Abstract
Aims/hypothesis
The Gq-coupled 5-hydroxytryptamine 2B (5-HT2B) receptor is known to regulate the proliferation of islet beta cells during pregnancy. However, the role of serotonin in the control of insulin release is still controversial. The aim of the present study was to explore the role of the 5-HT2B receptor in the regulation of insulin secretion in mouse and human islets, as well as in clonal INS-1(832/13) cells.
Methods
Expression of HTR2B mRNA and 5-HT2B protein was examined with quantitative real-time PCR, RNA sequencing and immunohistochemistry. α-Methyl serotonin maleate salt (AMS), a serotonin receptor agonist, was employed for robust 5-HT2B receptor activation. Htr2b was silenced with small interfering RNA in INS-1(832/13) cells. Insulin secretion, Ca2+ response and oxygen consumption rate were determined.
Results
Immunohistochemistry revealed that 5-HT2B is expressed in human and mouse islet beta cells. Activation of 5-HT2B receptors by AMS enhanced glucose-stimulated insulin secretion (GSIS) in human and mouse islets as well as in INS-1(832/13) cells. Silencing Htr2b in INS-1(832/13) cells led to a 30% reduction in GSIS. 5-HT2B receptor activation produced robust, regular and sustained Ca2+ oscillations in mouse islets with an increase in both peak distance (period) and time in the active phase as compared with control. Enhanced insulin secretion and Ca2+ changes induced by AMS coincided with an increase in oxygen consumption in INS-1(832/13) cells.
Conclusions/interpretation
Activation of 5-HT2B receptors stimulates GSIS in beta cells by triggering downstream changes in cellular Ca2+ flux that enhance mitochondrial metabolism. Our findings suggest that serotonin and the 5-HT2B receptor stimulate insulin release.
Similar content being viewed by others
Introduction
Glucose-induced insulin secretion is modulated by G protein-coupled receptors and their endogenous ligands [1–3]. Therefore, pathways activated by such receptors are often evaluated as pharmaceutical targets in diabetes treatment. The introduction of incretin-based therapies (e.g. glucagon-like peptide 1 [GLP-1] analogues used for treating type 2 diabetes) is a successful example of this approach [4, 5].
Serotonin (5-hydroxytryptamine [5-HT]) receptors are expressed in rodent islets [6–8] and virtually all 5-HT receptors (5-HT1–7) are G protein-coupled with the exception of 5-HT3 receptors (ligand-gated K+ and Na+ ion channels) [9]. Recently, microarray and RNA sequencing analyses revealed transcripts of almost all 5-HT receptors in human islets [10, 11]. The natural ligand binding to these receptors, 5-HT, is synthesised from the amino acid tryptophan, is a well-established neurotransmitter in the central nervous system and is involved in regulation of mood and behaviour [9]. 5-HT has also been detected in islets of Langerhans in several mammalian species [12], including human islets [11], and is suggested to be co-released with insulin and ATP from rodent beta cells [13–16]. However, rodent islet studies examining the effects of 5-HT on insulin secretion have produced contradictory results; an inhibition [17, 18] or a stimulation [19] of glucose-stimulated insulin secretion (GSIS) has been observed. Others propose that 5-HT directly stimulates beta cell exocytosis by receptor-independent mechanisms [20], termed serotonylation, a process where serotonin covalently binds to small GTPases.
Recently, 5-HT was implicated in beta cell expansion and compensatory insulin secretion during pregnancy [6, 8, 14]. Both a lactogen-dependent increase in biosynthetic 5-HT enzymes (tryptophan hydroxylase [i.e. TPH1 and TPH2]), increasing intra-islet 5-HT [14] or increased 5-HT signalling via the 5-HT receptor 2b (5-HT2B receptor) [6] mediates beta cell proliferation in pregnant rodents. Signalling through the 5-HT2B receptor involves coupling via the Gq-protein and activation of the phospholipase C–inositol triphosphate (IP3)–diacylglycerol (DAG) pathway [9]. Muscarinic (M3) receptors are also known to activate this pathway in islet beta cells, thereby potentiating insulin secretion [2]. Consequently, we explored whether insulin secretion is modulated by targeting the 5-HT2B receptors in human and mouse islets, as well as in INS-1(832/13) cells.
Methods
Human and mouse islets of Langerhans
Human islets were obtained from the Nordic Network for Clinical Islet Transplantation in Uppsala, Sweden and islets were isolated and cultured as previously described [21].
Female NMRI mice (7–10 weeks old) (Taconic, Skensved, Denmark) were housed under a 12 h light–dark cycle and were fed standard chow and water ad libitum prior to islet isolation. Mouse islets were isolated by collagenase digestion and incubated overnight in RPMI1640 (10 mmol/l glucose) (Sigma Aldrich, Stockholm, Sweden) at 37°C and 5% (vol./vol.) CO2 before experiments. The Ethics Committees in Uppsala and Lund/Malmö, Sweden approved the studies.
Cell culture
INS-1(832/13) cells were grown in 10 cm tissue culture dishes (Sarstedt, Landskrona, Sweden) at 37°C and 5% CO2. Cells were passaged every second day using 1 ml 0.05% (wt/vol.) trypsin-EDTA, and cultured in RPMI1640 (11.1 mmol/l d-glucose) (Sigma Aldrich) as previously described and received from H. Mulder (Lund University Diabetes Centre) [22]. The cells were tested mycoplasma free.
