Abstract
Purpose
In mental health care, patients and their care providers may conceptualize the nature of the disorder and appropriate action in profoundly different ways. This may lead to dropout and lack of compliance with the treatments being provided, in particular in young patients with more severe disorders. This study provides detailed information about patient–provider (dis)agreement regarding the care needs of children and adolescents.
Methods
We used the Camberwell Assessment of Need (CANSAS) to assess the met and unmet needs of 244 patients aged between 6 and 18 years. These needs were assessed from the perspectives of both patients and their care providers. Our primary outcome measure was agreement between the patient and care provider on unmet need. By comparing a general outpatient sample (n = 123) with a youth-ACT sample (n = 121), we were able to assess the influence of severity of psychiatric and psychosocial problems on the extent of agreement on patient’s unmet care needs.
Results
In general, patients reported unmet care needs less often than care providers did. Patients and care providers had the lowest extents of agreement on unmet needs with regard to “mental health problems” (k = 0.113) and “information regarding diagnosis/treatment” (k = 0.171). Comparison of the two mental healthcare settings highlighted differences for three-quarters of the unmet care needs that were examined. Agreement was lower in the youth-ACT setting.
Conclusions
Clarification of different views on patients’ unmet needs may help reduce nonattendance of appointments, noncompliance, or dropout. Routine assessment of patients’ and care providers’ perceptions of patients’ unmet care needs may also help provide information on areas of disagreement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over 40% of the children and adolescents who use mental healthcare terminate treatment prematurely, do not comply with treatment, or do not attend appointments regularly [1, 2]. Although this is a complex issue, one important factor may be that patients and mental healthcare providers do not agree on the nature of the problems and on the unmet care needs that need to be addressed during treatment [3,4,5]. Such a lack of agreement may lead to disagreement on the goals to be pursued and on appropriate treatment trajectories [6]. By negatively affecting attachment between patient and care provider, it may also affect their working relationship [7,8,9]. If the quality of the working alliance is poor, mental health problems may increase and functioning may deteriorate, ultimately leading to referral to a more intensive form of care [10,11,12,13].
We defined a “care need” as a physical, psychological, social, or environmental demand for aid, care or service intended to resolve a problem that a patient or his/her care provider perceived and expressed [14]. Care needs can be subdivided into (1) met needs, i.e., difficulties in a particular domain of functioning that are adequately taken care of; and (2) unmet needs, i.e., those for which a patient is not receiving the right care or the appropriate level of care [15].
Previous studies show that children and adolescents differ considerably from care providers with regard to the presence of psychiatric problems [16,17,18]. Care providers tend to report more problems than children/adolescents themselves. Higher levels of agreement were reported for externalizing problems (such as aggression and antisocial behavior) than for internalizing problems (such as sadness and anxiety) [16,17,18]. Although it is important during treatment to focus on psychiatric problems and related care needs, patients may also perceive care needs in other domains of functioning [19]. For this reason, a narrow focus on psychopathology-related care needs—and on possible disagreements between professionals and patients in this area—would not make it possible to fully understand patients’ unmet care needs. Overall, other studies in adults that had a broad focus on care needs in different areas of functioning found that psychiatric patients scored more unmet care needs than their care providers did [20,21,22], but that adult patients with severe psychiatric problems and psychosocial difficulties scored fewer needs [23].
There is currently little or no research on the extent to which children and adolescents agree or disagree with care providers on the broad range of met and unmet care needs. Therefore, the aim of our study was to obtain insight into the extent of agreement on these needs between the two groups. Further, we aimed to better understand whether the extent of agreement would differ between two setting with a different treatment intensity.
We had two a priori hypotheses: (1) that patients in the two settings would report less unmet care needs than their care providers; and (2) that we would find more disagreements between patients and care providers on the presence of patients’ unmet care needs in a youth-ACT setting—in other words, in a setting where patients had more severe psychiatric problems and psychosocial difficulties.
Methods
Design
In two different mental healthcare settings characterized by different severities of psychiatric problems and psychosocial difficulties, we used a cross-sectional design to compare the extent of agreement and disagreement between patients and mental healthcare providers on reported unmet care needs.
To increase our insight into the extent of agreement regarding these needs, we first established their frequencies in a specialized mental healthcare setting, approaching them from the perspectives of children and adolescents and also from those of care providers. We then examined the extent of agreement on these needs between the two groups. To better understand how the extent of agreement on patients' unmet care needs was influenced by the severity of psychiatric problems and by psychosocial difficulties, we compared unmet care needs between two treatment settings [24]. For this purpose, we included patients from a general outpatient mental healthcare setting and from youth-ACT, an Assertive Community Treatment setting. Youth-ACT is an intensive and outreaching mental healthcare service for children and adolescents with severe psychiatric and psychosocial problems [25,26,27].
