were patients under 16 years of age and patients with missing data. The study period was from November 1, 2018 to September 30, 2021. Otsu City Hospital, which has approximately 400 available beds and 8 ICU beds (6 ICU beds until October 2018), is a secondary hospital that offers emergency care to patients who may require hospitalization and provides intensive care for cases of acute coronary syndrome, stroke, and sepsis. It serves a population of approximately 340,000 people and manages 12,000 emergency room visits and 4,000 emergency transports every year. The study design considered the before–after setting because it investigated a policy change or transition at a given time point [1,2,3, 8,9,10]. Three periods were defined for comparison: 1) high-former, which indicated high-intensity ICU staffing with full-time board-certified intensivist(s) from November 1, 2018 to June 30, 2019; 2) low-mid, which indicated low-intensity ICU staffing without any full-time board-certified intensivists from July 1, 2019 to March 31, 2020; and 3) high-latter, which indicated high-intensity ICU staffing with full-time board-certified intensivist(s) from April 1, 2020 to September 30, 2021. Seven or eight physicians staffed the ICU department in the high-former period; two or three physicians, including intensivists, exclusively staffed the ICU and managed a high-intensity ICU, which included mandatory intensivist consultation [1], or a closed ICU. Two intensivists were staffed until January 2019, after which one intensivist was staffed. Physicians dedicated to the ICU were the responsible physicians for ICU patients during the day-time. During the nighttime, one of them or full-time in-house specialists in other fields were on duty. In the low-mid period, two physicians who were board-certified specialists in other fields managed the ICU along with full-time or part-time doctors, and the ICU continued to offer 24/7 care. During this period, there were no full-time intensivists available, and thus the unit functioned as an open ICU, so this term was categorized as low-intensity ICU staffing [1]. A new intensivist arrived on April 1, 2020 and became a new member of the ICU. Four physicians, including newly hired intensivists with several part-time intensivists, restarted high-intensity ICU staffing; this period was defined as high-latter (Table 1).
Statistical analyses
Matching based on the Acute Physiology and Chronic Health Evaluation (APACHE) II score was used to balance covariates prior to survival analysis. APACHE II and its related clinical values were collected from electronic health records within the first 24 h of ICU admission [11]. The collected values and data to be analyzed included age, sex, white blood cell count (103/mm3), hematocrit (%), Na+ level (mmol/L), K+ level (mmol/L), creatinine level (mg/dL), pH, partial pressure of arterial oxygen (mmHg), mean arterial pressure (mmHg), heart rate (beats per minute), respiratory rate (breaths per minute), body temperature (℃), and Glasgow Coma Scale score. To convert the APACHE II score to quantitative prognostic probability, additional information was collected, such as the requirement for emergency surgery, the reasons for ICU admission, and APACHE II diagnostic category weight according to the principal reason for ICU admission for calculating the predicted mortality (Supplementary information). Cases with no missing data were eligible for the analysis. The conventional paired matching was no longer applicable because there were multiple treatment groups [12,13,14]. The low-mid period was determined as the reference group, and the high-former vs. low-mid matching was done first. Then, matched samples in the low-mid (reference) were extracted and fixed. Next, the high-latter vs. low-mid matching was conducted. The samples in the high-former and high-latter periods matched with the same sample in the low-mid period were combined into a trio. Matchings were performed at a 1:1 ratio using 0.2 calipers without replacement to minimize the number of biased variables using the Match function in the Matching package in R [15].