Quantitative real-time PCR
mRNA was prepared from human islets and INS-1(832/13) cells (RNA Easy Plus mini kit; Qiagen, Hilden, Germany). cDNA was obtained by reverse transcription (Maxima First Strand cDNA Synthesis Kit; Fermentas, Thermo Scientific, Helsingborg, Sweden). Human HTR2B assay (Hs00265286) and reference genes encoding cyclophilin A (PPIA) (Hs0156700), polymerase 2 (POL2A, also known as TIL1) (Hs00172187) and hypoxanthine guanine phosphoribosyl transferase (HPRT) (Hs02800695) (Life Technologies, Stockholm, Sweden) were run on ABI PRISM 7900 (Applied Biosystems, Foster City, CA, USA). Htr2b expression in INS-1(832/13) cells was detected with fwd primer 69768: ATGAAGCAGACTGCCGAGAA and rev primer 692768: CACCGCCAAGGACATTAGAA using SYBR-Green (Invitrogen, Stockholm, Sweden) and normalised against Ppia (Rn03302269), Pol2a (Rn00585096) and Hprt (Rn01527840) (Invitrogen) on ABI PRISM 7900 (Applied Biosystems). Samples were run in triplicate, and the transcript quantity was normalised with the \( {2}^{{\Delta \mathrm{C}}_{\mathrm{t}}} \) formula.
RNA sequencing
Total RNA was extracted (as above) from human donor islets (n = 50). Islets from each donor were cultured in 5.5 mmol/l and 18.9 mmol/l glucose for 24 h. RNA-seq libraries were generated (TruSeq RNA sample preparation kit; Illumina, San Diego, CA, USA) and sequenced on an Illumina HiSeq 2000, using paired-end chemistry and 100 bp cycles to an average depth of 29 M read pairs per sample. Reads were aligned to the reference transcriptome (hg19) with Bowtie2 (www.genomebiology.com/2009/10/3/R25, www.nature.com/nmeth/journal/v9/n4/full/nmeth.1923.html) and gene expression was estimated as fragments per kilobase of transcript per million mapped reads (FPKM) by the Rsem software (www.ncbi.nlm.nih.gov/pubmed/21816040).
Immunohistochemical analysis
Sections (5 μm) of paraffin-embedded human (n = 5) and mouse (n = 4) pancreases were mounted on slides and air-dried overnight at 37°C. Slides were deparaffinised as previously described [23], and incubated with primary antibodies: goat anti-5-HT2B (sc-15080, 1:50; Santa Cruz Biotech, Dallas, TX, USA), rabbit anti-glucagon (7811, 1:10,000; Euro Diagnostica, Malmö, Sweden) and guinea pig anti-proinsulin (9003, 1:2,500; Euro Diagnostica) overnight at 4°C in moisturising chambers. Slides were rinsed in PBS with Triton X-100 for 2 × 10 min. Secondary antibodies conjugated to Cy2, Texas Red or AMCA were applied [24]. Specificity of immunostaining was tested using primary antisera pre-absorbed with homologous antigen (5-HT2B, sc-15080p; Santa Cruz Biotech, Dallas, TX, USA) (100 μg of peptide/ml antiserum). Immunofluorescence was examined under an epifluorescence microscope (Olympus BX60, Tokyo, Japan). Images were captured with a digital camera (Nikon DS-2Mv, Tokyo, Japan).
Insulin and 5-HT measurements
Non-diabetic human islets (from 34 donors) and mouse islets (from 10 mice) were handpicked under a stereomicroscope. The islets were picked in a randomised fashion with large, small and medium sized islets.
For each individual donor (arriving sporadically), islets were divided into groups of five and for each individual mouse into groups of three in each well of a 96-well plate and pre-incubated for 30 min with secretion assay buffer (in mmol/l: 2.8 glucose, 114 NaCl, 4.7 KCl, 1.2 KH2PO4, 1.16 MgSO4, 25.5 NaHCO3, 20 HEPES, 2.5 CaCl2 and 0.2% (wt. vol) BSA [fatty acid free]). Incubations were performed using 2.8 and 16.7 mmol/l glucose with or without 5-HT2B agonist α-methyl serotonin maleate salt (AMS) (Sigma Aldrich) or Xestospongin C (Tocris, Bristol, UK) in a 96-well plate at 37°C. Each experiment was performed with six to eight replicates for each condition. Insulin was determined after 1 h using Human and Mouse ELISA (Mercodia, Uppsala, Sweden).
INS-1(832/13) cells were seeded on 24-well plates, 24 h before the insulin secretion experiment resulting in ~ 100% confluence. Prior to the experiment, cells were washed in 1 ml secretion assay buffer (see above) followed by 2 h incubation in the same buffer. Cells were stimulated with 2.8 or 16.7 mmol/l glucose with or without 5-HT2B receptor agonists AMS or Ro60-0175 (Sigma Aldrich). Concentrations of AMS and Ro60-0175 were determined from EC50 values [25–27] and based on previous in vitro studies [28, 29]. Insulin was measured with rat ELISA (Mercodia) after 1 h and normalised to total protein (BCA; Pierce Biotechnology, Rockford, IL, USA).
5-HT was measured with a 5-HT ELISA (LDN Labor Diagnostika Nord; Nordhorn, Germany) in INS-1(832/13) cells (n = 3) and islets (islets from four mice) stimulated with 2.8 and 16.7 mmol/l glucose for 1 h (as above).
RNA interference
Small interfering RNA (siRNA) sequences for HTR2B and negative control siRNA (sense: GAGACCCUAUCCGUGAUUATT, anti-sense: UAAUCACGGAUAGGGUCUCTT) (Invitrogen) were used. Cells were transfected with 60 nmol/l siRNA, using Lipofectamine 2000 (Invitrogen). Medium was changed after 24 h and cells were assayed for knock down after 48 h. Alternatively, cells were cultured for 72 h post-transfection and insulin secretion was measured in response to 2.8 and 16.7 mmol/l glucose with or without AMS.
