Abstract
Objective
To estimate the effect of artificial ventilation on regional cerebral blood flow, cardiovascular regulation, and cerebral oxidative metabolism in newborns.
Design and subjects
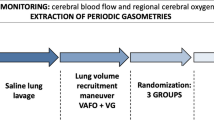
Comparison of three randomized treatment groups of newborn piglets: Group 1 (artificially ventilated sham-operated group; n =7); group 2 (artificially ventilated group with normoxia and moderate normocapnic hypoxia; n =7); group 3 (spontaneously breathing group with normoxia and moderate normocapnic hypoxia; n =6).
Measurements and results
Animals were anesthetized with 0.5% isoflurane in 70% nitrous oxide and 30% oxygen. Groups 1 and 2 were artificially ventilated. Animals in group 3 breathed spontaneously. Moderate normocapnic hypoxia was induced in groups 2 and 3 for 1 h by lowering the inspiratory oxygen fraction from 0.35 to 0.11. Mode of ventilation induced at most marginal effects on global cerebrovascular response, cardiovascular regulation, and cerebral oxidative metabolism. However, under normoxic conditions, regional cerebral blood flow of the medulla oblongata, pons, mesencephalon, thalamus, and cerebellum were markedly reduced in artificially ventilated piglets (P <0.05). Moderate normocapnic hypoxia led to a marked increase in regional cerebral blood flow, which was significantly lower in the medulla oblongata, pons, mesencephalon, thalamus, and cerebellum of artificially ventilated piglets (P <0.05).
Conclusion
Artificial ventilation clearly induces reduced neuronal activity in the brain stem and cerebellum of newborn piglets. This is suggested by a considerably reduced blood flow in these regions under normoxia and moderate normocapnic hypoxia. However, there is no relevant detrimental effect on cardiovascular regulation and brain oxidative metabolism.
Similar content being viewed by others
Introduction
The introduction of mechanical ventilation for the treatment of neonatal respiratory insufficiency has resulted in the successful treatment of many previously fatal diseases. Nevertheless, the use of mechanical ventilation in sick newborns was accompanied with some unfavorable secondary effects, in particular chronic lung injury or bronchopulmonary dysplasia. Furthermore, assisted ventilation alters systemic cardiovascular function through its effects on venous return and pulmonary vascular resistance. However, little is known about the effects of artificial ventilation itself on the function of other organs of newborns including the brain. This is surprising because it has previously been shown that preterm babies treated with mechanical ventilation exhibited reduced cerebral blood flow (CBF) [1]. In contrast, CBF-carbon dioxide reactivity increased during the first 48 h of life in artificially ventilated preterm infants with persistently normal brain sonograms [2]. However, the influence of artificial ventilation on regional cerebral blood flow of the various brain regions of newborns has not been systematically examined.
The influence of mechanical ventilation on specific brain functions is likely in regard to respiration-related brain structures, because of the inhibitory effects of the Hering-Breuer reflex and of reduced muscular reafferences to brainstem neurons [3]. Whether such inhibitory influences comprise a widespread reduction in brainstem activity remains unknown. Nevertheless, such functional inhibition could exacerbate weaning and extubation [4].
In order to elucidate possible regional cerebral alterations of mechanical ventilation, we examined the effects of positive pressure ventilation on regional cerebral blood flow and compared it with those of spontaneous breathing under normocapnic normoxia and hypoxia.
Materials and methods
This protocol was approved by the committee of the Thuringian State Government for Animal Research. Animals were obtained from a breeding farm. Immediately before the onset of the experiments, animals were moved to the laboratory in a climatized transport incubator.