Setting
The study was performed in a specialized treatment center for child and adolescent psychiatry in the Netherlands. Patients and care providers were included from two settings that provided care for the same catchment area.
The first was a general outpatient treatment setting (with low to moderate treatment intensity), in which treatment was provided by a multidisciplinary team consisting of one child psychiatrist, six psychologists, and one nurse practitioner, who made diagnostic assessments and provided cognitive behavioral therapy, eye-movement desensitization, and reprocessing therapy (EMDR); family support; and pharmacological treatment.
The second was a youth-ACT setting (Assertive Community Treatment with high treatment intensity) consisting of one child psychiatrist, five psychologists, three nurse practitioners, and two mental health nurses. This team offered home-based outreach-oriented treatment to patients with more severe psychiatric and psychosocial problems. Care providers had small shared caseloads (< 15 patients) and provided outreaching case management, early intervention, cognitive behavioral therapy, EMDR, family support, and pharmacological treatment. The intensity of ACT treatment was scaled up or down according to the severity of a patient’s current psychiatric symptoms and psychosocial impairments.
Participants
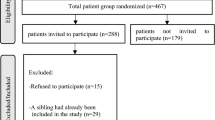
Figure 1 presents the flowchart for inclusion. Participants, who were recruited between 2014 and 2016, were patients aged between 6 and 18 years. A total of 467 patients were considered for participation in the study. An initial random sample of 133 patients was selected from the general outpatient population of 298 patients. Next, 10 of these outpatients had to be excluded because they already had a sibling who participated in the study (n = 2), they refused to participate (n = 6), or were referred to the youth-ACT setting during the inclusion period (n = 2). For the youth-ACT sample, we initially selected all patients who were referred from a general outpatient setting to this ACT treatment setting during the inclusion period (n = 169). Thereafter, 48 ACT patients had to be excluded because they did not meet the inclusion criteria: 27 patients because their sibling was already included in the study, 12 patients were not referred to the ACT setting from the outpatient setting, but by the general practitioner instead, and 9 patients refused to participate. The final sample consisted of 244 patients: 123 in the outpatient sample and 121 in the youth-ACT sample.
Ethical approval
The study was reviewed and approved by the Medical Ethical Committee at VU University Medical Centre Amsterdam (protocol no. 2015.245) and by the Scientific Committee at the EMGO+ Institute for Health and Care Research Amsterdam. Approval was also provided by the local scientific review board of the participating mental health institution.
Separately, children/adolescent participants, and their parents received written and oral information on the research project. In accordance with prevailing Dutch legislation, written consent from parents and/or children/adolescents was obtained as follows: (i) if children younger were aged less than 12, only parents were asked for consent for; (ii) if children were aged between 12 and 16, parents and children were both asked for consent; and (iii) if adolescents were 16 years or older, informed consent was obtained from them alone.
Measurement instruments
The Demographic Information Questionnaire (DEMOG) was used to measure the following four demographic characteristics of each child or adolescent: (1) age, (2) gender, (3) country of birth, and (4) living in a single-parent family or a two-parent family [28].
The Neuropsychiatric Interview for Children and Adolescent (MINI-KID) was used to assess patients’ psychiatric diagnoses [29], which were supplemented with clinical diagnoses that were not included in the MINI-KID [30].
The Camberwell Assessment of Need Short Appraisal Schedule (CANSAS) was used to assess the patient’s care needs as they were perceived both by the child/adolescent and by the mental healthcare provider [15]. CANSAS covers 23 items, each with three response options: (1) no need (= no problem); (2) met need (= difficulties in a particular domain of functioning that is receiving suitable assessment or intervention); (3) and unmet need (= difficulties in a particular domain of functioning that requires further assessment or is not receiving the right care or an appropriate level of care) [31]. To categorize CANSAS items (see Tables 2, 3), we used the following three International Classification of Functioning, Disability and Health (ICF) health and health-related domains: (i) physical and mental functions, (ii) performance of daily activities, and (iii) participation in the community [19, 32, 33].
Data analysis
The participants’ demographics were analyzed using descriptive statistics, first for the entire sample and then separately for the two subgroups (general outpatient setting and the youth-ACT setting). Subgroup differences regarding age, gender, country of birth, general functioning, and living situation were analyzed using the t test for continuous variables, or using the Chi-square test with Yates continuity correction (χ2 test) for categorical variables. As an alternative to the Chi-square test, Fisher’s exact test was computed if the number in at least one of the cells of the categorical variable was lower than 5 [34].