Western blot analysis
INS-1(832/13) cells were lysed (9 mol/l urea, 100 mmol/l HEPES, 1% (vol./vol.) Triton X-100, 0.25% (wt/vol.) IcoPAL-630, 0.25% dodecyl maltoside (wt/vol.), pH 7.2) and protein concentration was estimated (Pierce Biotechnology). Protein (10–30 μg) was loaded onto a 10% Tris-HEPES gel (Pierce Biotechnology) and electrophoresis was performed according to the manufacturer’s protocol. Proteins were then transferred to an Immobilon-FL PVDF-membrane (Millipore, Billerica, MA, USA). Membranes were blocked in blocking buffer (LI-COR, Lincoln, NE, USA) and incubated overnight at 4°C with mouse pAb anti-HTR2b (556334, 1:500; Becton Dickinson, Franklin Lakes, NJ, USA) and β-actin (A5441, 1:5,000; Sigma Aldrich). Application of secondary antibodies and detection were performed as previously described [30].
Calcium imaging
Islets (n = 19 islets from five control mice vs n = 27 from five AMS-treated mice) were attached to CellTak (Corning, New York, NY, USA)-coated glass bottom dishes (MatTek, Ashland, MA, USA) overnight. Fura 2-AM (4 μmol/l) (TEFLabs, Austin, TX, USA) were applied for 40 min followed by 30 min of de-esterification in imaging buffer. Imaging was performed as previously described [31]. One frame per second was recorded at 37°C under perfusion at 0.7 ml/min for 5 min at 2.8 mmol/l glucose, followed by 20 min at 16.7 mmol/l glucose, then 20 min at 2.8 mmol/l glucose with or without AMS. A marked region around each islet and the light intensity was recorded to acquire the mean light intensity at 340 nm (exposure 150 ms) and 380 nm (exposure 100 ms). Intensity measurements were used to calculate the ratio of bound Fura-2 (340 nm) and unbound (380 nm) Ca2+.
Mitochondrial respiration
INS-1(832/13) cells were seeded in 24-well culture microplates (XF24) (Seahorse Bioscience, Billerica, MA, USA) (100,000 cells/well) in 500 μl of RPMI1640 medium. Plates were incubated for 48 h at 37°C in 5% CO2. Prior to assay, the medium was removed and replaced by 750 μl assay medium (in mmol/l: 114 NaCl, 4.7 KCl, 1.2 KH2PO4, 1.16 MgSO4, 20 HEPES, 2.5 CaCl2 and 0.2% (wt/vol.) BSA, pH 7.2) supplemented with 2.8 mmol/l glucose. Oxygen consumption rate (OCR) was determined in 7 μl volume above the plated cells. Respiration was measured in 2.8 mmol/l glucose for 60 min followed by transition to 16.7 mmol/l glucose. Respiration driving ATP synthesis and proton leak were determined by the addition of oligomycin (4 μg/ml). After 30 min, 4 μmol/l of the mitochondrial uncoupler FCCP (carbonyl cyanide-p-trifluoromethoxyphenylhydrazone) was added to determine maximal respiratory capacity. After an additional 10 min, 1 μmol/l rotenone was added to block transfer of electrons from complex I to ubiquinone.
Statistical analysis
All data are presented as means ± SEM. Differences in expression levels and insulin release were analysed with Mann–Whitney U test. RNA sequencing data are presented as relative logarithmic values normalised to total number of reads; p values were determined by a paired t test. The AUC for Ca2+ measurements was analysed using the trapezoidal rule and p values were calculated with Student’s t test. The proportion of islets displaying different Ca2+ profiles was analysed with one-way ANOVA and Tukey’s multiple comparisons test. Statistical testing was performed using Statistical Package for the Social Sciences (SPSS) version 19.0 software (SPSS, Chicago, IL, USA) or GraphPad Prism 6 software (GraphPad Software, La Jolla, CA, USA). Significance for all tests was considered as p < 0.05. Outliers from each experiment were determined by using a Grubb’s outlier test in GraphPad Prism.
Results
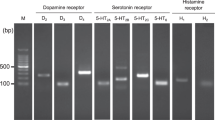
HTR2B RNA expression in INS-1(832/13) cells and human islets
Expression levels of Htr2b in INS-1(832/13) cells increased significantly after 36 h incubation with the 5-HT2B receptor agonist AMS (5 μmol/l) (n = 5, p = 0.002) (Fig. 1a) and the natural ligand 5-HT (10 μmol/l) (n = 3, p = 0.034) (Fig. 1b) compared with untreated cells. Incubation of cells with the 5-HT2B receptor antagonist SB204741 [32] (1 μmol/l) decreased expression of the receptor when compared with untreated cells (Fig. 1c; n = 3, p = 0.0003). Interestingly, in INS-1(832/13) cells incubated in 30 mmol/l glucose, a condition used to examine glucotoxicity, expression of Htr2b was reduced compared with cells grown in cell culture medium (n = 7, p = 0.006) (Fig. 1d). This suggests that expression of Htr2b in INS-1(832/13) cells is regulated by its own activation and inhibition. In addition, expression of HTR2B is negatively regulated by a glucotoxic challenge. In human islets, the expression of HTR2B was not altered in islets from donors with type 2 diabetes compared with those from controls (Fig. 1e [n = 6 non-diabetic and 4 type 2 diabetes islet donors]). However, RNA sequencing in islets (n = 50) collected from non-diabetic humans and incubated for 24 h in 18.9 mmol/l glucose revealed decreased expression of HTR2B when compared with islets cultured in 5.5 mmol/l glucose (p = 0.04). Thus human islets displayed a regulation in response to glucose similar to that shown by the INS-1(832/13) cells.