Surgical procedures
Twenty newborn piglets (age 12 −36 h old; body weight 1,543±169 g) were anaesthetized initially with 1.5% isoflurane in 70% nitrous oxide and 30% oxygen. Cutaneous incisions were made after subcutaneous instillation of a local anesthetic (xylocitin 2%, Jenapharm, Jena, Germany). A central venous catheter was introduced through the left external jugular vein and used for the administration of drugs and for volume substitution (lactated Ringer’s solution: 5 ml kg−1 body weight h−1). An appropriate endotracheal tube was inserted through a tracheotomy. Fourteen randomly chosen animals were immobilized with pancuronium bromide (0.2 mg kg-1 body weight h−1, i.v.) and artificially ventilated (Servo Ventilator 900C, Siemens-Elema, Sweden). Volume-controlled ventilation was performed. Tidal volume and respiratory rate were adjusted to maintain end-tidal CO2 concentration near 5%. End-tidal CO2 was monitored by a CO2 analyzer (CO2 Analyzer 930, Siemens-Elema). A positive end-expiratory pressure of 2–4 mbar was used. Tidal volume (between 15 ml and 20 ml), respiratory rate (20–25 cycles per min), and inspiratory time fraction (25%) were titrated to maintain an arterial PCO2 of 35–40 mmHg. The peak airway pressure was usually between 12 mbar and 15 mbar. The remaining six animals breathed spontaneously throughout the experiment. Anesthesia was maintained throughout the surgical interventions with 0.5–0.8% isoflurane. A polyurethane catheter was advanced through an umbilical artery into the abdominal aorta to measure blood gases and pH, record arterial blood pressure, and withdraw reference blood samples for the colored microsphere method. For measurement of cardiac output by thermodilution, a thermocouple was inserted through the second umbilical artery into the abdominal aorta at the height of the diaphragm. The left ventricle was cannulized retrogradely via the right common carotid artery with a polyurethane catheter. A further polyurethane catheter was inserted into the superior sagittal sinus through a midline burr hole and advanced to the confluence of the sinuses in order to obtain brain venous blood samples. Rectal temperature was maintained throughout the experiment at 38 °C using a water-perfused heating pad and a feedback-controlled heating lamp.
Experimental protocol
After surgical preparation was completed, a 30-ml blood exchange was performed (intravenous infusion of heparinized blood obtained from a donor sibling piglet and withdrawal of the same amount from an arterial line, simultaneously) in order to replace blood volume throughout the experiment. Then, the isoflurane concentration was adjusted to 0.25% in 70% nitrous oxide and 30% oxygen and the piglets were allowed to rest for approximately 60 min.
After baseline values had been obtained, in seven randomly chosen artificially ventilated animals (group 2) and in the spontaneously breathing piglets (group 3) the inspired fraction of oxygen was reduced from 0.35 to ~ 0.11 in exchange for nitrogen in order to induce a moderate normocapnic hypoxemia. The remaining seven animals served as sham-operated normoxic control group (group 1). After 1 h gas mixture was re-established and the recovery was monitored for 30 min. At the end of baseline period (baseline), at the 15th minute (hypoxia 15’), and 50th minute of hypoxia (hypoxia 50’), as well as at the 30th minute of reoxygenation (recovery) arterial blood pressure and heart rate were measured, and then cerebral blood flows were estimated immediately followed by the withdrawal of arterial blood samples in order to estimate blood gases and electrolytes, pH, glucose, and lactate content. Subsequently, the same volume of donor blood was re-infused.
Analytical procedures and calculations
Blood pH, PCO2, and PO2 were determined with an ABL50 Blood Gas Analyzer (Radiometer, Copenhagen, Denmark). Blood hemoglobin content and oxygen saturation were determined using a Hemoximeter OSM2 (Radiometer). Glucose and lactate contents were determined with an electrolyte, metabolite laboratory EML105 (Radiometer). Regional CBF was measured by means of the reference sample color-labeled microsphere technique [5]. Application in piglets and methodical considerations have been presented and discussed in detail elsewhere [6, 7]. All reference and tissue samples contained >400 microspheres. Absolute flows to the tissues were calculated by the formula: flowtissue = number of microspherestissue · (flowreference / number of microspheresreference). The cerebrovascular resistance was calculated as the quotient of the mean arterial blood pressure and the regional brain blood flows. Because the sagittal sinus drains the cerebral cortex, the cerebral white matter, and some deep gray structures (basal ganglia, thalamus, and the hippocampus) [8], the blood flow to and from the cerebrum included these structures. Cerebral oxygen consumption was obtained by multiplying the blood flow to the cerebrum by the brain arteriovenous oxygen content difference. Cerebral oxygen extraction was calculated as the quotient of cerebral oxygen consumption and cerebral oxygen delivery. Cardiac output was measured by the thermodilution method (HZW BN 7206; August Fischer, Göttingen, Germany).