To analyze the extent of agreement between patients and care providers at item level, Cohen’s kappa coefficients were computed for the overall sample and then separately for the two treatment settings. On the basis of the Cohen’s kappa values, the extent of agreement was categorized as follows: poor (≤ 0.20); fair (0.21–0.40); moderate (0.41–0.60); good (0.61–0.80); or very good (≥ 0.81–1.00) [35].
To determine whether patient and care provider agreed or disagreed on the presence of an unmet need, the following calculation was made for both settings at CANSAS-item level: only the patient reported an unmet care need (P > CP); patient and care provider both reported the presence or absence of an unmet care need (P = CP); or only the care provider reported an unmet care need (P < CP) (see Table 3). Frequencies of agreement or disagreement on unmet care needs between patients and care providers were calculated for the two treatment settings, and subgroup differences between these settings were analyzed using Fisher’s exact test [34]. For all calculations, a value below p < 0.05 was considered to be statistically significant [35].
Results
Characteristics of the study sample
Table 1 shows the demographic characteristics of our two study samples. As would be expected, patients in the regular outpatient sample had a significantly higher score for overall functioning (GAF) than those in the youth-ACT sample (mean = 55.0, sd = 5.4 vs. mean = 45.9, sd = 8.0; p < 0.05).
In the subsample of youth-ACT patients significantly higher frequencies were found for ASD (39.7%), mood (37.2%), behavior (29.8%), somatoform (13.2%), and personality (2.9%), indicating higher levels of comorbidity in patients treated in youth-ACT. Significantly more of those receiving ACT treatment reported growing up in a single-parent family (42.3%) than those receiving regular outpatient treatment (26.2%; p < 0.05). There were no significant differences between the two samples regarding age, gender, and country of birth.
Agreement between patients and care providers in the overall sample
Table 2 shows the kappa coefficients (k) that were calculated to determine the agreement between patients and care providers in the overall sample at CANSAS item level. In general, patients reported unmet care needs less than care providers did. Below, our results are presented using the ICF domains, but, for purpose of conciseness, we now report only the results whose frequency in at least one of the two settings (outpatient or youth-ACT) was higher than 10%.
Physical and mental functions
Agreement between patients and care providers on unmet needs for “mental health problems”—the most reported unmet care need—was poor (k = 0.113), with the scores between patients (63.9%) and care providers (93.5%) differing significantly (p < 0.05). Agreement on unmet care need for “information regarding diagnosis/treatment” was also poor (k = 0.171), with patients (54.5%) reporting unmet needs significantly less than care providers (82.4%; p < 0.05). Agreement on “danger to others” was fair (k = 0.277), with patients reporting significantly fewer unmet needs (7.8%) than care providers (20.0%; p < 0.05). Agreement was also fair with regard to “danger to themselves” (k = 0.271), with patients reporting 7.4% and providers reporting 24.9% (p < 0.05). Agreement on unmet care needs related to “psychotic symptoms” was moderate (k = 0.438), with no significant differences between the two groups (patients 7.8% vs. providers 10.6%). Agreement for “medication side effects” was good (k = 0.660; patients 10.7% vs. providers 9.4%; ns). Agreement on physical functions was moderate for unmet needs related to “physical handicap or disease” (k = 0.570; patients 11.1% vs. providers 14.3%; ns). Finally, agreement on “quality or quantity of food” was only fair (k = 0.380), with no significant differences between the two groups (patients 7.8% vs. providers 12.7%).
Performance of daily activities
Patient–provider agreement on abilities of self-care (e.g., daily hygiene and oral health) as an unmet care was fair (k = 0.328); the difference between patients (9%) and care providers (21.6%) was statistically significant (p < 0.05). Agreement on “cleaning up room or bedroom” was also fair (k = 0.233; patients 6.1% vs. providers 13.1%; p < 0.05). Agreement on “handling money” was moderate (k = 0.411; patients 8.6% vs. providers 12.2%), as was agreement on “paid job or side job” (k = 0.534; patients 9.0% vs. providers 14.7%), with no significant difference between the two groups. Agreement on unmet needs regarding “reading and writing skills at expected grade level” was good (k = 0.687), with no significant difference between patients (13.4%) and care providers (15.5%).