(a–d) Htr2b expression in INS-1(832/13) cells with or without AMS (a), with or without 5-HT (b), with or without SB204741 (c) and incubated in 11.1 mmol/l glucose (control) and 30 mmol/l glucose (d). (e) HTR2B expression in islets from non-diabetic donors (control) and donors with type 2 diabetes (T2D). (f) RNA sequencing in non-diabetic human islets incubated in 5.5 mmol/l and 18.9 mmol/l glucose. (g, h) Tph1, Tph2 and Ddc expression in INS-1 (832/13) cells (g) and in mouse islets of Langerhans (h). Data are shown as means ± SEM. *p < 0.05, **p < 0.01 and ***p < 0.001 for indicated comparisons
Enzymes required for 5-HT synthesis, tryptophan hydroxy-lase 1 and 2 (encoded by Tph1, Tph2), as well as dopa decarboxylase (encoded by Ddc), were expressed at the mRNA level in both INS-1(832/13) cells (Fig. 1g; n = 3) and mouse islets (Fig. 1h; n = 3 mice). Expression of Htr2a transcripts was found in mRNA preparations from both species, while Htr2c receptor transcripts were not (data not shown).
5-HT2B protein is present in human and mouse beta cells
Next, we investigated the tissue distribution of 5-HT2B receptors in human (n = 5) and mouse (n = 4) pancreas (Fig. 2). 5-HT2B receptors (Fig. 2a) were primarily present in human beta cells (Fig. 2d). In contrast, no 5-HT2B immunofluorescence was observed in alpha cells (Fig. 2d). In mouse islets, a similar pattern was observed, revealing 5-HT2B immunofluorescence in insulin-positive cells (Fig. 2e, f, g). Antibody specificity was verified by lack of staining in human pancreas (Fig. 2h, i) after pre-absorption with homologous antigen.
(a–d) Immunostaining of 5-HT2B (a), glucagon (b) and insulin (c), and overlay (d), in human pancreas. (e–g) Immunostaining of 5-HT2B (e) and insulin (f), and overlay (g), in mouse pancreas. (h, i) Human pancreas with immunostaining of 5-HT2B (h) and 5-HT2B antibody pre-absorbed with blocking peptide (i). Scale bars, 50 μm
Activation of the 5-HT2B receptor augments GSIS
The compound AMS has previously been tested in vitro, ex vivo [29] and in vivo [33] and possesses a 100-fold higher binding selectivity for 5-HT2B receptors compared with 5-HT2A and 5-HT2C receptors [34]. We exposed INS-1(832/13) cells and human and mouse islets to AMS at 2.8, 8.3 or 16.7 mmol/l glucose. In human islets, AMS increased insulin secretion at 8.3 mmol/l glucose (10 μmol/l AMS; n = 13, p = 0.04) and 16.7 mmol/l glucose (5 μmol/l AMS; n = 11, p = 0.03) compared with controls stimulated with glucose alone (n = 34; Fig. 3a). Similarly, a robust stimulation of insulin secretion was observed when mouse islets (n = 10) were treated with 16.7 mmol/l glucose and AMS (10 μmol/l) as compared with glucose alone (p = 0.002) (Fig. 3b). Last, AMS (10 μmol/l) potentiated GSIS in INS-1(832/13) cells (n = 18, p = 0.002) (Fig. 3c). Addition of other secretagogues, such as carbachol (muscarinic activation) or forskolin (cAMP stimulation), in combination with AMS had no additional effect on GSIS from INS-1(832/13) cells (data not shown). To further evaluate the potentiation of GSIS by 5-HT2B receptor activation, we used Ro60-0175 (10 μmol/l), another 5-HT2B receptor agonist. Importantly, this agonist also potentiated GSIS in INS-1 (832/13) cells (n = 6, p = 0.02) (Fig. 3d). 5-HT2B mainly acts on the Gq, phospholipase C, IP3–DAG pathway, so we investigated whether the effects of AMS could be abolished using the IP3 receptor inhibitor Xestospongin C. Indeed, addition of 0.4 μmol/l Xestospongin C reduced the potentiating effect of AMS on GSIS in mouse islets (n = 4, Fig. 3e).
(a) Human islets stimulated with glucose (2.8, 8.3 or 16.7 mmol/l) (white bars) with addition of 5 μmol/l (grey bars) or 10 μmol/l AMS (black bars). (b) Mouse islets stimulated with 2.8 or 16.7 mmol/l glucose (white bars) with addition of 10 μmol/l AMS (black bars). (c) INS-1(832/13) cells stimulated with 2.8 or 16.7 mmol/l glucose (white bars), with addition of 10 μmol/l AMS (black bars). (d) INS-1(832/13) cells stimulated with 2.8 or 16.7 mmol/l glucose (white bars) with addition of 10 μmol/l Ro60-0175 (black bars). (e) Mouse islets incubated with 10 mmol/l glucose (control) with addition of 10 μmol/l AMS, 0.4 μmol/l Xestospongin C (XSP-C) or 10 μmol/l AMS plus 0.4 μmol/l Xestospongin C; all measurements are fold vs basal (2.8 mmol/l glucose). (f, g) 5-HT release from INS-1 (832/13) cells (f) and in mouse islets (g) stimulated with 2.8 or 16.7 mmol/l glucose. Data are means ± SEM. *p < 0.05, **p < 0.01 and ***p < 0.001 for indicated comparisons
5-HT is released from INS-1(832/13) cells and mouse islets
5-HT was released from both INS-1(832/13) cells (n = 3) and mouse (n = 4) islets at 2.8 mmol/l glucose (Fig. 3f, g). No additional increase in 5-HT concentration was observed when subjecting cells/islets to an increased glucose concentration (16.7 and 10 mmol/l, respectively). This suggests that glucose does not regulate release of 5-HT from rodent beta cells; rather, 5-HT leaks from the secretory vesicles as previously described [15].
Silencing 5-HT2B receptors inhibits GSIS
An alternative approach to study the function of the receptor is to reduce its expression in beta cells. RNA interference targeting Htr2b resulted in a 70% knockdown of the receptor at the mRNA level (n = 3, p = 0.001) (Fig. 4a) and a 30% reduction at the protein level (n = 4, p = 0.002) (Fig. 4b, c). GSIS was significantly reduced as compared with controls (n = 10, p = 0.001) (Fig. 4d) after exposing siRNA-treated cells to 2.8 vs 16.7 mmol/l glucose. Next, we stimulated Htr2b siRNA-treated cells with AMS at 16.7 mmol/l glucose. In contrast to control cells, no potentiation of GSIS was observed (Fig. 4d). This implies that the agonist has high selectivity for the 5-HT2B receptor and stimulates insulin secretion via this receptor.