Statistical analysis
Data are reported as means±standard deviation. One-way analysis of variance was used to determine the effects of experimental procedure on physiological variables, and cerebral blood flows, parameters of brain oxidative metabolism between animal groups. Post hoc comparisons were made with the Tukey’s Test for all pairwise multiple comparisons. One-way repeated measures analysis of variance was used to prove effects within the groups studied in regard of baseline values. Differences were considered significant when P <0.05.
Results
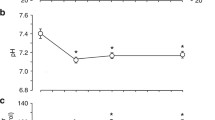
The results concerning the physiological variables are summarized in Table 1. During baseline conditions data were within the physiological range and consistent with other data obtained from anesthetized newborn piglets [9, 10]. During the hypoxemic period arterial O2 content was similarly reduced in groups 2 and 3 (P <0.05), whereas arterial lactate content was similarly increased (P <0.05 compared with controls) and remained elevated during the observed recovery period. However, systemic cardiovascular effects of moderate normocapnic hypoxia were different in relation to the mode of ventilation: artificially ventilated animals but not spontaneously breathing newborn piglets showed an increase in heart rate, which reached the level of significance (P <0.05). The latter, however, exhibited a marked increase in cardiac output during late hypoxia and at the early recovery period (P <0.05).
Mode of ventilation induced only marginal effects on global cerebrovascular response and cerebral oxidative metabolism during normoxic and hypoxic conditions. With the exception of the mildly reduced cerebrovascular resistance during normoxic baseline conditions in spontaneously breathing piglets (Table 2, P <0.05), there was similar behavior in global CBF and cerebrovascular resistance in groups 2 and 3. In addition, cerebral oxygen delivery and cerebral oxygen consumption were unchanged throughout this experiment in all groups studied. Cerebral oxygen extraction was reduced in spontaneously breathing piglets (Table 2, P <0.05). However, there was no change throughout the experiment under normoxic conditions (group 1) as well as during and after normocapnic hypoxia (groups 2 and 3).
Under normoxic conditions, regional CBF of the lower brainstem (medulla oblongata and pons, mesencephalon), thalamus and cerebellum was markedly higher in spontaneously breathing piglets (Fig. 1; P <0.05). In contrast, CBF of the cerebral cortex and the hippocampus was similar in all groups studied. Moderate normocapnic hypoxia led to a marked increase in regional CBF. This increase was significantly higher in the medulla oblongata, pons, and thalamus of spontaneous breathing animals during 15-min and 50-min hypoxia and in the mesencephalon and cerebellum during 50-min hypoxia. The highest absolute increase was in the medulla oblongata and pons (P <0.05). CBF of these regions remained elevated in spontaneously breathing animals during the early recovery, too (P <0.05). However, the percent changes from baseline in blood flow to all brain structures during normocapnic hypoxia did not differ between ventilated and spontaneously breathing animals.