ITSA was conducted to consider time trends [7]. An original ITSA focused on a segmented regression, presented as:
where \({Y}_{t}\) is the outcome at a given time point \(t\), \(I\left(t\right)=\left\{\begin{array}{cc}0& \textrm{if}\ t\le {t}_{0}\\ 1& \textrm{otherwise}\end{array}\right.\) is the event variable, \(T\left(t\right)=\left\{\begin{array}{cc}0& \textrm{if}\ t\le {t}_{0}\\ t-{t}_{0}& \textrm{otherwise}\end{array}\right.\) is the indicator of elapsed time from the event, \({t}_{0}\) is the time of the event, \({\epsilon }_{t}\) is an error term, and \(\beta\) s are regression coefficients. A segmented regression estimates \({\beta }_{2}\) (step or level change) and \({\beta }_{3}\) (slope or trend change) to evaluate the impact of the event. Schaffer et al. recommended the adaptation of the autoregressive integrated moving average (ARIMA) model to ITSA because the linear regression model assumed that the error terms were independent and not correlated between each data point, but longitudinal time series data typically exhibited features of non-stationarity, autocorrelation, and seasonality [16]. The set of parameters of the ARIMA model was determined by the auto.arima function in the forecast package in R [17] based on minimizing the Akaike or Bayesian information criterion [16]. The interest of analysis was the 30-day survival rate of covariate-balanced patients who were admitted to the ICU grouped by month, and the unit of time point for ITSA was months. Regression was performed using the lm_robust function in the estimatr package in R [18], accounting for heteroscedasticity based on the HC3 heteroscedasticity consistent covariance matrix [19, 20]. Heteroscedasticity was tested by the Breusch-Pagen test.
The primary outcome was all-cause mortality from the day of ICU admission. The secondary outcomes were the numbers of ICU and hospital deaths, the lengths of ICU and hospital stays, all-cause mortality stratified by APACHE II score-based predicted mortality according to the severity with a threshold of ≤ 30%, and level and trend changes estimated via ITSA. All-cause mortality was analyzed using the Cox proportional hazards model. Continuous data were expressed as the mean ± standard deviation, and categorical data were expressed as numbers (percentages). The analysis of variance for unmatched samples, and Friedman test for matched samples were used for continuous values and chi-squared test was used for categorical data. A p-value of < 0.05 was considered significant. Probabilistic uncertainty was represented using confidence intervals (CIs). Statistical analyses were performed using the R programming language and software (version 3.6.2).
Results
Baseline characteristics and matching
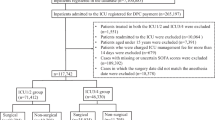
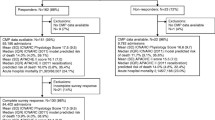
This study considered 987 admitted patients, among which 263 were enrolled in the high-former period, 214 were enrolled in the low-mid period, and 510 were enrolled in the high-latter period. Of these, 251, 213, and 498 patients in the high-former, low-mid, and high-latter periods, respectively, had complete data and were eligible for the outcome analysis (Fig. 1). The patients' mean age was 72.1 ± 16.1 years, 36.4% were > 80 years of age, and 57.5% were men. Patients admitted in the low-mid period had higher APACHE II scores and predicted mortality. The matching procedure matched 600 patients. Table 2 shows the baseline characteristics of the admissions and the parameters associated with the APACHE II-predicted mortality among the three periods before and after matching. All data were adequately balanced after matching.
Primary outcomes
The Cox proportional hazard model of the comparison between the high-former and low-mid periods showed a hazard ratio (HR) of 0.84 [95% CI, 0.58, 1.21; p = 0.35], and that between the high-latter and low-mid periods showed an HR of 0.94 [95% CI, 0.67, 1.32; p = 0.73]. The result of the comparison of the primary outcome between the three periods before matching was p = 0.63 (Fig. 2a). Among the matched groups, the result of the comparison between the high-former and low-mid periods showed an HR of 0.88 [95% CI, 0.56, 1.39; p = 0.58], and that between the high-latter and low-mid periods showed an HR of 0.84 [95% CI, 0.54, 1.30; p = 0.43]. The result of the comparison of the primary outcome among the three periods was p = 0.80 (Fig. 2b).
Secondary outcomes
The numbers of ICU deaths among the high-former, low-mid, and high-latter periods were 12 (4.78%), 10 (4.69%), and 18 (3.61%) (p = 0.68) before matching and 10 (5.00%), 9 (4.50%), and 5 (2.50%) (p = 0.40) after matching. The numbers of hospital deaths among the high-former, low-mid, and high-latter periods were 54 (21.5%), 40 (18.8%), and 89 (17.9%) (p = 0.49) before matching and 49 (24.5%), 35 (17.5%), and 35 (17.5%) (p = 0.13) after matching (Table 3). The LOSs among the high-former, low-mid, and high-latter periods were 3.18 days, 3.88 days, and 3.52 days (p = 0.09) before matching and 3.47 days, 3.88 days, and 3.30 days (p = 0.17) after matching. The lengths of hospital stay among the high-former, low-mid, and high-latter periods were 30.5 days, 34.0 days, and 32.2 days (p = 0.51) before matching and 32.7 days, 33.7 days, and 32.8 days (p = 0.39) after matching (Table 3).