(a, b) Expression of Htr2b (a) and ratio of 5-HT2B protein (b) in INS-1(832/13) negative control (NC) cells and after knockdown (KD). (c) Representative western blot with 5-HT2B protein in untreated control INS-1(832/13) cells (C) and in NC cells and after KD, with protein ladder (L) shown. (d) INS-1(832/13) cells stimulated with 2.8 mmol/l and 16.7 mmol/l glucose (white bars), post KD (grey bars) and stimulated with AMS (10 μmol/l) (black bars). Data are means ± SEM. *p < 0.05 and **p < 0.01 for indicated comparisons
5-HT2B receptor activation alters islet Ca2+ profiles
Intracellular Ca2+ levels in mouse islets generally display distinct first-phase oscillations in response to elevated glucose concentrations. This is followed by a second-phase train of oscillations of lower amplitude and intensity (Fig. 5a). A striking increase (threefold, p = 6.02 × 10−6) in peak duration (time in s that the peak is in a plateau phase or active phase) was observed in mouse islets treated with AMS (10 μmol/l) as compared with control islets treated with glucose alone (Fig. 6a). Moreover, a significant increase in the distance between Ca2+ peaks or period (peak-to-peak distance in ms) was observed in AMS-treated islets compared with controls (p = 0.015) (Fig. 6b). This suggests that 5-HT2B activation amplifies the effects of glucose on intracellular Ca2+. In fact, 11% of the AMS-treated islets displayed this distinct profile of strong regular Ca2+ bursts; this was never observed in control experiments (11% vs 0%) (Fig. 5b and Table 1). As a consequence of increased distance between peaks and peak duration the frequency of oscillations in the second phase was reduced by 43% in AMS-treated islets (2.95 vs 1.69 oscillations/min, p = 0.027; Fig. 6c), as well as the difference in the ratio between first-phase and second-phase oscillations (see variable C3P, ratio C1/C4M) (Fig. 6d and Table 2; p = 0.03).
(a) First-phase Ca2+ oscillation in response to 16.7 mmol/l glucose followed by second-phase oscillations in untreated mouse islets. Explanations for the letters C1, C2 etc. are presented in Table 2. (b) When treated with 10 μmol/l AMS, 11% of the islets had a distinct Ca2+ profile in response to 16.7 mmol/l glucose. (c) AMS-treated islets with an extended first phase, followed by a distinct Ca2+ profile. (d) In the total experimental set-up 20% of islets displayed no clear first phase. (i), First-phase area under graph during first 2 min; (ii), second-phase frequency of oscillations and area under graph measured during last 10 min interval
(a) Peak duration of Ca2+ traces in control and AMS-treated mouse islets. (b) Distance between Ca2+ peaks in control and AMS-treated mouse islets. (c) Frequency of second-phase oscillations in control and AMS-treated mouse islets. (d) First-phase and second-phase ratio (C1/C4M) in control and AMS-treated mouse islets. Data are means ± SEM. *p < 0.05 and ****p < 0.0001 for indicated comparisons
The area of the Ca2+ dip prior to the initial Ca2+ burst, which likely represents Ca2+ uptake into endoplasmic reticulum stores, was also measured (see variable Ad Fig. 5a, Table 2). Although a 23% reduction in Ca2+ was observed in AMS-treated islets, reflecting increased cytoplasmic Ca2+, this did not reach statistical significance (Table 2).
Roughly half of control (58%) and AMS-treated islets (44%) displayed an extended first phase (Fig. 5c and Table 1), while 20% of all islets in the experimental set-up displayed no clear first phase (Fig. 5d and Table 1). This suggests a heterogeneity in Ca2+ responses that typically is observed in islets. The number of imaged islets was: n = 19 control islets from 5 mice vs n = 27 AMS-treated islets from 5 mice.
5-HT2B receptor activation enhances mitochondrial metabolism
As AMS potentiated GSIS in islets/cells and since alterations in Ca2+ flux are suggested to influence activation of mitochondrial enzymes [35], we investigated whether these events were associated with changes in mitochondrial metabolism. INS-1(832/13) cells were stimulated with glucose with or without the addition of AMS and oxygen consumption was determined. OCR increased under both conditions, but cells treated with AMS exhibited a greater glucose-induced increase in respiration (Fig. 7a, b, p = 0.05). Maximum mitochondrial respiratory rate increased in AMS-treated cells (Fig. 7c, p = 0.007), and this was further confirmed when analysing the apex of maximum respiratory capacity (Fig. 7d, p = 0.017). A significant increase in spare respiratory capacity was observed in AMS-stimulated cells compared with controls (Fig. 7e, p = 0.04). These data suggest that AMS treatment enhances beta cell respiratory capacity. Neither difference in proton leak nor in coupling efficiency was observed between the two treatments (data not shown).
(a) INS-1(832/13) cells stimulated with 2.8 (at baseline) and 16.7 mmol/l glucose either with (black circles) or without (white circles) AMS. AMS was added at the same time as additional glucose (indicated by the arrow); oligomycin, FCCP and rotenone were added to both groups as shown. (b) INS-1(832/13) cells stimulated with 16.7 mmol/l glucose without (untreated) or with addition of AMS. (c) Maximal respiration point in cells without (untreated) or with AMS. (d) Maximal respiration rate without (untreated) or with AMS. (e) Spare respiratory capacity in cells stimulated without (untreated) or with AMS. Data are means ± SEM (n = 8). *p < 0.05 and **p < 0.01 for indicated comparisons
Discussion
In the present study, we explored the regulatory role of 5-HT2B receptor activation on GSIS. We show that pharmacological activation of 5-HT2B receptors, with two different agonists (AMS and Ro60-0175), potentiates GSIS in human and mouse islets and in INS-1 (832/13) cells. Moreover, a reduction in Htr2b mRNA expression in INS-1(832/13) reduced GSIS by nearly 30%. Together, these findings support the functional importance of this receptor in control of GSIS. This function can be further understood in light of the cellular expression of 5-HT2B receptors, which was localised to islet beta cells in human and mouse islets.