1 Effect of moderate normocapnic hypoxia on regional cerebral blood flow (CBF) in artificially ventilated (open columns, group 2, n =7) and spontaneously breathing piglets (hatched columns, group 3, n =6). (Values are means±SD. * $ P <0.05; * indicates significant differences to the sham operated group (filled columns, group 1, n =7), $ indicates significant differences between groups 2 and 3)
Discussion
The main new finding in this study is that the blood flow of brainstem, cerebellum, and thalamus is markedly reduced in ventilated piglets compared with spontaneously breathing ones, whereas forebrain blood flow remained similar in both groups. Meanwhile, it has been clearly indicated that highly regulated metabolic interactions occur between neuronal (synaptic) activity and neuronal/astrocytic glucose utilization [11, 12], which in turn controls local cerebral blood flow [13]. A strong coupling between local cerebral energy metabolism and blood flow already exists in the neonatal brain [14]. Therefore, the reduction in the regional CBF of brainstem, cerebellum, and thalamus may indicate a reduced neuronal activity in these brain regions by artificial ventilation provided that the coupling between blood flow and metabolism remained intact. We determined cerebral oxygen extraction, (Table 2), which was unaltered throughout the experiment under normoxic conditions (group 1) as well as during and after normocapnic hypoxia (groups 2 and 3). Furthermore, cerebral oxygen consumption was preserved and constant, too. Therefore, there is evidence that coupling between blood flow and metabolism is preserved and constant during the experiment [15, 16, 17]. In addition, there was a significant increase in cerebral oxygen extraction of artificially ventilated newborn piglets during normoxic as well as hypoxic conditions by about 25 percent compared to spontaneously breathing ones (Table 2, P <0.05). Because cerebral oxygen consumption was quite similar under spontaneously breathing and artificial ventilation, capillary recruitment appears to be increased in consequence of artificial ventilation, which would lead to an increase in oxygen diffusion capacity and hence in cerebral oxygen extraction [18].
Reduced brainstem activity during artificial ventilation may be caused by diminished activation of respiratory-related neurons, considering that other afferents may also be markedly deprived by systemic muscular paralysis. Afferences from excited slowly adapting lung receptors appear to be responsible for inhibiting effects upon the inspiratory neurons [3]. The reduced proprioreceptive and metabolic reafferent activities from paralyzed respiratory and other muscles could also participate on reduced brainstem activation in consequence of their blunted activating effects within the common brainstem system [19]. On the other hand, it can be assumed that during mechanical ventilation under conditions with reduced or abolished lung compliance (e.g., in neonates with hyaline membrane disease or other pulmonary disorders), and therefore diminished inspiratory distension, the activity of slowly adapting lung receptors must be deprived. Consequently, a reduced afferent input should lessen inhibiting effects on inspiratory neurons and in turn metabolic demand should be augmented. Therefore, under such conditions an increase in brainstem CBF should be expected.
Furthermore, the presented findings suggest that the functional activity of thalamus and cerebellum is mainly influenced by their involvement in motor activity and its control. Even under resting conditions and mild sedation, regional blood flow of these regions was diminished by 36% to 41% after medical immobilization. In contrast, whole brain cortex and hippocampus showed only marginal alterations under such conditions. Brain cortex preparation was performed without any functional or cytoarchitectonic considerations. Therefore, we were unable to determine possible regional differences within the brain cortex.
Mild sedation by volatile anesthetics and analgesia by nitrous oxide used here appears to be adequate for the experimental approach of this study. Previous studies have been shown that there is no detectable influence on cardiovascular response in newborn piglets [20]. Furthermore, CBF and cerebral O2 uptake values presented in this study were similar to values obtained from newborn piglets which were treated with other drugs for general anesthesia which were indicated as not altering brain oxidative metabolism and from awake newborn piglets [21, 22]. CBF distribution throughout the immature brain with a gradient between brainstem (highest perfusion values) and forebrain (lowest perfusion values) confirms previous findings [23]. In addition, the used dosage of pancuronium bromide for muscular relaxation does not alter systemic hemodynamic status and CBF regulation in newborn piglets [24, 25]. On the other hand, there is evidence drawn from our own previous studies that newborn piglets studied under the conditions used were without relevant stressful consequences as shown on related cardiovascular or humoral parameters. In a previous study with extensive surgical preparations, including opening the abdominal cavity, craniotomy, ureter cannulization after retroperitoneal preparation, and up to 5-h experimental performance, sham-operated newborn piglets did not show significant difference in arterial blood pressure and only a slight increase in heart rate (by 20%) throughout the observational period. This corresponded with a comparatively moderate increase in circulating catecholamines (epinephrine: by 73%, norepinephrine: by 66%) [26]. This elevation in circulating catecholamines was markedly blunted compared with a rather mild hypoxic exposure. After 45 min of mild normocapnic hypoxia (art. oxygen saturation = 71±8%, art PO2 = 39±7 mmHg) we found a marked increase in circulating catecholamines (epinephrine: by 175%, norepinephrine: by 125%) [10]. Furthermore, during baseline conditions, data were within the physiological range, consistent with other data obtained from anesthetized newborn piglets [9, 10], and similar with data obtained from newborn non-anesthetized piglets [27].
