Abstract
Aims/hypothesis
In patients with type 2 diabetes mellitus, the effects of HbA1c variability on macrovascular events remain uncertain. The present investigation evaluates the association of HbA1c variability with non-fatal cardiovascular events, emergency admissions and episodes of severe hypoglycaemia in a cohort of patients newly started on insulin therapy.
Methods
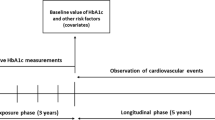
HbA1c variability was defined as the rate of change in values between observations. The medical records of 406,356 patients enrolled in a disease management programme for type 2 diabetes mellitus were analysed to identify a cohort of 13,777 patients with observed transition to insulin therapy. The cohort was observed for a period of at least 5 years. Cox regression models were applied to quantify the association of HbA1c variability with the events of interest.
Results
The models reveal a significant non-linear association between HbA1c variability and the risk of experiencing myocardial infarction, stroke and hypoglycaemia. The lowest risk is seen with a variability of approximately 0.5% (5.5 mmol/mol) per quarter. Using Cox models to predict survival curves for the cohort with hypothetical HbA1c variability of 0.5% (5.5 mmol/mol) and 1.5% (16.4 mmol/mol) per quarter, the proportion experiencing myocardial infarction within 2 years increases significantly from 1% to 10%. The proportion experiencing stroke increases from 1% to 29%, hypoglycaemia from 2% to 24% and the risk of emergency admission from 2% to 21%.
Conclusions/interpretation
In patients newly started on insulin therapy, rapid and higher HbA1c variability is associated with an increased risk of myocardial infarction, stroke, severe hypoglycaemia and emergency admission.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus is a condition highly prevalent around the world. The impact of the associated micro- and macrovascular diseases such as chronic renal disease, diabetic retinopathy, coronary artery disease and peripheral artery disease means that this chronic disease both affects the quality of life and places a burden on healthcare systems and national economies [1, 2]. In the treatment of diabetes, the HbA1c has proven to be a valid indicator of long-term glycaemic status and adequacy of a treatment. Its level is associated with the degree of micro- and macrovascular damage in the organism, and this has led to its use as one of the main laboratory variables in diabetes therapy [3, 4].
Various studies have demonstrated that HbA1c variability is also an independent risk factor for micro- and macrovascular complications [5–10]. Yang et al demonstrated an association of HbA1c variability with subclinical coronary atherosclerosis and also that HbA1c variability is a stronger predictor of premature coronary damage than mean HbA1c in patients with diabetes duration less than 10 years [11]. A recent observational study identified that HbA1c variability is associated with mortality independent of the baseline HbA1c level [12]. Conversely, a cross-sectional analysis within the Italian Renal Insufficiency And Cardiovascular Events (RIACE) multicentre study showed no impact of HbA1c variability on macrovascular outcomes [13]. Previous studies investigated more often the associations between HbA1c variability and microvascular complications than macrovascular outcomes [14]. The possible risks of HbA1c variability in different subgroups are still not well understood and are intensively discussed. This discussion has even cast doubt on previous findings, suggesting possible statistical bias in the methods [15, 16]. There remains, therefore, some uncertainty as to the importance of HbA1c variability as a concept distinct from either the absolute HbA1c value or from a one-off rapid decrease to a target value. To date, most studies have expressed HbA1c variability based on the standard deviation of all HbA1c measurements [5–11, 13, 14].
The present study focuses on patients receiving first-time insulin treatment, which is very effective in lowering average glucose levels in an already high-risk population. We analysed routine data collected to monitor the Bavarian Disease Management Program (DMP) for patients with type 2 diabetes mellitus, which was introduced in 2003 to improve the quality of diabetes care. We hypothesise a positive correlation between high HbA1c variability and the incidence of non-fatal cardiovascular outcomes (myocardial infarction and stroke), episodes of severe hypoglycaemia and emergency admissions. HbA1c variability was assessed using a novel measure that demonstrates a different conceptual approach and thus complements previous work.