Limited information exists regarding the effects of 5-HT2B signalling on beta cell function. A previous report shows that tamoxifen-induced beta cell-specific knockout of 5htr2b results in mice remaining normoglycaemic during an intraperitoneal glucose tolerance test when challenged by a high-fat diet in vivo [36]. Such results infer that 5-HT2B is unimportant for islet function. We performed acute manipulations of 5-HT2B signalling, using agonists and gene silencing, which could be considered a weakness when opposed to in vivo studies. However, in a chronic experimental situation the known redundancy of 5-HT receptors can become more prominent in an in vivo situation. To this end, no studies have explored in vitro beta cell function in islets isolated from Htr2b beta cell-specific knockout mice. This enhances the novelty of the present findings.
A recent study suggests that an additional member of the 5-HT2 family (5-HT2C) is increased in islets from diabetic db/db mice and in palmitate-treated MIN-6 cells [37], and that this results in reduced GSIS. Here, we were unable to detect the transcript of 5-HT2C in either human or mouse islets.
Most studies suggest that 5-HT inhibits insulin secretion [11, 15, 17, 18]. Clinically, 5-HT systems in the central nervous system are targeted by antidepressants and long-term use of antidepressants is associated with an increased type 2 diabetes risk [38, 39]. Since beta cells express multiple 5-HT receptors [10, 11] and the serotonin transporter (SERT) [40], direct effects on insulin secretion are likely. Indeed, selective serotonin re-uptake inhibitors (SSRIs) inhibit insulin secretion in clonal beta cells [41, 42], possibly through an increased 5-HT concentration in the extracellular space. We observed positive effects of acute exposure of 5-HT2B receptor agonists on GSIS. Notably, we show that IP3 receptor inhibition reversed the effects of AMS on insulin secretion, suggesting that the effect on GSIS is partly mediated by an increase in intracellular Ca2+. This is to some extent corroborated by our findings since we observed a 23% reduction in Ca2+ uptake in the endoplasmic reticulum in AMS-treated islets. We also show a significant increase in peak duration (plateau of peak) and distance between peaks (period), which suggest that islets spend more time in an active phase and the period between peaks are prolonged. Similar Ca2+ patterns are observed when glucose is raised from an intermediary concentration to a high concentration that causes a regimen change in Ca2+ oscillation from fast to slow oscillations with greater amplitude and increased plateau phase [43]. Thus, 5-HT2B receptor activation appears to amplify the effects of glucose on intracellular Ca2+. In agreement with previous studies [44, 45] we also found that islet beta cells represent a heterogeneous population. In this case, this could be accounted for by findings indicating that 5-HT, and possibly 5-HT receptor expression, is confined to a subset of beta cells [14].
Changes in intracellular Ca2+ may also affect mitochondrial metabolism via activation of dehydrogenases operating in the tricarboxylic acid cycle [35]. Alterations in Ca2+ oscillations, caused by 5-HT2B receptor activation, may amplify the production of metabolic coupling factors during GSIS [46]. In fact, INS-1(832/13) cells stimulated with glucose and AMS displayed an increase in glucose-stimulated oxygen consumption, indicating enhanced mitochondrial activity. We also observed an increased spare respiratory capacity, suggesting that 5-HT2B receptor activation is involved in priming cells to meet an increased metabolic demand. This agrees with previous data, suggesting that signalling through 5-HT2B receptors in pregnant rodent beta cells is involved in proliferation, an energy-demanding process [6]. Interestingly, treatment with the selective serotonin re-uptake inhibitor fluoxetine disturbs mitochondrial respiration by increasing the formation of reactive oxygen species [42]. Thus, 5-HT overload may have detrimental effects on beta cell function, while physiological 5-HT levels or activation of specific 5-HT receptors may serve an enhancing role.
Information on individual effects of 5-HT receptors on GSIS in vitro is limited. We recently showed that HTR1D and HTR2A are overexpressed in islets from individuals with type 2 diabetes as compared with islets from non-diabetic individuals. The amine 5-HT and activation of 5-HT1D receptors in non-diabetic human islets inhibits GSIS while activation of 5-HT2A receptors potentiates GSIS. Interestingly, islets from donors with type 2 diabetes lose the inhibitory effect of 5-HT on GSIS, suggesting that alterations in 5-HT production or 5-HT receptor expression may contribute to beta cell dysfunction [11].
5-HT3 receptors are implicated in compensatory increase in insulin secretion during pregnancy [8] and global Htr3a knockout mice on a high-fat diet display a defective first-phase insulin release in vitro [36]. Additionally, beta cell-specific Tph1-knockout mice fed a high-fat diet become increasingly glucose intolerant in vivo, exhibiting an insulin secretory defect in vitro, suggesting that basal 5-HT production in beta cells is essential in GSIS. Importantly, we show that mouse islets and INS-1(832/13) cells harbour the enzymes necessary for 5-HT synthesis and that low amounts of 5-HT are released from INS-1(832/13) cells and mouse islets.
Currently, the incidence of type 2 diabetes is increasing worldwide and there is an urgent need to develop novel therapeutic strategies that improve beta cell function. In sum, we provide novel data on localisation, function and signalling events caused by activation of 5-HT2B receptors in beta cells in three different species. This information could be further explored to provide a drug target for type 2 diabetes treatment.