Normocapnic hypoxia induced a marked overall CBF increase. This response is mainly caused by hypoxia-induced vasodilation. Underlying mechanisms are intensively studied even in the newborn piglet [28, 29, 30], but up to now the complex interaction of numerous vasoactive mediators involved remained unclear [31, 32]. Nevertheless, the final step of hypoxia-induced vasodilation is obviously caused by an opioid-related activation of ATP-sensitive potassium channels and a cAMP-related activation of calcium sensitive potassium channels [33, 34]. The resulting membrane hyperpolarization is responsible for a reduced intracellular calcium availability, which in turn caused the smooth muscle relaxation.
There was a proportional increase in regional CBF during moderate normocapnic hypoxia in spontaneously breathing and artificially ventilated piglets. Experimental performance does not allow us to distinguish between the effects of paralysis and ventilation as the consequence of reduced blood flow in artificially ventilated piglets. Therefore, we suggest that, presumably, the effects of hypoxia-induced increased muscular activity may be responsible for an elevated CBF in brainstem regions of spontaneously breathing piglets (Fig. 1), which resulted from an additional vasodilatory response in these brain regions during moderate normocapnic hypoxia in spontaneously breathing newborn piglets.
A reduced neuronal activity in brain stem and cerebellum of newborns due to artificial ventilation can achieve clinical relevance: extubation failure in mechanically ventilated newborns, which is still more frequent than in older individuals [35], often resulted from insufficient central inspiratory drive [4]. This may be caused by prolonged reduction in brainstem activity. Not only respiration-related responses, but also effects of overall muscular paralysis may be responsible for reduced brainstem and cerebellar activity. Therefore, a related muscular (and possibly sensory) activation may improve timed onset of spontaneous breathing and may improve successful weaning. On the other hand, reduced neuronal activity in brain stem and cerebellum due to artificial ventilation may contribute to an improved compensation during critical period of oxygen loss due to hypoxic-ischemic injury in the immature brain. Perinatal hypoxic-ischemic cerebral injury is one of the most commonly recognized causes of severe, long-term neurological deficits in infants and children [36]. Parasagittal cerebral injury, the principal ischemic lesion of the term infant, refers to bilateral cortical and adjacent subcortical white matter necrosis. The necrosis occurs within border zones also referred to as watershed areas between the end branches of the major cerebral arteries. These regions are extremely vulnerable to decreases in cerebral perfusion [37]. In severe hypoxia-ischemia, survival is attempted by an intracerebral redistribution of blood flow from the forebrain to the vital centers of the brain stem [23]. Consequently, a reduced neuronal activity in brain stem and cerebellum owing to artificial ventilation should reduce the amount of intracerebral blood flow redistribution at the expense of forebrain structures.
Despite marked impact on regional CBF distribution in relation to the respiration modes used, especially during normocapnic hypoxia, there was no difference in systemic cardiovascular regulation between spontaneously breathing and mechanically ventilated newborn piglets. This is not surprising because it is known that systemic hypoxia induces a circulatory redistribution even in immature mammals which favors the blood flow towards the heart, brain, and adrenals at the expense of the other organs and tissues [10]. This is mainly affected by an increase in sympathoadrenal activity. However, in contrast to older animals, cardiovascular response in newborns is mainly caused by circulating catecholamines because of delayed central sympathetic maturity. Indeed, Lee and Downing have shown that hypoxia-induced cardiovascular responses were observed in intact and ganglionic blockade piglets, but no changes occurred in adrenalectomized piglets [38]. Direct stimulation of adrenal medulla and extramedullar chromaffin cells by reduced arterial PO2 is mainly responsible for increased catecholamine release in newborn rats early after birth [39].
In conclusion, there is a reduced blood flow of the brainstem, thalamus, and cerebellum in ventilated, anesthetized, and paralyzed piglets. This indicates a reduced neuronal activity in these brain regions. However, this does not impair cardiovascular regulation and forebrain oxidative metabolism, even during moderate normocapnic hypoxia.