For the secondary outcomes of the subpopulation stratified by APACHE II score-based predicted mortality according to the severity with a threshold of ≤ 30%, the all-cause mortality rates of less severe patients showed an HR of 0.95 [95% CI, 0.51, 1.77; p = 0.86] between the high-former and low-mid periods and an HR of 1.51 [95% CI, 0.85, 2.71; p = 0.16] between the high-latter and low-mid periods. The all-cause mortality rates of severe patients showed an HR of 0.79 [95% CI, 0.49, 1.28; p = 0.34] between the high-former and low-mid periods and an HR of 0.69 [95% CI, 0.46, 1.05; p = 0.09] between the high-latter and low-mid periods (Table 4). The comparison among the three periods showed p = 0.18 for less severe patients and p = 0.23 for severe patients before matching (Fig. 3a). After matching, the all-cause mortality rates of less severe patients showed an HR of 1.22 [95% CI, 0.65, 2.30; p = 0.53] between the high-former and low-mid periods and an HR of 1.22 [95% CI, 0.60, 2.45; p = 0.58] between the high-latter and low-mid periods. The all-cause mortality rates of severe patients showed an HR of 0.87 [95% CI, 0.52, 1.45; p = 0.60] between the high-former and low-mid periods and an HR of 0.70 [95% CI, 0.39, 1.23; p = 0.21] between the high-latter and low-mid periods (Table 4). The comparison among the three periods showed p = 0.79 for less severe patients and p = 0.45 for severe patients (Fig. 3b).
The survival rate stratified by the severity of predicted mortality according to Acute Physiology and Chronic Health Evaluation (APACHE) II scores. Patients are divided into non-severe (predicted mortality ≤ 30%) and severe (predicted mortality > 30%) cases. Survival curves are drawn for data (a) before matching and (b) after matching
The ARIMA model was determined as \(\left(p, d, q\right)=(0, 0, 0),\) indicating that the autocorrelation order of the model (p), the moving average order of the model (q), and the time series difference (d) were 0, and no seasonality was appropriately fitted. The result of the Breusch-Pagan test for heteroscedasticity was p = 0.08. At the transition from the high-former period to the low-mid period, ITSA showed a level change of 4.05% [95% CI, -13.1, 21.2; p = 0.63] and a trend change of -0.94%/month [95% CI, -2.80, 0.92; p = 0.31]. At the transition from the low-mid period to the high-latter period, ITSA showed a level change of 1.35% [95% CI, -13.8, 16.5; p = 0.86] and a trend change of 0.05%/month [95% CI, -0.78, 0.89; p = 0.89] (Fig. 4 and Table 5).