Methods
Cohort analysis
Pseudonymised patient medical records were analysed by the Association of Statutory Health Insurance Physicians of Bavaria (Kassenärztliche Vereinigung Bayerns [KVB]). The records were collected for the primary purpose of quality assurance within a DMP for patients with type 2 diabetes mellitus and contain relevant medical information such as the current HbA1c value, comorbidities and process variables. Coordinating general practitioners submit the records on a quarterly or half-yearly basis and receive remuneration for each record, regardless of the perceived quality of care. Data were available for the period October 2003 to December 2013.
To benefit from the more detailed baseline information collected prior to July 2008, patients were excluded if they were enrolled after this point. This yielded 406,356 patients with type 2 diabetes mellitus, of whom 148,132 patients had a record of insulin therapy. From this group, 16,806 patients had a documented transition to insulin therapy prior to July 2008, with an insulin-free baseline record encompassing at least 6 months to enable a valid baseline assessment. The baseline was determined in the 6 month period prior to the first record of insulin treatment. Patients were excluded as implausible or untypical if the baseline HbA1c was less than 6.5% or if the baseline HbA1c was less than 7.5% and no additional oral glucose-lowering therapy was recorded at baseline. This resulted in a coherent cohort of 13,777 patients.
The outcomes were recorded by the coordinating DMP physician in the consultation following the event. Mortality data were therefore not available. Myocardial infarction and stroke were defined as the new occurrence of these events according to medical standards. Severe hypoglycaemia was defined as hypoglycaemia that required medical attention. Emergency admission was defined as unplanned hospitalisation due to diabetic complications. The observation period was the time between the first record of insulin and either the end of follow-up or the record before the first event being analysed. For each outcome individually, patients were excluded if they had experienced the event of interest during the baseline period. Due to interval censoring, it was also necessary to exclude patients with an event recorded simultaneously with the first record of insulin. In such cases, it was unclear whether the event occurred before or after the transition to insulin.
In the context of the DMP record, missing data occur when no record is available, when an optional field is not filled in or when the information contained in the record changes. This has three main implications for the present study. First, sex was not recorded prior to July 2008. Patients without a recorded sex were therefore assigned to a third ‘missing’ category (alternative strategies of multiple imputation and the exclusion of these patients resulted in only marginal changes to the estimated effects of HbA1c variability). Second, serum creatinine is an optional attribute, available at baseline for at most 90% of patients. The binary indicator ‘diabetic nephropathy’ was therefore used as the sole indicator of kidney function. Third, for patients temporarily dropping out of the DMP or having widely spaced records, information regarding HbA1c and outcomes may be incomplete. The chosen method and study design were selected to account, as far as possible, for such data collection issues.
The study was approved by the Medical Ethics Committee of the University Hospital Klinikum rechts der Isar in Munich, Germany.
Approach to calculating HbA1c variability
The present study defined HbA1c variability using the difference between successive measurements. These differences are scaled according to the time between measurements to obtain a series of values representing the rate of change in HbA1c for the time between records. Therefore, the average rate of change in HbA1c is a more detailed description of the present methodological approach to investigate HbA1c variability. A value of 1 thus implies a rate of increase of 1 percentage point in HbA1c per quarter, and a decrease of 1 percentage point (10.9 mmol/mol) over one quarter is considered equivalent to a decrease of 2 percentage points (21.9 mmol/mol) over two quarters. The DMP requires that physicians provide a patient record with HbA1c every quarter or half year, although in practice regular measurements cannot be guaranteed. Differences were therefore discarded as unreliable observations of the true variability if the time between measurements was less than 1 week or greater than 6 months, or if the average change in HbA1c was greater than 3 percentage points (32.8 mmol/mol) per quarter. Similar to previous studies [6, 10, 12, 13], the variability during the observation period was reduced to a single, directionless constant to facilitate interpretation. Whereas other studies used the standard deviation of all HbA1c values (HbA1c-SD), the present study used the mean of the absolute HbA1c differences as described above. An alternative approach, modelling the individual differences in the framework of a time-varying covariates model, is presented in electronic supplementary material (ESM) 1.