References
Greisen G (1986) Cerebral blood flow in preterm infants during the first week of life. Acta Paediatr Scand 75:43–51
Pryds O, Greisen G, Lou H, Friis Hansen B (1989) Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr 115:638–645
Richter DW, Spyer KM (1990) Cardiorespiratory control. In: Loewy AD, KM Spyer (eds) Central regulations of autonomous control. Oxford Univ Press, New York, Oxford
Veness Meehan KA, Richter S, Davis JM (1990) Pulmonary function testing prior to extubation in infants with respiratory distress syndrome. Pediatr Pulmonol 9:2–6
Makowski EL, Meschia G, Droegemueller W, Battaglia FC (1968) Measurement of umbilical arterial blood flow to the sheep placenta and fetus in utero. Circ Res 23:623–631
Bauer R, Walter B, Wurker E, Kluge H, Zwiener U (1996) Colored microsphere technique as a new method for quantitative-multiple estimation of regional hepatic and portal blood flow. Exp Toxicol Pathol 48:415–420
Walter B, Bauer R, Gaser E, Zwiener U (1997) Validation of the multiple colored microsphere technique for regional blood flow measurements in newborn piglets. Basic Res Cardiol 92:191–200
Coyle MG, Oh W, Stonestreet BS (1993) Effects of indomethacin on brain blood flow and cerebral metabolism in hypoxic newborn piglets. Am J Physiol 264:H141-H149
Lerman J, Oyston JP, Gallagher TM, Miyasaka KAG, Volgyesi GA, Burrows FA (1990) The minimum aIveolar concentration (MAC) and hemodynamic effects of halothane, isoflurane, and sevoflurane in newborn swine. Anesthesiology 73:717–721
Bauer R, Walter B, Gaser E, Rosel T, Kluge H, Zwiener U (1998) Cardiovascular function and brain metabolites in normal weight and intrauterine growth restricted newborn piglets--effect of mild hypoxia. Exp Toxicol Pathol 50:294–300
Magistretti PJ (2000) Cellular bases of functional brain imaging: insights from neuron-glia metabolic coupling. Brain Res 886:108–112
Gjedde A, Marrett S (2001) Glycolysis in neurons, not astrocytes, delays oxidative metabolism of human visual cortex during sustained checkerboard stimulation in vivo. J Cereb Blood Flow Metab 21:1384–1392
Lauritzen M (2001) Relationship of spikes, synaptic activity, and local changes of cerebral blood flow. J Cereb Blood Flow Metab 21:1367–1383
Vannucci RC, Yager JY (1998) Perinatal brain metabolism. In: Polin RA, WW Fox (ed) Fetal and neonatal physiology. Saunders, Phiadelphia, pp 2123–2137
Gjedde A (1997)The relation between brain function and cerebral blood flow and metabolism. In: Hunt Batjer H (ed) Cerebrovascular disease. Lippincott-Raven, Philadelphia, pp 23–40
Hyder F, Shulman RG, Rothman DL (1998) A model for the regulation of cerebral oxygen delivery. J Appl Physiol 85:554–564
Hyder F, Shulman RG, Rothman DL (1999) Regulation of cerebral oxygen delivery. Adv Exp Med Biol 471:99–110
Vafaee MS, Gjedde A (2000) Model of blood-brain transfer of oxygen explains nonlinear flow-metabolism coupling during stimulation of visual cortex. J Cereb Blood Flow Metab 20:747–754
Langhorst P, Schulz B, Schulz G, Lambertz M (1983) Reticular formation of the lower brainstem. A common system for cardiorespiratory and somatomotor functions: discharge patterns of neighboring neurons influenced by cardiovascular and respiratory afferents. J Auton Nerv Syst 9:411–432
Gootman PM, Buckley NM, Gootman N, Crane LA, Buckley BJ (1978) Integrated cardiovascular responses to combined somatic afferent stimulation in newborn piglets. Biol Neonate 34:187–198