Interrupted time-series analysis (ITSA) of the effect of the transition of ICU staffing. Thirty-day survival rates (square dots) with 95% prediction intervals (vertical error bars) are shown. At the transition from the high-former period to the low-mid period, ITSA shows a level change of 4.05% [95% CI, -13.1, 21.2; p = 0.63] and a trend change of -0.94%/month [95% CI, -2.80, 0.92; p = 0.31]. At the transition from the low-mid period to the high-latter period, ITSA shows a level change of 1.35% [95% CI, -13.8, 16.5; p = 0.86] and a trend change of 0.05%/month [95% CI, -0.78, 0.89; p = 0.89] for the 30-day survival rate. ITSA, interrupted time-series analysis; ICU, intensive care unit; CI, confidence interval
Discussion
When ICU staffing transitions from low intensity to high intensity, there are significant improvements in outcomes [1, 2] in medical [21], surgical [10, 22], and specialized (cardiovascular [9, 23, 24], neurological [25,26,27], and pediatric [28]) ICUs. The Leapfrog Group's ICU Physician Staffing Safety Standards recommend high-intensity staffing [4] based on the results of prior studies [21,22,23, 29]. Despite such compelling evidence, cost barriers or a lack of available expertise prevents hospitals from employing full-time intensivists [30]; only 47% of hospitals in the United States met this standard in a 2015 survey [31]. Consequently, other specialists or hospitalists are forced to care for ICU patients [32]. Some studies have clarified that ICU management does not improve mortality rates [8, 9, 29, 32] and that its effectiveness is controversial, whereas some guidelines recommend placing intensivists in the ICU [3, 4]. Conversely, it is intuitively easy to imagine that an absence of intensivists may reduce ICU management quality. However, our study showed that the transitions from high-intensity to low-intensity ICU staffing and from low-intensity to high-intensity ICU staffing did not significantly change clinical outcomes for all-cause mortality. This might have occurred due to the following reasons. First, even during the low-mid period, at least one well-trained full-time or part-time physician from another field was staffed to enable continuous ICU staffing (the 24/7 staffing model). In addition to implementing the 24/7 staffing model of ICU physicians, multidisciplinary medical teams comprising nurses, pharmacologists, clinical engineers, physical therapists, and medical social workers contributed to ICU management throughout the study period. The remaining staff (i.e., the board-certified respiratory internist and the newly hired physician specializing in emergency medicine) consistently followed the ABCDEF bundle [33] – an evidence-based approach that targets critically ill patients [34] – during the low-mid period to optimize treatment for patients in the ICU by collaborating with multidisciplinary medical teams. Despite the downgrade of the staffing model, the increased adherence to clinical practice guidelines [2] and the presence of multidisciplinary teams in the ICU [35, 36] would have affected patient outcomes. Second, the impact of the presence of intensivists on mortality might not be as significant as expected in earlier studies [37]. Early studies that demonstrated a relationship between mortality reduction and intensivist staffing models were mostly from single-center and before–after analyses conducted in the 1990s or 2000s [1, 2]. Furthermore, ICU and hospital mortality rates varied by decade, decreasing in the 1980s and 2000s but not in the 1990s or 2010s [2]. Recent multicenter analyses showed no significant association between high-intensity ICU staffing and mortality [38, 39]. These studies suggest that the relationship between intensivist staffing and patient mortality is weaker than previously thought. Third, the transition in intensivist staffing probably has only a limited impact on mortality in small- and medium-volume hospitals. A closed ICU implementing a 24/7 ICU intensivist staffing model in an academic hospital reduced LOS and generated significant cost savings [40]. Furthermore, a recent study revealed that the presence of 24/7 in-house ICU intensivists positively affects the quality of care for critically ill patients in high-acuity, high-volume centers; however, the benefits could not be sufficiently extrapolated to low-acuity, low-volume hospitals to justify the increase in staffing needs and costs [41]. In our study, 24/7 staffing with trained physicians and multidisciplinary medical teams played an essential role in maintaining the quality of intensive care in a relatively small community hospital. Lastly, the statistical power was too small to detect any significant increase or decrease in mortality due to the small mortality effect size. A study that demonstrated an improvement in the 28-day mortality of oncology patients in an ICU implementing a high-intensity staffing model reduced the mortality rate from 47.69% to 29.84% [42]. Since oncology patients are more severely ill (median APACHE II score, 20) than the general ICU patient population, there is room to improve mortality rates. However, it is difficult to significantly reduce the mortality rate in such a low-mortality population [9]. Since our study's participants had lower ICU and hospital mortality in any period than those seen in the Japanese database (6.3% ICU mortality for critically ill adults [43]), it had low statistical power due to the small effect size.
The importance of employing intensivists in ICUs and healthcare systems is widely recognized [44]. Furthermore, the importance of employing full-time ICU physicians is highlighted in Japan [45, 46]. However, the implementation of high-quality ICU management remains inadequate, even in developed countries. In the United States, 53% of ICUs did not meet Leapfrog's standard according to a 2015 survey [31]. In Canada, 85% of ICUs could not satisfy the professional standards of practice recommended by the relevant guidelines, and 49% of them did not have dedicated in-house ICU physicians according to a 2006 survey [47]. Lastly, only 39% of ICUs in Japan employed board-certified intensivists according to a 2008 survey [36]. Intensivists are a rare resource, and the feasibility of broad-based expansion of ICU staffing will take time. Increased adherence to clinical practice guidelines [2] and the presence of multidisciplinary teams in the ICU [35, 36] would positively impact patient outcomes.