Participation in the community
Agreement on “future prospects” (e.g., opportunities/changes for a successful and prosperous life)—a frequently reported unmet need—was fair (k = 0.346; patients 33.6% vs. providers 65.3%, p < 0.05). With regard to “making and/or keeping friends” as an unmet care need, patients, and care providers reported significantly differently, leading to only fair agreement (k = 0.299; 26.2% vs. 55.9%, respectively; p < 0.05). Agreement on unmet needs related to “regular/suitable school or other daytime activities” (e.g., practicing a hobby/sport) were moderate (k = 0.437), with significant differences between patients (23.0%) and providers (42.9%; p < 0.05). Patient–provider agreement for unmet care needs related to “intimate relations” was moderate (k = 0.561), with patients (7.4%) reporting significantly fewer unmet care needs related to “intimate relations” than care providers (14.7%; p < 0.05). Agreement on the presence of unmet needs related to “sexuality” was only poor (k = 0.181; patients 2.0% vs. providers 13.9%; p < 0.05).
Comparison of agreement between outpatient clinics and youth-ACT
Comparison of youth-ACT and outpatient clinics showed significant differences between the two settings for three-quarters of the unmet care needs that were investigated (see Table 3). Compared with their peers in the outpatient setting, youth-ACT patients agreed less with their care providers (P = CP) on the presence or absence of an unmet need for care. If there was disagreement, patients, unlike their care provider, did not usually report an unmet care need (P < CP). Below, for reasons of brevity, we highlight solely results of P < CP whose frequency in at least one of the two settings was higher than 10%.
Physical and mental functions
As Table 3 shows, relative to those in the outpatient setting, patients in the youth-ACT setting reported that they had no unmet needs with regard to “information regarding treatment and/or diagnosis” (P < CP 41.7%) significantly more than the care provider did (P < CP 26.0%; p < 0.05).
With regard to unmet care needs for “danger to others” and “danger to themselves,” patients and care providers (P < CP 31.7% and P < CP 26.7%, respectively) in the youth-ACT sample disagreed significantly more than patients and their care providers (P < CP 7.3% and P < CP 3.3%, respectively; p < 0.05) in the outpatient sample.
With regard to “quality and/or quantity of food”, there were significant differences (p < 0.05) between the two settings, with ACT patients (P < CP 14.2%) disagreements more on this item than outpatients (P < CP 2.4%).
With respect to the unmet need for “mental health problems”, there were no significant differences between patient–provider disagreements in the ACT setting (P < CP 35.0%) and those in the regular outpatient setting (P < CP 28.5%; ns).
Performance of daily activities
With regard to “abilities for self-care”, patients receiving youth-ACT treatment reported unmet care needs significantly less than their care providers (P < CP 25.0%), and significantly less than outpatients (P < CP 6.5%; p < 0.05). There were also significant differences (p < 0.05) between the youth-ACT sample and outpatient sample with regard to three unmet care needs: “cleaning-up room or bedroom” (youth-ACT P < CP 19.2% vs. outpatients P < CP 1.6%); “paid job or side job” (youth-ACT P < CP 14.2% vs. outpatients, P < CP 1.6%); and “handling money” (youth-ACT P < CP 12.5% vs. outpatients P < CP 2.4%).
Participation in the community
With regard to friendship-related unmet needs, patients in the youth-ACT sample scored significantly less than their care providers did (P < CP 50.8%), and significantly less than those receiving outpatient care (P < CP 16.3%; p < 0.05). Youth-ACT patients had significantly more patient–provider disagreements (p < 0.05) than outpatients with regard to unmet needs pertaining “future prospects” (youth ACT P < CP 45.0% vs. outpatients P < CP 22.0%); “regular/suitable school or other daytime activities” (youth-ACT vs. outpatients P < CP 38.3%, P < CP 8.1%); “sexuality” (youth-ACT P < CP 20.8% vs. outpatients P < CP 3.3%); and “intimate relations” (youth-ACT P < CP 15.0% vs. outpatients P < CP 0.8%).
Discussion
This study is based on the assumption that agreement among patients and care providers on relevant care needs is a prerequisite not only for efficient and effective collaboration, but also for treatment adherence and treatment outcomes. Although such agreement may be even more relevant among young patients than among adults, it has not, to our knowledge, been studied systematically.
In general, care needs (met and unmet) can be studied on different levels, e.g. (i) the problems experienced by the client; (ii) the interventions required to alleviate or limit these problems; (iii) the services required to provide these interventions. A specific problem can be solved (and related care needs can be met) by several different interventions, which can be applied by different types of services. Since the presence of a problem may require one or more interventions to ameliorate these problems, some authors suggested that needs should not only be assessed at the problem level, but also at the intervention level [36]. In this study we have focused in the first instance on the problem level because that is where the treatment process starts, namely with the initial question: do the patient and/or practitioner think the patient has a problem for which care is needed or not?