Statistical analysis
For each outcome separately, Cox proportional hazards models were used to assess the increase in risk due to HbA1c variability. The models controlled for the following potentially confounding baseline variables: age; sex; smoking status; absolute HbA1c value at baseline; diabetes history of more than 8 years (i.e. the median duration at baseline); cardiovascular disease; peripheral artery disease; the presence of diabetic complications (retinopathy, neuropathy or nephropathy); and record of previous myocardial infarction, stroke or diabetes-related emergency admission. It was not possible to control for severe hypoglycaemia prior to baseline because the small number of cases presents numerical problems. Non-linear effects were estimated by means of penalised splines and displayed graphically. To help assess the validity of the model, the proportional hazards assumption was tested using the cox.zph function in R [17].
The clinical relevance of the non-linear partial hazard ratios estimated by the Cox regression models is not readily apparent. For this reason, the models were used to predict adjusted survival curves for the cohort while fixing the hypothetical HbA1c variability of each patient to ‘low’ (0.5% [5.5 mmol/mol]), ‘increased’ (1% [10.9 mmol/mol]) and ‘high’ (1.5% [16.4 mmol/mol]) levels, respectively. This classification resulted from the findings displayed in Fig. 1. Confidence intervals were estimated by means of 100 bootstrap samples [18, 19]. The model-based adjusted survival curves were compared with the unadjusted Kaplan–Meier estimates generated using the actual data (i.e. without setting HbA1c variability). The analysis was conducted using the R environment for statistical computing, together with the survival package for estimation of the Cox regression models [20].
Results
Table 1 summarises the baseline characteristics. Patients with volatile HbA1c, variability between 0.5% and 3% per quarter (5.5–32.8 mmol/mol), had higher baseline HbA1c levels than patients with the lowest mean HbA1c variability 0–0.49% (0–5.4 mmol/mol). They were also more likely to be male and to smoke. Additionally, the groups with higher HbA1c variability had a higher percentage of previous stroke, myocardial infarction, peripheral artery disease, renal insufficiency and emergency admission. No large group differences were found regarding kidney function (measured by mean estimated GFR [eGFR]), blood pressure, or therapy with oral glucose-lowering medication in general or in the use of metformin. The final column summarises patients for whom the available HbA1c measurements were insufficient to assess variability as described above (e.g. measurements too widely spaced). For the distribution of follow-up and event times, see ESM 2.
Figure 1 displays the non-linear effect of mean HbA1c variability as estimated by the Cox regression models. The plots reveal a clear non-linear effect of HbA1c variability on the risk of experiencing myocardial infarction, stroke, hypoglycaemia and emergency admission. For the first three outcomes, the lowest risk was seen with a variability of approximately 0.5% (5.5 mmol/mol) per quarter, increasing both for patients with lower recorded variation and those with higher variation. For emergency admissions, the effect was approximately linear, with variability lower than 0.5% (5.5 mmol/mol) leading to a decreased risk. The proportional hazards assumption could be confirmed for the outcomes myocardial infarction (p = 0.85) and stroke (p = 0.25), but not for the outcomes of severe hypoglycaemia and emergency admission (p = 0.00). This may indicate that the latter outcomes present a more complex picture, although the results obtained are consistent with those of alternative models that do pass the proportional hazards test (e.g. linear predictor for HbA1c variability). ESM 1 shows an alternative model using time-varying covariables that further differentiate between positive and negative fluctuations, which together were experienced by 97% of participants.
