Abstract
Purpose
Lack of motivation for treatment makes a subgroup of patients with severe mental illness (SMI) difficult to engage in psychiatric treatment. Such difficult-to-engage patients may also be the most in need of treatment. We hypothesized that the level of psychosocial problems would be inversely related to motivation for treatment.
Methods
Cross-sectional study in two independent samples. The first sample (n = 294) included SMI patients who participated in a randomized controlled trial and were assessed using the Health of the Nation Outcome Scales (HoNOS) and self-rated and clinician-rated motivation-for-treatment scales. The second sample (n = 1,170) included SMI patients who were treated in Assertive Outreach Teams and were routinely assessed with the HoNOS and a motivation-for-treatment scale. In both samples, patients also self-rated their quality of life.
Results
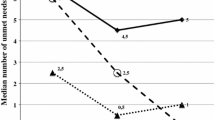
In both samples, patients with HoNOS scores of 16 and higher had lower motivation scores on all motivation scales than patients with lower HoNOS scores, and also a lower quality of life.
Conclusions
A motivation paradox seems inherent to this association between higher psychosocial problems levels, less motivation for treatment, and lower quality of life. Such a paradox has clinical relevance, as it may provide an ethical basis for outreach services which aim to engage marginally motivated SMI patients with severe psychosocial problems into mental health care.
Similar content being viewed by others
References
Torrey EF, Zdanowicz M (2001) Outpatient commitment: what, why, and for whom. Psychiatr Serv 52(3):337–341
Nose M, Barbui C, Tansella M (2003) How often do patients with psychosis fail to adhere to treatment programmes? A systematic review. Psychol Med 33(7):1149–1160
Killaspy H, Banerjee S, King M, Lloyd M (2000) Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. Br J Psychiatry 176:160–165
Drieschner KH, Lammers SMM, van der Staak CPF (2004) Treatment motivation: an attempt for clarification of an ambiguous concept. Clin Psychol Rev 23(8):1115–1137
Barkhof E, Meijer CJ, de Sonneville LM, Linszen DH, de Haan L, de Sonneville LMJ (2012) Interventions to improve adherence to antipsychotic medication in patients with schizophrenia—a review of the past decade. Eur Psychiatry J Assoc Eur Psychiatr 27(1):9–18
McMurran M, Huband N, Overton E (2010) Non-completion of personality disorder treatments: a systematic review of correlates, consequences, and interventions. Clin Psychol Rev 30(3):277–287
Kortrijk HE, Mulder CL, Roosenschoon BJ, Wiersma D (2010) Treatment outcome in patients receiving assertive community treatment. Community Ment Health J 46(4):330–336
Davis S (2002) Autonomy versus coercion: reconciling competing perspectives in community mental health. Community Ment Health J 38(3):239–250
Williamson T (2002) Ethics of assertive outreach (assertive community treatment teams). Curr Opin Psychiatry 15(5):543–547
van Beek N, Verheul R (2008) Motivation for treatment in patients with personality disorders. J Pers Disord 22(1):89–100
Velasquez MM, Crouch C, von Sternberg K, Grosdanis I (2000) Motivation for change and psychological distress in homeless substance abusers. J Subst Abuse Treat 19(4):395–401
Wing JK, Beevor AS, Curtis RH, Park SB, Hadden S, Burns A (1998) Health of the nation outcome scales (HoNOS). Research and development. Br J Psychiatry 172:11–18
Jochems EC, Mulder CL, van Dam A, Duivenvoorden HJ, Scheffer SC, van der Spek W et al (2012) Motivation and treatment engagement intervention trial (MotivaTe-IT): the effects of motivation feedback to clinicians on treatment engagement in patients with severe mental illness. BMC Psychiatry 12:209
van Veldhuizen JR (2007) FACT: a Dutch version of ACT. Community Ment Health J 43(4):421–433