Agreement between patients and care providers in the overall sample
In general, agreement between patients and care providers with regard to patients' unmet care needs was low (see Table 2). While 23 unmet care needs were investigated, we found poor agreement for four, fair agreement for eight, moderate agreement for nine, and good agreement for only two. The lowest level of agreement was found for “mental health problems” and “information regarding diagnosis and/or treatment.” This is remarkable, as these two care needs are key topics during psychiatric treatment.
Overall, in line with our first hypothesis, patients reported fewer unmet care needs than their care providers (P < CP). The first possible explanation for this is that the care provider obtained information not only from the child, but also from the parents, whose views on appropriate care needs often differ from those of their children [37,38,39]. A second possible explanation lies in the rather self-evident fact that while patients tend to make personal statements, care providers’ statements also reflect a professional judgement [40].
Agreement in youth-ACT versus outpatient setting
Comparison of the youth-ACT setting with the general outpatient treatment setting showed significant differences with regard to three-quarters of the unmet care needs (see Table 3). In both settings, fewer patients than care providers reported unmet care needs (P < CP). The extent of disagreement was higher in the youth-ACT setting, which was in line with our second hypothesis. A possible explanation for this is that patients in the youth-ACT sample had more severe psychiatric problems [27]. Such patients are more likely to report fewer problems and needs—because they may be less aware of existing problems, are sometimes less willing to seek solutions, or believe that persisting problems cannot be resolved [23, 41, 42]. Higher frequencies of ASD (39.7%), mood (37.2%), behavior (29.8%) and somatoform (13.2%) were found in the youth-ACT sample (see Table 1). Overall, in the ACT sample more comorbidity was assessed, which supports the hypothesis that the patients in this sample had more severe psychopathology.
Another explanation why youth-ACT patients disagreed more than outpatients may be that more of these patients came from multiproblem families [27]. When a patient lives in an environment that is potentially harmful to his or her development, care providers tend to report more unmet care needs [43]. On the other hand, patients may be tempted to report unmet care needs less often when they have grown up in living situations in which they have become accustomed to the presence of problems. In contrast, care providers, who have more distance, do identify problems [44, 45].
A third explanation is that, due to the home visits ACT care providers made during the intake phase, when they observed patients in their own living environment, ACT care providers depended less than outpatient care providers on information provided by the patient to form a picture of his or her unmet care needs.
Implications for clinical practice and research
For clinical practice, the key to preventing noncompliance, nonattendance at appointments, and dropout may be in care providers’ awareness that their view of a patient’s unmet care needs often differs from that of the patient. We therefore recommend care providers—particularly those in youth-ACT settings or other intensive treatment settings—to routinely assess a child’s perceived care needs and compare them with their own perceptions of unmet care needs. Given the higher levels of comorbidity in the ACT sample, the examination of specific care needs related to this comorbidity should receive special attention in clinical practice. By sharing information on their perceptions of such needs, and by being explicit about the areas in which they disagree, patients and care providers can engage in a process of decision making that makes it possible to formulate goals and interventions on which they can then collaborate. Unmet care needs on which there is no agreement can be assessed according to their urgency; it may prove possible to postpone further attention to them until a later treatment phase.
We studied unmet care needs at the problem level, and investigated agreement regarding need for care, irrespectively of the type of intervention or services needed. In the future, it may be interesting to investigate whether different informants have a common view on the interventions required, once they agree on the problems that need to be addressed during treatment. Future research could also address the impact of improving agreement between patients and care providers with regard to unmet care needs on compliance with treatment and its outcomes.
Strengths and limitations
This is the first study to provide detailed information about patient–provider (dis)agreement regarding the care needs of children and adolescents who have been referred to general outpatient care and youth-ACT. This is a strength because children and adolescents with different severity levels of psychiatric problems were studied, which supported the generalizability of findings.
A limitation of the study is its cross-sectional design, which prevented us from identifying causes of disagreements between patients and care providers on patients’ unmet care needs [46].
Conclusions
We found that patients and care providers often disagreed on patients’ care needs, particularly in a youth-ACT treatment setting. Clarifying different views on patient’s unmet care needs may help to reduce nonattendance of appointments and early termination of treatment. Similarly, if patients and care providers systematically assessed patients’ unmet care needs, useful information may be provided on areas of disagreement. Future research should show whether better treatment outcomes would be produced by an approach focused on obtaining a shared view on unmet care needs.