Table 2 and Fig. 2 present the results from the adjusted survival curves generated by the Cox regression models. If all patients had a mean HbA1c variability of 0.5% (5.5 mmol/mol), the models predict 5 year incidences (i.e. 100% minus the proportion without event after 5 years) of 3% for myocardial infarction and 5% each for stroke, severe hypoglycaemia and emergency admission. These predictions are comparable with the estimates obtained using the actual data, reflecting the fact that the distribution of average HbA1c variability is centred around 0.5% (5.5 mmol/mol) and that fewer than 5% of all patients had a variability greater than 1% (10.9 mmol/mol). If all patients are imputed a variability of 1% (10.9 mmol/mol), the 5 year incidences are increased substantially to 6% for myocardial infarction, 15% for stroke, 14% for severe hypoglycaemia and 15% for emergency admission. If all patients are assigned a variability of 1.5% (16.4 mmol/mol), the 5 year incidences are 21% for myocardial infarction, 46% for stroke, 45% for severe hypoglycaemia and 45% for emergency admission. Confidence intervals are presented in Table 2 and demonstrate that the effects are statistically significant.
Adjusted survival curves for the four outcomes as predicted by the fitted Cox regression models. The dashed lines represent the prediction after assigning each patient in the cohort an average HbA1c variability of 0.5% (5.5 mmol/mol) per quarter. The dotted–dashed lines represent the prediction with an average variability of 1% (10.9 mmol/mol) per quarter and the solid lines represent the prediction with 1.5% (16.4 mmol/mol) per quarter. The shaded areas represent 95% CIs
Discussion
To our knowledge, the present study is the first study to evaluate the occurrence of adverse cardiovascular effects with respect to HbA1c variability in the clinically important setting of insulin therapy initiation. The data describe a broad population of primary care patients, thus providing a relatively unbiased account of actual care. We proposed and applied a novel approach to investigate long-term HbA1c variability. Our findings emphasise a strong correlation between the HbA1c variability from initiation of insulin treatment in a previously insulin-naive patient and the adverse outcomes investigated. After adjusting for confounding factors we found that a higher average HbA1c variability was significantly associated with myocardial infarction, stroke, severe hypoglycaemic episodes and emergency admissions. Such volatility results from a fluctuation in both directions over a series of measurements. Variability is therefore an indication of unstable glucose control and can also be a marker of therapy adherence and patient compliance [21]. The exact pathophysiological mechanisms of this finding remain unclear [22–27]. Recently, several studies have shown correlations between microvascular outcomes and HbA1c variability, both in type 1 diabetes mellitus [14, 28] and type 2 diabetes mellitus [5–10]. These mainly focus on microalbuminuria, and trials investigating macrovascular outcomes have not had concurrent results. The RIACE study group found no association between HbA1c variability and myocardial infarction or stroke [13], although average HbA1c variability in the individuals under investigation was lower (HbA1c-SD values at 0.46% [5.0 mmol/mol] in patients with cardiovascular disease [CVD] and 0.47% [5.1 mmol/mol] in patients without cardiovascular disease) in comparison with other studies. For example, a Finnish cohort study of type 1 diabetes mellitus patients [28] demonstrated an association between macrovascular outcomes and HbA1c variability, with HbA1c-SD at 0.79% (8.6 mmol/mol) without cardiovascular events and 0.87% (9.5 mmol/mol) in patients with cardiovascular events. A Chinese study observing a long-term SD of HbA1c in 8439 patients with type 2 diabetes mellitus was also able to establish that patients who developed CVD exhibited higher variability (HbA1c-SD 1,4% [15.3 mmol/mol] vs 1,1% [12.0 mmol/mol]). Here, CVD was defined more widely, including, for example, myocardial infarction, heart failure and non-fatal ischaemic stroke [10]. Interestingly, the recent literature is quite inconsistent about the relationship between the effect of low HbA1c and the risk of mortality or CVD [15]. Various studies demonstrated a consistent positive linear relationship between HbA1c and the risk of mortality or CVD [29, 30]. Other studies revealed a non-linear (U- or J-shaped) relationship [31, 32]. The present findings confirm to a great extent the recent results from Kontopantelis et al [33]. They showed, within a retrospective cohort study of more than 246,000 patients after adjustment for several important confounders, that the relationship between HbA1c levels and coronary and stroke mortality was positive curvilinear related (U-shaped). These results are in line with the present non-linear-findings, with the lowest risk for cardiovascular events and hypoglycaemia seen with an HbA1c variability of approximately 0.5% (5.5 mmol/mol) per quarter.
