Abstract
Purpose
While studies indicate that few children with anxiety disorders receive specialized mental health care, significant knowledge gaps exist for the mental health care trajectory outside of specialized care. We examined whether physician-based care after an emergency department (ED) visit for mental health care predicted time to ED return.
Methods
We conducted a retrospective cohort study using administrative data from Alberta, Canada. Included in the cohort were 8075 children <18 years discharged from an ED (104 EDs in total), April 2002–September 2010, following a visit for an anxiety disorder or acute stress reaction. We used a multivariable Cox proportional hazards model to estimate time to ED return for mental health care (censored at 90 days). The variables of interest were: number and type of physician visits 30 days after index visit. We adjusted for sociodemographics, clinical acuity, comorbidity, and recent history of ED mental health care in the model.
Results
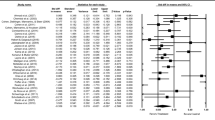
Within 30 days of ED discharge, multiple physician follow-up visits were associated with shorter return time (adjusted HR 1.24, 95 % CI 1.08–1.43). A single physician follow-up visit was associated with longer return time (adjusted HR 0.68, 95 % CI 0.58–0.79). Physician follow-up visits for mental health care were associated with shorter return time (adjusted HR 2.5, 95 % CI 2.21–2.83).
Conclusions
Following an index visit, ED return by children with anxiety disorders or acute stress reactions is associated with specific characteristics of subsequent physician visits. Improving physician use of evidence-based treatment and family access to coordinated services may reduce costly hospital-based care.
Similar content being viewed by others
References
Merikangas KR, He JP, Burnstein M, Swanson SA, Aveneoli S, Cui L, Benjet C, Georgiades K, Swendsen J (2010) Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 49(10):980–989
Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, He JP, Koretz D, McLaughlin KA, Petukhova M, Sampson NA, Zaslavsky AM, Merikangas KR (2012) Prevalence, persistence, and sociodemographic correlates of DMS-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry 69:372–380
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593–602
Merikangas KR, He JP, Burnstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M (2011) Service utilization for lifetime mental disorders in US adolescents: results of the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 50(1):32–45
Dolan MA, Mace SE, American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, American College of Emergency Physicians and Pediatric Emergency Medicine Committee (2006) Pediatric mental health emergencies in the emergency medical services system. Pediatrics 118:1764–1767
Dolan MA, Fein JA, Committee on Pediatric Emergency Medicine (2011) Technical report: pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics 127:e1356–e1366
Taastrøm A, Klahn J, Staal N, Thomsen PH, Johansen A (2014) Children and adolescents in the psychiatric emergency department: a 10-year survey in Copenhagen Country. Nord J Psychiatry 68:385–390
Sills MR, Bland SD (2002) Summary statistics for pediatric psychiatric visits to US emergency departments, 1993–1999. Pediatrics 110:340
Newton AS, Ali S, Johnson DW, Haines C, Rosychuk JR, Keaschuk RA, Jacobs P, Klassen TP (2009) A four-year review of pediatric mental health emergencies in Alberta. CJEM 11(5):447–454
Newton AS, Ali S, Johnson DW, Haines C, Rosychuk RJ, Keaschuk RA, Jacobs P, Cappelli M, Klassen TP (2010) Who comes back? Characteristics and predictors of return to emergency department services for pediatric mental health care. Acad Emerg Med 17(2):177–186
Alberta Health and Wellness (2004) Ambulatory care in Alberta using Ambulatory Care Classification System data. Edmonton, Canada
World Health Organization (2010) International Statistical Classification of Diseases and Related Health Problems. http://apps.who.int/classifications/icd10/browse/2010/en Accessed 6 May 2011
Gravel J, Manzano S, Arsenault M (2009) Validity of the Canadian Paediatric Triage and Acuity Scale in a tertiary care hospital. CJEM 11(1):23–28