Mulder CL, Staring ABP, Loos J, Buwalda VJA, Kuijpers S, Sytema S et al (2004) De Health of the Nation Outcome Scales (HoNOS) als instrument voor ‘routine outcome assessment’. Tijdschr Psychiatr 46:273–284
Drieschner KH (2005) Measuring treatment motivation and treatment engagement in forensic psychiatric outpatient treatment: development of two instruments. Febodruk, Enschede
Ryan RM, Plant RW, O’Malley S (1995) Initial motivations for alcohol treatment: relations with patient characteristics, treatment involvement, and dropout. Addict Behav 20(3):279–297
Wild T, Cunningham JA, Ryan RM (2006) Social pressure, coercion, and client engagement at treatment entry: a self-determination theory perspective. Addict Behav 31(10):1858–1872
Drieschner KH, Boomsma A (2008) The Treatment Motivation Scales for forensic outpatient treatment (TMS-F): construction and psychometric evaluation. Assessment 15(2):224–241
Drieschner KH, Boomsma A (2008) Validation of the Treatment Motivation Scales for Forensic outpatient treatment (TMS-F). Assessment 15(2):242–255
Deci EL, Ryan RM (2000) The “What” and “Why” of goal pursuits: human needs and the self-determination of behavior. Psychol Inq Int J Adv Psychol Theory 11(4):227–268
Ryan RM, Deci EL (2008) A self-determination theory approach to psychotherapy: the motivational basis for effective change. Can Psychol 49(3):186–193
Ryan RM, Lynch MF, Vansteenkiste M, Deci EL (2010) Motivation and autonomy in counselling, psychotherapy, and behavior change: a look at theory and practice. Couns Psychol 39(2):193–260
Priebe S, Huxley P, Knight S, Evans S (1999) Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Int J Soc Psychiatry 45(1):7–12
Drukker M, van Os J, Bak M, a Campo J, Delespaul P (2010) Systematic monitoring of needs for care and global outcomes in patients with severe mental illness. BMC Psychiatry 10:36
Drukker M, Bak M, Campo J, Driessen G, Van Os J, Delespaul P (2010) The cumulative needs for care monitor: a unique monitoring system in the south of the Netherlands. Soc Psychiatry Psychiatr Epidemiol 45(4):475–485
Kortrijk HE, Mulder CL, van der Gaag M, Wiersma D (2012) Symptomatic and functional remission and its associations with quality of life in patients with psychotic disorder in Assertive Community Treatment teams. Compr Psychiatry 53(8):1174–1180
Katsakou C, Rose D, Amos T, Bowers L, McCabe R, Oliver D et al (2012) Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol 47(7):1169–1179
Lundahl B, Burke BL (2009) The effectiveness and applicability of motivational interviewing: a practice-friendly review of four meta-analyses. J Clin Psychol 65(11):1232–1245
Sytema S, Wunderink L, Bloemers W, Roorda L, Wiersma D (2007) Assertive community treatment in the Netherlands: a randomized controlled trial. Acta Psychiatr Scand 116(2):105–112
Burns T (2010) The rise and fall of assertive community treatment? Int Rev Psychiatry 22(2):130–137
Mulder CL, Ruud T, Bahler M, Kroon H, Priebe S (2013) The availability and quality across Europe of outpatient care for difficult-to-engage patients with severe mental illness: a survey among experts. Int J Soc Psychiatry [Epub ahead of print]
Thornicroft G, Tansella M (2013) The balanced care model for global mental health. Psych Med 43(4):849–863
Jochems EC, Mulder CL, van Dam A, Duivenvoorden HJ (2011) A critical analysis of the utility and compatibility of motivation theories in psychiatric treatment. Curr Psych Rev 7(4):298–312
Acknowledgments
This work was funded by Bavo-Europoort and the Epidemiological and Social Psychiatric Research institute, Erasmus MC.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mulder, C.L., Jochems, E. & Kortrijk, H.E. The motivation paradox: higher psychosocial problem levels in severely mentally ill patients are associated with less motivation for treatment. Soc Psychiatry Psychiatr Epidemiol 49, 541–548 (2014). https://doi.org/10.1007/s00127-013-0779-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-013-0779-7