The definition and measurement of HbA1c variability present a central difficulty with such studies, as patients usually have irregular follow-up periods with measurements often unequally spaced. Our definition of HbA1c variability complements the more basic approach taken by previous studies [5–11, 13, 14, 28]. These have generally defined variability as the standard deviation of all HbA1c measurements during the observational period, with correction for the number of measurements available. This approach has two main problems. First, the length of time between measurements is ignored, leading to potentially misleading conclusions when HbA1c measurements are widely spaced. Second, with only a small number of measurements per patient, the validity and interpretation of the standard deviation, even with correction, is unclear. Based on the squared difference of the measurements to their average value, the approach would seem to amplify large differences. The difficulty in the definition and interpretation of HbA1c variability has been noted by several authors [15, 16]. Our approach provides a partial but imperfect solution to these problems; while accounting for the length of time between measurements, the variance of our statistic may be higher with widely spaced measurements. Further statistical refinement may therefore be possible. Only Skriver and colleagues used an improved definition similar to our own, averaging the absolute differences of the HbA1c measurements from a defined reference point [12]. The studies differ in their choice of reference point and thereby in the interpretation of the measure. For Skriver and colleagues, variability is the residual of the observations from a line connecting the first and last observation, such that a patient with linearly increasing or decreasing HbA1c is considered to have zero HbA1c variability. Our definition, providing a standardised measure of the rate of change in HbA1c value, would consider the same patient to have positive variability. It would seem that our measure more directly accounts for changes in HbA1c level, whereas Skriver and colleagues investigate the deviation from a smooth linear trend. Further work is required to establish the most robust method of measuring HbA1c variability in a clinical or study setting. Statistical simulation studies could shed further light on this question.
When comparing the results of the present study to similar studies, it is important to note that patients were observed from the initiation of insulin therapy. This patient group is potentially at higher risk of adverse events than others. Furthermore, our definition of HbA1c variability differs from the standard deviation used in other studies.
This study has several important strengths. The database used enabled the identification of a homogeneous group with regularly spaced, longitudinal records of HbA1c and other diabetes-related information. The size and composition of this study group represents a typical cohort of patients at high risk for HbA1c variability. The underlying DMP encompasses approximately 63% [34] of all type 2 diabetes mellitus patients in Bavaria, with data submitted by over 6000 practices. Although some selection effects have been recorded [35], the large scale of the DMP means that patients are recruited from the vast majority of primary care practices in Bavaria.
The routine data from the DMP for type 2 diabetes mellitus were collected for the purposes of quality improvement and not primarily for medical research. For this reason, several limitations should be considered. In contrast to controlled clinical studies, the DMP data are not subject to systematic external control or validation. Moreover, relevant information such as the insulin dosage or treatment regimen was not collected. In particular, the DMP data structure means that oral glucose-lowering medication can only be differentiated between metformin and ‘other oral glucose-lowering medication’ without further information on substance of dosage. A further limitation is that no record of patient dropout was available. In particular, myocardial events leading to death are not distinguishable from other forms of dropout. Mortality data were not available and therefore only non-lethal, documented outcomes could be observed, possibly leading to a bias that is difficult to quantify because of lack of data. It is noteworthy that the incidence of first myocardial infarction over the follow-up period is lower than that of stroke. As repeated events were not considered, this may reflect the higher incidence of myocardial infarction at baseline. Alternatively, myocardial infarction may more often lead to immediate dropout (e.g. death) and thus be missing from the underlying data set. Another limitation has to be considered regarding the patients’ sex. For approximately 900 patients with dropout before July 2008, the sex was unknown. Sensitivity analyses showed that various methods of dealing with these patients (e.g. remove from analysis, assign a ‘neutral’ sex or imputation using the available data) lead only to marginal changes in the estimated effect of HbA1c variability.