Data availability
As the participants have not granted permission for data sharing, the data are not available.
Abbreviations
- ACT:
-
Assertive Community Treatment
- CANSAS:
-
Camberwell Assessment of Need Short Appraisal Schedule
- df:
-
Degrees of freedom
- CP:
-
Care provider
- EMDR:
-
Eye-movement desensitization and reprocessing therapy
- FE:
-
Fisher’s exact test
- GAF score:
-
Global Assessment of Functioning score
- ICF:
-
International Classification of Functioning and Disability
- K:
-
Cohen’s kappa coefficient
- MINI-KID:
-
MINI International Neuropsychiatric Interview for Children and Adolescents
- ns:
-
Not significant
- P:
-
Patient
- SD:
-
Standard deviation
- SPSS:
-
Statistical Package for the Social Sciences
- χ2 test:
-
Chi-square test
References
de Haan A, Boon A, de Jong J, Hoeve M, Vermeieren R (2013) A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin Psychol Rev 33(5):698–711. https://doi.org/10.1016/j.cpr.2013.04.005(PMID: 23742782)
Navridi E, Midgley N (2007) An exploratory study of premature termination in child analysis. J Infant Child Adolesc Psychother 5(4):437–458. https://doi.org/10.1080/15289160701382360
Corkum P, Bessey M, McGonnell M, Dorbeck A (2015) Barriers to evidence-based treatment for children with attention-deficit/hyperactivity disorder. Atten Defic Hyperact Disord 7(1):49–74. https://doi.org/10.1007/s12402-014-0152-z(PMID: 25055885)
Garcia J, Weisz J (2002) When youth mental health care stops: therapeutic relationships problems and other reasons for ending youth outpatient treatment. J Consult Clin Psychol 70(2):439–443. https://doi.org/10.1037/0022-006X.70.2.439(PMID: 11952203)
Reininghaus U, McCabe R, Slade M, Burns T, Croudace T, Priebe S (2013) The validity of patient- and clinician-rated measures of needs and the therapeutic relationship in psychosis: a pooled analysis. Psychiatry Res 209(3):711–720. https://doi.org/10.1016/j.psychres.2013.01.013(PMID: 23452753)
Tryon G, Winograd G (2011) Goal consensus and collaboration. Psychotherapy 48(1):50–57. https://doi.org/10.1037/a0022061(PMID: 21401274)
Bordin E (1979) The generalizability of the psychoanalytic concept of the working alliance. Psychother Theor Res Pract 16(3):252–260. https://doi.org/10.1037/h0085885
Luborsky L (2002) A pattern-setting therapeutic alliance study revisited. Psychother Res 10(1):17–29. https://doi.org/10.1093/ptr/10.1.17
Shirk S, Saiz C (1992) Clinical, empirical, and developmental perspectives on the therapeutic relationship in child psychotherapy. Dev Psychopathol 4(4):713–728. https://doi.org/10.1017/S0954579400004946
Shirk S, Karver M (2003) Prediction of treatment outcome from relationship variables in child psychotherapy: a meta-analytic review. J Consult Clin Psychol 71(3):452–464. https://doi.org/10.1037/0022-006X.71.3.452(PMID: 12795570)
Karver M, De Nadai A, Monahan M, Shirk S (2018) Meta-analysis of the prospective relation between alliance and outcome in child and adolescent psychotherapy. Psychotherapy 55(4):341–355. https://doi.org/10.1037/pst0000176(PMID: 30335449)
Ford T, Macdiarmid F, Russell D, Racey D, Goodman R (2017) The predictors of persistent DSM-IV disorders in 3-years follow-ups of the British child and adolescent mental health surveys 1999 and 2004. Psychol Med 47(6):1126–1137. https://doi.org/10.1017/S0033291716003214(PMID: 27995813)
Murphy R, Hutton P (2018) Practitioner review: therapist variability, patient-reported therapeutic alliance, and clinical outcomes in adolescent undergoing mental health treatment - a systematic review and meta-analysis. J Child Psychol Psychiatry 59(1):5–19. https://doi.org/10.1111/jcpp.12767(PMID: 28681928)
Houtjes W (2015) Needs of elderly people with late-life depression: challenges for care improvement. Vrije Universiteit Amsterdam. ISBN: 978-94-6108-985-4
Phelan M, Slade M, Thornicroft G, Dunn G, Holloway F, Wykes T (1995) The Camberwell Assessment of Need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. Br J Psychiatry 167(5):589–595. https://doi.org/10.1192/167.5.589(PMID: 8564313)
Schultze-Lutter F, Renner F, Paruch J, Julkowski D, Ruhrmann S (2014) Self-reported psychotic-like experiences are a poor estimate of clinician-rated attenuated and frank delusions and hallucinations. Psychopathology 47(3):194–201. https://doi.org/10.1159/000355554(PMID: 24192655)