This study had some limitations. First, the APACHE II score-based matching analysis did not necessarily control group bias. Second, this study used a single-center, before–after setting. Since before–after analyses suffer from secular trends [2, 8], our results cannot be simply generalized and extrapolated to other settings. Third, due to the unavailability of data, we did not account for other clinical outcomes that could have realized intensivists' maximum potential, such as the duration of mechanical ventilation, the optimization of sedation, and cost-effective management. A significant difference might have occurred in these surrogate clinical indicators.
Conclusions
All-cause mortality did not significantly change with the transition from 24/7 high-intensity ICU staffing with board-certified intensivist(s) to 24/7 low-intensity ICU staffing without the board-certified staff and then back to high-intensity ICU staffing. Our results indicated that the existence of intensivists is not the sole factor influencing clinical outcomes in the ICU and that intensivists play a vital role in intensivist-led ICU rounds to treat critically ill patients by collaborating with intra-hospital physicians and multidisciplinary medical teams.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ICU:
-
Intensive care unit
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- LOS:
-
Length of ICU stay
- ITSA:
-
Interrupted time-series analysis
- ARIMA:
-
Autoregressive integrated moving average
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
References
Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288(17):2151–62.
Wilcox ME, Chong CAKY, Niven DJ, Rubenfeld GD, Rowan KM, Wunsch H, et al. Do intensivist staffing patterns influence hospital mortality following ICU admission? A systematic review and meta-analyses. Crit Care Med. 2013;41(10):2253–74.
Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU Admission, Discharge, and Triage Guidelines: A Framework to Enhance Clinical Operations, Development of Institutional Policies, and Further Research. Crit Care Med. 2016;44(8):1553–602.
Manthous CA. Leapfrog and critical care: evidence- and reality-based intensive care for the 21st century. Am J Med. 2004;116(3):188–93.
Shime N. Clinical and investigative critical care medicine in Japan. Intensive Care Med. 2016;42(3):453–5.
Rosenbaum PR. Multivariate Matching Methods. In: Balakrishnan N, Colton T, Everitt B, Piegorsch W, Ruggeri F, Teugels JL, editors. Wiley StatsRef: Statistics Reference Online. 1st ed. Wiley; 2015. p. 1–6. Available from: https://doi.org/10.1002/9781118445112.stat02440.pub2. [Cited 2022 Aug 7].
Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;9(350):h2750.
Nagendran M, Dimick JB, Gonzalez AA, Birkmeyer JD, Ghaferi AA. Mortality Among Older Adults Before Versus After Hospital Transition to Intensivist Staffing. Med Care. 2016;54(1):67–73.
Kim DJ, Sohn B, Kim H, Chang HW, Lee JH, Kim JS, et al. The Impact of an Attending Intensivist on the Clinical Outcomes of Patients Admitted to the Cardiac Surgical Intensive Care Unit after Coronary Artery Bypass Grafting. Korean J Thorac Cardiovasc Surg. 2020;53(1):8–15.
Park CM, Chun HK, Lee DS, Jeon K, Suh GY, Jeong JC. Impact of a surgical intensivist on the clinical outcomes of patients admitted to a surgical intensive care unit. Ann Surg Treat Res. 2014;86(6):319–24.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Zhao QY, Luo JC, Su Y, Zhang YJ, Tu GW, Luo Z. Propensity score matching with R: conventional methods and new features. Ann Transl Med. 2021;9(9):812.
Solomon DH, Rassen JA, Glynn RJ, Garneau K, Levin R, Lee J, et al. The comparative safety of opioids for nonmalignant pain in older adults. Arch Intern Med. 2010;170(22):1979–86.
Solomon DH, Rassen JA, Glynn RJ, Lee J, Levin R, Schneeweiss S. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170(22):1968–76.