Abbreviations
- AMS:
-
α-Methyl serotonin maleate salt
- DAG:
-
Diacylglycerol
- GLP-1:
-
Glucagon-like peptide 1
- GSIS:
-
Glucose-stimulated insulin secretion
- 5-HT:
-
5-Hydroxytryptamine; serotonin
- IP3:
-
Inositol triphosphate
- OCR:
-
Oxygen consumption rate
- siRNA:
-
Small interfering RNA
References
Holst JJ, Gromada J (2004) Role of incretin hormones in the regulation of insulin secretion in diabetic and nondiabetic humans. Am J Physiol Endocrinol Metab 287:E199–E206
Rodriguez-Diaz R, Dando R, Jacques-Silva MC et al (2011) Alpha cells secrete acetylcholine as a non-neuronal paracrine signal priming beta cell function in humans. Nat Med 17:888–892
Rosengren AH, Jokubka R, Tojjar D et al (2010) Overexpression of alpha2A-adrenergic receptors contributes to type 2 diabetes. Science 327:217–220
Aaboe K, Krarup T, Madsbad S, Holst JJ (2008) GLP-1: physiological effects and potential therapeutic applications. Diabetes Obes Metab 10:994–1003
Drucker DJ (2015) Deciphering metabolic messages from the gut drives therapeutic innovation: the 2014 Banting Lecture. Diabetes 64:317–326
Kim H, Toyofuku Y, Lynn FC et al (2010) Serotonin regulates pancreatic beta cell mass during pregnancy. Nat Med 16:804–808
Kirchgessner AL, Liu MT, Raymond JR, Gershon MD (1996) Identification of cells that express 5-hydroxytryptamine1A receptors in the nervous systems of the bowel and pancreas. J Comp Neurol 364:439–455
Ohara-Imaizumi M, Kim H, Yoshida M et al (2013) Serotonin regulates glucose-stimulated insulin secretion from pancreatic beta cells during pregnancy. Proc Natl Acad Sci U S A 110:19420–19425
Nichols C, Sanders-Bush E (2001) Serotonin receptor signaling and hallucinogenic drug action. Heffer Rev Psychadelic Res 2:73–79
Amisten S, Salehi A, Rorsman P, Jones PM, Persaud SJ (2013) An atlas and functional analysis of G-protein coupled receptors in human islets of Langerhans. Pharmacol Ther 139:359–391
Bennet H, Balhuizen A, Medina A et al (2015) Altered serotonin (5-HT) 1D and 2A receptor expression may contribute to defective insulin and glucagon secretion in human type 2 diabetes. Peptides 71:113–120
Sundler F, Hakanson R, Loren I, Lundquist I (1980) Amine storage and function in peptide hormone-producing cells. Invest Cell Pathol 3:87–103
Aspinwall CA, Huang L, Lakey JR, Kennedy RT (1999) Comparison of amperometric methods for detection of exocytosis from single pancreatic β-cells of different species. Anal Chem 71:5551–5556
Schraenen A, Lemaire K, de Faudeur G et al (2010) Placental lactogens induce serotonin biosynthesis in a subset of mouse beta cells during pregnancy. Diabetologia 53:2589–2599
Gylfe E (1978) Association between 5-hydroxytryptamine release and insulin secretion. J Endocrinol 78:239–248
Smith PA, Proks P, Ashcroft FM (1999) Quantal analysis of 5-hydroxytryptamine release from mouse pancreatic β-cells. J Physiol 521:651–664
Zawalich WS, Tesz GJ, Zawalich KC (2004) Effects of prior 5-hydroxytryptamine exposure on rat islet insulin secretory and phospholipase C responses. Endocrine 23:11–16
Lernmark A (1971) The significance of 5-hydroxytryptamine for insulin secretion in the mouse. Horm Metab Res 3:305–309
Peschke E, Peschke D, Hammer T, Csernus V (1997) Influence of melatonin and serotonin on glucose-stimulated insulin release from perifused rat pancreatic islets in vitro. J Pineal Res 23:156–163
Paulmann N, Grohmann M, Voigt JP et al (2009) Intracellular serotonin modulates insulin secretion from pancreatic beta-cells by protein serotonylation. PLoS Biol 7:e1000229
Hutton JC (1989) The insulin secretory granule. Diabetologia 32:271–281
Hohmeier HE, Mulder H, Chen G, Henkel-Rieger R, Prentki M, Newgard CB (2000) Isolation of INS-1-derived cell lines with robust ATP-sensitive K+ channel-dependent and -independent glucose-stimulated insulin secretion. Diabetes 49:424–430
Landerholm K, Falkmer SE, Jarhult J, Sundler F, Wierup N (2011) Cocaine- and amphetamine-regulated transcript in neuroendocrine tumors. Neuroendocrinology 94:228–236
Asad S, Nikamo P, Gyllenberg A et al (2012) HTR1A a novel type 1 diabetes susceptibility gene on chromosome 5p13-q13. PLoS One 7:e35439
Cussac D, Newman-Tancredi A, Quentric Y et al (2002) Characterization of phospholipase C activity at h5-HT2C compared with h5-HT2B receptors: influence of novel ligands upon membrane-bound levels of [3H]phosphatidylinositols. Naunyn Schmiedeberg’s Arch Pharmacol 365:242–252
Porter RH, Benwell KR, Lamb H et al (1999) Functional characterization of agonists at recombinant human 5-HT2A, 5-HT2B and 5-HT2C receptors in CHO-K1 cells. Br J Pharmacol 128:13–20
Elliott P, Wallis DI (1992) Serotonin and L-norepinephrine as mediators of altered excitability in neonatal rat motoneurons studied in vitro. Neuroscience 47:533–544
Campos-Bedolla P, Vargas MH, Calixto E et al (2006) α-Methyl-5-HT, a 5-HT2 receptor agonist, stimulates β2-adrenoceptors in guinea pig airway smooth muscle. Pharmacol Res 54:468–473
Gorini C, Jameson HS, Mendelowitz D (2009) Serotonergic modulation of the trigeminocardiac reflex neurotransmission to cardiac vagal neurons in the nucleus ambiguus. J Neurophysiol 102:1443–1450