Dolle K, Schulte-Körne G, von Hofacker N, Izat Y, Allgaier A (2012) Agreement of clinical diagnosis, structured interviews, and self-report questionnaires for depression in children and adolescent. Z Kinder Jugendpsychiatr Psychother 40(6):405–414. https://doi.org/10.1024/1422-4917/a000200(PMID: 23109129)
De Los RA, Ohannessian C (2016) Introduction to the special issue: discrepancies in adolescent–parent perceptions of the family and adolescent adjustment. J Youth Adolesc 45(10):1957–1972. https://doi.org/10.1007/s10964-016-0533-z(PMID: 27384957)
World Health Organization (2016) International statistical classification of diseases and related health problems, 10th version. WHO Press, Geneva https://icd.who.int/browse10/Content/statichml/ICD10Volume2_en_2016.pdf. Accessed 10 Feb 2020
Houtjes W, van Meijel B, Deeg D, Beekman A (2011) Unmet needs of outpatients with late-life depression; a comparison of patient, staff and carer perceptions. J Affect Disord 134(1–3):242–248. https://doi.org/10.1016/j.jad.2011.05.052(PMID: 21684611)
Junghan U, Leese M, Priebe S, Slade M (2007) Staff and patient perspectives on unmet need and therapeutic alliance in community mental health services. Br J Psychiatry 191(6):543–547. https://doi.org/10.1192/bjp.bp.107.037978(PMID: 18055959)
Lasalvia A, Ruggeri M, Mazzi M, Dall'Agnola R (2000) The perception of needs for care in staff and patients in community-based mental health services: the South-Verona outcome project 3. Acta Psychiatr Scand 102(5):366–375. https://doi.org/10.1034/j.1600-0447.2000.102005366.x(PMID: 11098809)
Lasalvia A, Bonetto C, Tansella M, Stefani B (2007) Does staff-patient agreement on needs for care predict a better mental health outcome? A 4-year follow-up in a community service. Psychol Med 38(1):123–133. https://doi.org/10.1017/S0033291707000785(PMID: 17537280)
Vijverberg R, Ferdinand R, van Meijel B, Beekman A (2020) Unmet care needs of children with ADHD. PLoS One 15(1):e0228049. https://doi.org/10.1371/journal.pone.0228049(PMID: 31951639)
Rots-de Vries C, van Goor I, Stronks K, Garretsen H (2011) Evaluation of an assertive outreach intervention for problem families: intervention methods and early outcomes. Scand J Caring Sci 25(2):211–219. https://doi.org/10.1111/j.1471-6712.2010.00811.x(PMID: 20626696)
Russell A, Ford T, Russell G (2018) The relationship between financial difficulty and childhood symptoms of attention deficit/hyperactivity disorder: a UK longitudinal cohort study. Soc Psychiatry Psychiatr Epidemiol 53(1):33–44. https://doi.org/10.1007/s00127-017-1453-2(PMID: 29124294)
Vijverberg R, Ferdinand R, Beekman A, van Meijel B (2018) Factors associated with treatment intensification in child and adolescent psychiatry. BMC Psychiatry 18(291):1–10. https://doi.org/10.1186/s12888-018-1874-9(PMID: 30200911)
Reflectum (2013) Bibliotheek vragenlijsten NVPP/LVE. Reflectum, Deventer
Sheehan D, Sheehan K, Shytle R, Janavs J, Bannon Y, Rogers J, Milo K, Stock S, Wilkinson B (2010) Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). J Clin Psychiatry 71(3):313–326. https://doi.org/10.4088/JCP.09m05305whi(PMID: 20331933)
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Association Publishing, Arlington
Hancock G, Orrell M (2004) Introduction: defining need. In: CANE - Camberwell Assessment of Need for elderly: a needs assessment for older mental health service users. Gaskell, London
Dobryzynska E, Rymanszewska J, Biecek P, Kiejna A (2016) Do mental health outpatient services meet users' needs? Trail to identify factors associated with higher needs for care. Community Ment Health J 52(4):472–478. https://doi.org/10.1007/s10597-015-9923-z(PMID: 26387519)
Üstün T (2007) Using the international classification of functioning, disease and health in attention-deficit/hyperactivity disorder: separating the disease form its epiphenomena. Ambul Pediatr 7(1):132–139. https://doi.org/10.1016/j.ambp.2006.05.004(PMID: 17261492)
Campbell I (2007) Chi-squared and Fisher−Irwin test of two-by-two tables with small sample recommendations. Stat Med 26(19):3661–3675. https://doi.org/10.1002/sim.2832(PMID: 17315184)
Altman D (1991) Practical statistics for medical research. Chapman & Hall, London