Flecknell PA, Wootton R, John M (1983) Cerebral blood flow and cerebral metabolism in normal and intrauterine growth retarded neonatal piglets. Clin Sci 64:161–165
Anday EK, Lien R, Goplerud JM, Kurth CD, Shaw LM (1993) Pharmacokinetics and effect of cocaine on cerebral blood flow in the newborn. Dev Pharmacol Ther 20:35–44
Ashwal S, Dale SP, Longo LD (1984) Regional cerebral blood flow: studies in the fetal lamb during hypoxia, hypercapnia, acidosis and hypotension. Pediatr Res 18:1309–1316
Chemtob S, Barna T, Beharry K, Aranda JV, Varma DR (1992) Enhanced cerebral blood flow autoregulation in the newborn piglet by d-tubocurarine and pancuronium but not by vecuronium. Anesthesiology 76:236–244
Easa D, Uyehara CF, Stevens EL, Finn KC, Balaraman V, Sim H (1993) Pancuronium does not alter the hemodynamic status of piglets after normoxia or hypoxia. Pediatr Res 33:365–372
Bauer R, Walter B, Zwiener U (2000) Effect of severe normocapnic hypoxia on renal function in growth-restricted newborn piglets. Am J Physiol Regul Integr Comp Physiol 279:R1010–1016
Eisenhauer CL, Matsuda LS, Uyehara CF (1994) Normal physiologic values of neonatal pigs and the effects of isoflurane and pentobarbital anesthesia. Lab Anim Sci 44:245–252
Leffler CW, Smith JS, Edrington JL, Zuckerman SL, Parfenova H (1997) Mechanisms of hypoxia-induced cerebrovascular dilation in the newborn pig. Am J Physiol 272:H1323–1332
Wilderman MJ, Armstead WM (1996) Relationship between nitric oxide and opioids in hypoxia-induced pial artery vasodilation. Am J Physiol 270:H869–874
Bari F, Thore CR, Louis TM, Busija DW (1998) Inhibitory effects of hypoxia and adenosine on N-methyl-D-aspartate- induced pial arteriolar dilation in piglets. Brain Res 780:237–244
Faraci FM, Heistad DD (1998) Regulation of the cerebral circulation: role of endothelium and potassium channels. Physiol Rev 78:53–97
Leffler CW (1997) Prostanoids: intrinsic modulators of cerebral circulation. News Physiol Sci 12:72–77
Shankar V, Armstead WM (1995) Opioids contribute to hypoxia-induced pial artery dilation through activation of ATP-sensitive K+ channels. Am J Physiol 269:H997–1002
Ben-Haim G, Armstead WM (2000) Stimulus duration-dependent contribution of k(ca) channel activation and cAMP to hypoxic cerebrovasodilation. Brain Res 853:330–337
Khan N, Brown A, Venkataraman ST (1996) Predictors of extubation success and failure in mechanically ventilated infants and children. Crit Care Med 24:1568–1579
Volpe JJ(1995) Neurology of the Newborn, 3rd edn. Saunders, Philadelphia
Perlman JM (1997) Intrapartum hypoxic-ischemic cerebral injury and subsequent cerebral palsy: medicolegal issues. Pediatrics 99:851–859
Lee JC, Werner JC, Downing SE (1980) Adrenal contribution to cardiac responses elicited by acute hypoxia in piglets. Am J Physiol 239:H751–755
Mojet MH, Mills E, Duchen MR (1997) Hypoxia-induced catecholamine secretion in isolated newborn rat adrenal chromaffin cells is mimicked by inhibition of mitochondrial respiration. J Physiol Lond 504:175–189
Acknowledgment
The authors thank Mrs. U. Jäger, Mrs. I. Witte, and Mr. L. Wunder for skillful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by Bundesministerium für Forschung und Technologie grant 01ZZ9104
Rights and permissions
About this article
Cite this article
Zwiener, U., Walter, B., Kratzsch, B. et al. Marked reduction of brainstem blood flow in artificially ventilated newborn piglets during normoxia and normocapnic hypoxia. Intensive Care Med 29, 2277–2284 (2003). https://doi.org/10.1007/s00134-003-2007-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-2007-5