Warren DW, Jarvis A, LeBlanc L, Gravel J, CTAS National Working Group; Canadian Association of Emergency Physicians; National Emergency Nurses Affiliation; Association des Médicins d’Urgence du Québec; Canadian Paediatric Society; Society of Rural Physicians of Canada (2008) Revisions to the Canadian Triage and Acuity Scale paediatric guidelines (PaedCTAS). CJEM 10(3):224–243
Practice Management Information Corporation (1989) International Classification of Diseases and related health problems (9th revision. Clinical Modification), 3rd edn Practice Management Information Corporation, Los Angeles, CA
Aboriginal Affairs and Northern Development Canada (2012) Indian and Northern Affairs Canada Terminology. http://www.aadnc-aandc.gc.ca/eng/1100100014642 Accessed 6 May 2011
Ramsawh HJ, Chavira DA, Kanegaye JT, Ancoli-Isreal S, Madati PJ, Stein MB (2012) Screening for adolescent anxiety disorders in a pediatric emergency department. Pediatr Emer Care 28:1041–1047
Mahajan P, Alpern ER, Grupp-Phelan J, Chamberlain J, Dong L, Holubkov R, Jacobs E, Stanley R, Tunik M, Sonnett M, Miller S, Foltin GL, Pediatric Emerency Care Applied Research Network (PECARN) (2009) Epidemiology of psychiatric-related visits to emergency departments in a multicenter collaborative research pediatric network. Pediatr Emer Care 25:715–720
Newton AS, Rosychuk RJ, Dong K, Curran J, Slomp M, McGrath PJ (2012) Emergency health care use and follow-up among sociodemographic groups of children who visit emergency departments for mental health crises. CMAJ 184:E665–E674
Snowden LR, Masland MC, Libby AM, Wallace N, Fawley K (2008) Racial/ethnic minority children’s use of psychiatric emergency care in California’s public mental health system. Am J Public Health 98:118–124
Snowden LR, Masland MC, Fawley K, Wallace N (2009) Ethnic differences in children’s entry into public mental health care via emergency mental health services. J Child Fam Stud 18:512–519
Connolly SD, Bernstein GA, Work Group on Quality Issues (2007) Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Adolesc Psychiatry 46(2):267–283
Chavira DA, Drahota A, Garland AF, Roesch S, Garcia M, Stein MB (2014) Feasibility of two modes of treatment delivery for child anxiety in primary care. Behav Res Ther 60:60–66
Thirlwall K, Cooper PJ, Karalus J, Voysey M, Willetts L, Creswell C (2013) Treatment of child anxiety disorders via guided parent-delivered cognitive-behavioural therapy: a randomised controlled trial. Br J Psychiatry 203(6):436–444
Adelman CB, Panza KE, Bartley CA, Bontempo A, Bloch MH (2014) A meta-analysis of computerized cognitive-behavioral therapy for the treatment of DSM-5 anxiety disorders. J Clin Psychiatry 75:e695–e704
Brown NM, Green JC, Desai MM, Weitzman CC, Rosenthal MS (2014) Need and unmet need for care coordination among children with mental health conditions. Pediatrics 133:e530–e537
Acknowledgments
This study is based in part on data provided by Alberta Health. The interpretation and conclusions contained herein are those of the researchers and do not necessarily represent the views of the Government of Alberta. Neither the Government of Alberta nor Alberta Health expresses any opinion in relation to this study. We thank Cathy McPhalen for her editorial contributions to this manuscript. We thank Jingbin Zhang for carrying out additional analyses based on peer review feedback. All phases of this study were supported by a grant from the Canadian Institutes of Health Research (CIHR; grant SFR1231). Dr. Newton holds a CIHR New Investigator Award. Dr. Rosychuk is a Health Scholar with Alberta Innovates-Health Solutions. Dr. McGrath holds a Canada Research Chair (Tier 1) in children’s health.
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Newton, A.S., Rosychuk, R.J., Niu, X. et al. Predicting time to emergency department return for anxiety disorders and acute stress reactions in children and adolescents: a cohort study. Soc Psychiatry Psychiatr Epidemiol 50, 1199–1206 (2015). https://doi.org/10.1007/s00127-015-1073-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-015-1073-7