Ljunggren G (2004) Needs assessment. In: Nies H, en Berman P (eds) Integrating services for older people: a resource book for managers. European Health Management Association, Dublin, pp 67–81
Kolko D, Kazdin A (1993) Emotional/behavioral problems in clinic an nonclinic children: correspondence among child, parent and teacher reports. J Child Psychol Psychiatry 34(6):991–1006. https://doi.org/10.1111/j.1469-7610.1993.tb01103.x(PMID: 8408380)
Thurber S, Osborn R (1993) Comparisons of parent and adolescent perspectives on deviance. J Genet Psychol 154(1):25–32. https://doi.org/10.1080/00221325.1993.9914718(PMID: 8331327)
Salbach-Andrae H, Lenz K, Lehmkuhl U (2009) Patterns of agreement among parent, teacher and youth ratings in a referred sample. Eur Psychiatry 24(5):345–351. https://doi.org/10.1016/j.eurpsy.2008.07.008(PMID: 18789656)
Buckingham S, Brandt N, Becker K, Gordon D, Cammack N (2016) Collaboration, empowerment and advocacy: consumer perspectives about treatment engagement. J Child Fam Stud 25(12):3702–3715. https://doi.org/10.1007/s10826-016-0507-5
Mulder C, Jochems E, Kortrijk H (2014) The motivational paradox: higher psychosocial problem levels in severely mentally ill patients are associated with less motivation for treatment. Soc Psychiatry Psychiatr Epidemiol 49(4):541–548. https://doi.org/10.1007/s00127-013-0779-7(PMID: 24136001)
Bachler E, Fruehmann A, Bachler H, Aas B, Nickel M, Schiepek G (2017) Patterns of change in collaboration are associated with baseline characteristics and predict outcome and dropout rates in treatment of multi-problem families. A validation study. Front Psychol 8:1221. https://doi.org/10.3389/fpsyg.2017.01221(PMID: 28785232)
De Los RA, Augenstein T, Wang M, Thomas S, Drabick D, Burgers D et al (2015) The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull 141(4):858–900. https://doi.org/10.1037/a0038498(PMID: 25915035)
Vaessen G (2009) Multi-probleemgezinnen in de jeugdzorg. Garant, Antwerpen
Balcher E, Frühmann A, Strunk G, Aas B, Bachler H, Nickel M (2016) Differential effects of the working alliance in family home-based treatment of multi-problem families. J Fam Ther 38(1):120–148. https://doi.org/10.1111/1467-6427.12063
Polit D, Beck C (2017) Nursing research: generating and assessing evidence for nursing practice, 10th edn. Wolters Kluwer, Philadelphia
Acknowledgements
The authors gratefully acknowledge the families and mental healthcare providers who participated. They also acknowledge research assistant Amanda Noorman, who helped conduct the study. We thank Adriaan Hoogendoorn and David Alexander for their valuable comments on this paper. We would also like to thank Daphne van de Draai for her assistance with building the SPSS files.
Funding
This research was funded by GGZ Delfland Psychiatric Institute, which played no role in the design of the study, in the collection, analysis or interpretation of the data; or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
RV, RF, AB, and BM designed this study. RV and RF performed the analysis and interpreted the data. RV and RF wrote the manuscript. BM and AB critically revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Medical Ethics Committee on Research Involving Human Subjects at VU University Medical Centre, Amsterdam (protocol no. 2015.245).
Consent to participate
Participants received written and oral information on the research project; children and parents received this separately. Prior to participation, written consent from the parents and/or children was obtained, according to three age categories: Category 1: Parents were asked for consent for children < 12 years old. Category 2: If children were between the ages of 12 and < 16 years old, parents and children alike were asked for consent. Category 3: Informed consent was obtained from children (not parents) only if they were aged ≥ 16.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vijverberg, R., Ferdinand, R., Beekman, A. et al. Agreement between patients and mental healthcare providers on unmet care needs in child and adolescent psychiatry. Soc Psychiatry Psychiatr Epidemiol 56, 2005–2015 (2021). https://doi.org/10.1007/s00127-020-01969-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-020-01969-8