Kumar R, Balhuizen A, Amisten S, Lundquist I, Salehi A (2011) Insulinotropic and antidiabetic effects of 17β-estradiol and the GPR30 agonist G-1 on human pancreatic islets. Endocrinology 152:2568–2579
Christensen GL, Jacobsen ML, Wendt A et al (2015) Bone morphogenetic protein 4 inhibits insulin secretion from rodent beta cells through regulation of calbindin1 expression and reduced voltage-dependent calcium currents. Diabetologia 58:1282–1290
Ebrahimkhani MR, Oakley F, Murphy LB et al (2011) Stimulating healthy tissue regeneration by targeting the 5-HT2B receptor in chronic liver disease. Nat Med 17:1668–1673
Chaouloff F, Jeanrenaud B (1987) 5-HT1A and α-2 adrenergic receptors mediate the hyperglycemic and hypoinsulinemic effects of 8-hydroxy-2-(di-n-propylamino)tetralin in the conscious rat. J Pharmacol Exp Ther 243:1159–1166
Baxter GS (1996) Novel discriminatory ligands for 5-HT2B receptors. Behav Brain Res 73:149–152
Duchen MR (1999) Contributions of mitochondria to animal physiology: from homeostatic sensor to calcium signalling and cell death. J Physiol 516:1–17
Kim K, Oh CM, Ohara-Imaizumi M et al (2015) Functional role of serotonin in insulin secretion in a diet-induced insulin-resistant state. Endocrinology 156:444–452
Maechler P, Wollheim CB (2000) Mitochondrial signals in glucose-stimulated insulin secretion in the beta cell. J Physiol 529(Pt 1):49–56
Raeder MB, Bjelland I, Emil Vollset S, Steen VM (2006) Obesity, dyslipidemia, and diabetes with selective serotonin reuptake inhibitors: the Hordaland Health Study. J Clin Psychiatry 67:1974–1982
Brown LC, Majumdar SR, Johnson JA (2008) Type of antidepressant therapy and risk of type 2 diabetes in people with depression. Diabetes Res Clin Pract 79:61–67
Ohta Y, Kosaka Y, Kishimoto N et al (2011) Convergence of the insulin and serotonin programs in the pancreatic β-cell. Diabetes 60:3208–3216
Isaac R, Boura-Halfon S, Gurevitch D, Shainskaya A, Levkovitz Y, Zick Y (2013) Selective serotonin reuptake inhibitors (SSRIs) inhibit insulin secretion and action in pancreatic beta cells. J Biol Chem 288:5682–5693
De Long NE, Hyslop JR, Raha S, Hardy DB, Holloway AC (2014) Fluoxetine-induced pancreatic beta cell dysfunction: new insight into the benefits of folic acid in the treatment of depression. J Affect Disord 166:6–13
Nunemaker CS, Bertram R, Sherman A, Tsaneva-Atanasova K, Daniel CR, Satin LS (2006) Glucose modulates [Ca2+]i oscillations in pancreatic islets via ionic and glycolytic mechanisms. Biophys J 91:2082–2096
Van Schravendijk CF, Kiekens R, Pipeleers DG (1992) Pancreatic beta cell heterogeneity in glucose-induced insulin secretion. J Biol Chem 267:21344–21348
Benninger RK, Hutchens T, Head WS et al (2014) Intrinsic islet heterogeneity and gap junction coupling determine spatiotemporal Ca2+ wave dynamics. Biophys J 107:2723–2733
Wiederkehr A, Wollheim CB (2008) Impact of mitochondrial calcium on the coupling of metabolism to insulin secretion in the pancreatic β-cell. Cell Calcium 44:64–76
Acknowledgements
We acknowledge the Human tissue laboratory at Lund University Diabetes Centre, Lund, Clinical Research Centre, Malmö, Sweden and the islet isolation unit, Nordic Network for Clinical transplantation at Uppsala University, Uppsala, Sweden, for providing donor islet material and Sciblu genomics at Lund University, Lund, Sweden. We thank L. Faxius (Unit for Diabetes and Celiac Disease, Department of Clinical Science, Lund University Diabetes Centre, Malmö, Sweden) for excellent technical assistance. H. Mulder (Department of Clinical Science, Lund University Diabetes Centre, Malmö, Sweden) is acknowledged for constructive feedback on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the Swedish Research Council (project number: 2012-1552 to MF), Excellence in diabetes research (EXODIAB), the Krapperup foundation, the Åke Wiberg foundation, the Royal Physiographic Society, the Albert Påhlsson foundation, the Crafoord foundation, the Childhood Diabetes Foundation and the Foundation of Sigurd and Elsa Golijes Minne.
Duality of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Contribution statement
The study was designed by MF. Data acquisition and analysis and RNA isolation for RNA sequencing of human islets incubated in high vs low glucose was performed by EOL, PV and JF. Data acquisition and analysis and interpretation of Ca2+ measurements were performed by IGM, HB, MF and LE. Experimental set-up, analysis and interpretation of mitochondrial respiration were performed by HB, ABagge and MF. All other data analysis and experiments were performed by HB, AM, CN, MDN, ABalhuizen, NW, IA and MF. The manuscript was drafted by HB, IA and MF and all authors were involved in critical revision and approved the final version of the manuscript before submission. MF is the guarantor of this work.
Rights and permissions
About this article
Cite this article
Bennet, H., Mollet, I.G., Balhuizen, A. et al. Serotonin (5-HT) receptor 2b activation augments glucose-stimulated insulin secretion in human and mouse islets of Langerhans. Diabetologia 59, 744–754 (2016). https://doi.org/10.1007/s00125-015-3847-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3847-6