Sekhon JS. Multivariate and Propensity Score Matching Software with Automated Balance Optimization: The Matching Package for R. J Stat Softw. 2011;42(7). Available from: http://www.jstatsoft.org/v42/i07/. [Cited 2022 Aug 13].
Schaffer AL, Dobbins TA, Pearson S-A. Interrupted time series analysis using autoregressive integrated moving average (ARIMA) models: a guide for evaluating large-scale health interventions. BMC Med Res Methodol. 2021;21(1):58.
Hyndman RJ, Khandakar Y. Automatic Time Series Forecasting: The forecast Package for R. J Stat Softw. 2008;27(3). Available from: http://www.jstatsoft.org/v27/i03/. [Cited 2021 May 11].
Graeme B, Jasper C, Alexander C, Macartan H, Luke S. estimatr: Fast Estimators for Design-Based Inference. Available from: https://CRAN.R-project.org/package=estimatr. [Cited 2022 Sep 21].
Long JS, Ervin LH. Using Heteroscedasticity Consistent Standard Errors in the Linear Regression Model. Am Stat. 2000;54(3):217.
Hayes AF, Cai L. Using heteroskedasticity-consistent standard error estimators in OLS regression: An introduction and software implementation. Behav Res Methods. 2007;39(4):709–22.
Carson SS, Stocking C, Podsadecki T, Christenson J, Pohlman A, MacRae S, et al. Effects of organizational change in the medical intensive care unit of a teaching hospital: a comparison of “open” and “closed” formats. JAMA. 1996;276(4):322–8.
Ghorra S, Reinert SE, Cioffi W, Buczko G, Simms HH. Analysis of the effect of conversion from open to closed surgical intensive care unit. Ann Surg. 1999;229(2):163–71.
Pronovost PJ, Jenckes MW, Dorman T, Garrett E, Breslow MJ, Rosenfeld BA, et al. Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery. JAMA. 1999;281(14):1310–7.
Miller PE, Chouairi F, Thomas A, Kunitomo Y, Aslam F, Canavan ME, et al. Transition From an Open to Closed Staffing Model in the Cardiac Intensive Care Unit Improves Clinical Outcomes. J Am Heart Assoc. 2021;10(3):e018182.
Mirski MA, Chang CW, Cowan R. Impact of a neuroscience intensive care unit on neurosurgical patient outcomes and cost of care: evidence-based support for an intensivist-directed specialty ICU model of care. J Neurosurg Anesthesiol. 2001;13(2):83–92.
Suarez JI, Zaidat OO, Suri MF, Feen ES, Lynch G, Hickman J, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004;32(11):2311–7.
Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med. 2001;29(3):635–40.
Ueno Y, Imanaka H, Oto J, Nishimura M. Change in Ratio of Observed-to-Expected Deaths in Pediatric Patients after Implementing a Closed Policy in an Adult ICU That Admits Children. Crit Care Res Pract. 2012;2012:674262.
Multz AS, Chalfin DB, Samson IM, Dantzker DR, Fein AM, Steinberg HN, et al. A “closed” medical intensive care unit (MICU) improves resource utilization when compared with an “open” MICU. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1468–73.
Juneja D, Nasa P, Singh O. Physician staffing pattern in intensive care units: Have we cracked the code? World J Crit Care Med. 2012;1(1):10–4.
The Leapfrog Group. Intensive care unit physician staffing: data by hospital on nationally standardized metrics. 2016. Available from: http://www.leapfroggroup.org/sites/default/files/Files/Castlight-Leapfrog-ICU-Physician-Staffing-Report-2016.pdf. [Cited 2020 Nov 2].
Wise KR, Akopov VA, Williams BR, Ido MS, Leeper KV, Dressler DD. Hospitalists and intensivists in the medical ICU: a prospective observational study comparing mortality and length of stay between two staffing models. J Hosp Med. 2012;7(3):183–9.
Marra A, Ely EW, Pandharipande PP, Patel MB. The ABCDEF Bundle in Critical Care. Crit Care Clin. 2017;33(2):225–43.
Pun BT, Balas MC, Barnes-Daly MA, Thompson JL, Aldrich JM, Barr J, et al. Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15,000 Adults. Crit Care Med. 2019;47(1):3–14.
Kim MM, Barnato AE, Angus DC, Fleisher LA, Fleisher LF, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med. 2010;170(4):369–76.
Committee on ICU Evaluation, Japanese Society of Intensive Care Medicine, The Health Labour Science Research group for “DPC”, the Ministry of Health, Labour, and Welfare. Influence of staffing and administrative policy of ICU on patient outcome. J Jpn Soc Intensive Care Med. 2011;18(2):283–94.
Costa DK, Wallace DJ, Kahn JM. The Association Between Daytime Intensivist Physician Staffing and Mortality in the Context of Other ICU Organizational Practices: A Multicenter Cohort Study. Crit Care Med. 2015;43(11):2275–82.
Checkley W, Martin GS, Brown SM, Chang SY, Dabbagh O, Fremont RD, et al. Structure, process, and annual ICU mortality across 69 centers: United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study. Crit Care Med. 2014;42(2):344–56.
Yoo EJ, Edwards JD, Dean ML, Dudley RA. Multidisciplinary Critical Care and Intensivist Staffing: Results of a Statewide Survey and Association With Mortality. J Intensive Care Med. 2016;31(5):325–32.
Banerjee R, Naessens JM, Seferian EG, Gajic O, Moriarty JP, Johnson MG, et al. Economic implications of nighttime attending intensivist coverage in a medical intensive care unit. Crit Care Med. 2011;39(6):1257–62.
Masud F, Lam TYC, Fatima S. Is 24/7 In-House Intensivist Staffing Necessary in the Intensive Care Unit? Methodist DeBakey Cardiovasc J. 2018;14(2):134–40.
Hawari FI, Al Najjar TI, Zaru L, Al Fayoumee W, Salah SH, Mukhaimar MZ. The effect of implementing high-intensity intensive care unit staffing model on outcome of critically ill oncology patients. Crit Care Med. 2009;37(6):1967–71.
Irie H, Okamoto H, Uchino S, Endo H, Uchida M, Kawasaki T, et al. The Japanese Intensive care PAtient Database (JIPAD): A national intensive care unit registry in Japan. J Crit Care. 2020;55:86–94.
Pronovost PJ, Holzmueller CG, Clattenburg L, Berenholtz S, Martinez EA, Paz JR, et al. Team care: beyond open and closed intensive care units. Curr Opin Crit Care. 2006;12(6):604–8.
Inui D, Nakataki E, Yamaguchi H, Oto J, Imanaka H, Nishimura M. Effects of the change of intensive care unit policy on patient’s prognosis. J Jpn Soc Intensive Care Med. 2009;16(1):33–7.
Uchino S. Are Japanese ICUs properly utilized? J Jpn Soc Intensive Care Med. 2010;17(2):141–4.
Parshuram CS, Kirpalani H, Mehta S, Granton J, Cook D, Canadian Critical Care Trials Group. In-house, overnight physician staffing: a cross-sectional survey of Canadian adult and pediatric intensive care units. Crit Care Med. 2006;34(6):1674–8.
Acknowledgements
The authors would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by the branding program as a world-leading research university on intractable immune and allergic diseases and a grant awarded to KH from MEXT Japan.
Author information
Authors and Affiliations
Contributions
YF conceptualized the study. YF, and KM collected data and patients. YF, KH, KM, YM, KK, and MH drafted the manuscript. YF, KH, and YN revised the manuscript. YF analyzed the data. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the ethical committee of Otsu City Hospital (approval number 23; approval date, June 18, 2020). This study was conducted under the Declaration of Helsinki and STROBE reporting guidelines. The need for informed consent was waived by the ethics committee of Otsu City Hospital due to the retrospective nature of the study.
Consent for publication
Consent for publication was waived by the ethical committee of Otsu City Hospital due to the retrospective study.
Competing interests
The authors report that there are no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fujii, Y., Hirota, K., Muranishi, K. et al. Clinical impact of physician staffing transition in intensive care units: a retrospective observational study. BMC Anesthesiol 22, 362 (2022). https://doi.org/10.1186/s12871-022-01905-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01905-0