Finally, the DMP patient records are collected at intervals of either 3 or 6 months. Although the average lifespan of erythrocytes is 120 days, HbA1c is better correlated with the mean average blood glucose level within the past 8–12 weeks [36]. Thus, an evaluation of HbA1c variability should ideally measure HbA1c at intervals of 2 or 3 months in all patients. The frequency of HbA1c measurement compares favourably with other studies, but a controlled trial would be required to provide optimal data quality.
In summary, the results of the present study are, to a great extent, in line with findings of previous studies and recommendations like ACCORD [37], the ADA/EASD guidelines [38], which advise focusing more on a patient’s overall condition and comorbidities when determining HbA1c target values. In particular, our results suggest that patients experiencing a rapid and higher HbA1c variability are at increased risk for myocardial infarction, stroke, severe hypoglycaemia and emergency admissions.
These results support previous findings indicating that hard and fast targeting to normalise HbA1c values can lead to poorer outcomes. Further investigation is necessary to evaluate the general extent to which long-term variability in glucose control causes adverse effects in patients with type 2 diabetes mellitus. Further research is required to demonstrate whether HbA1c variability represents a reliable (possible causal) predictor of adverse events in everyday clinical practice, especially when considering changes in glucose-lowering treatment.
Abbreviations
- CVD:
-
Cardiovascular disease
- DMP:
-
Disease Management Program
- eGFR:
-
Estimated GFR
- HbA1c-SD:
-
Standard deviation of all HbA1c values
- RIACE:
-
Renal Insufficiency And Cardiovascular Events
References
Mokdad AH, Ford ES, Bowman BA et al (2003) Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 289:76–79
Ward A, Alvarez P, Vo L, Martin S (2014) Direct medical costs of complications of diabetes in the United States: estimates for event-year and annual state costs (USD 2012). J Med Econ 17:176–183
Moss SE, Klein R, Klein BE, Meuer SM (1994) The association of glycemia and cause-specific mortality in a diabetic population. Arch Intern Med 154:2473–2479
Selvin E, Marinopoulos S, Berkenblit G et al (2004) Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med 141:421–431
Sugawara A, Kawai K, Motohashi S et al (2012) HbA1c variability and the development of microalbuminuria in type 2 diabetes: Tsukuba Kawai Diabetes Registry 2. Diabetologia 55:2128–2131
Hsu CC, Chang HY, Huang MC et al (2012) HbA1c variability is associated with microalbuminuria development in type 2 diabetes: a 7-year prospective cohort study. Diabetologia 55:3163–3172
Rodriguez-Segade S, Rodriguez J, Garcia Lopez JM, Casanueva FF, Camina F (2012) Intrapersonal HbA1c variability and the risk of progression of nephropathy in patients with Type 2 diabetes. Diabet Med 29:1562–1566
Penno G, Solini A, Bonora E et al (2013) HbA1c variability as an independent correlate of nephropathy, but not retinopathy, in patients with type 2 diabetes: the Renal Insufficiency And Cardiovascular Events (RIACE) Italian multicenter study. Diabetes Care 36:2301–2310
Hirakawa Y, Arima H, Zoungas S et al (2014) Impact of visit-to-visit glycemic variability on the risks of macrovascular and microvascular events and all-cause mortality in type 2 diabetes: the ADVANCE trial. Diabetes Care 37:2359–2365
Luk AOY, Ma RCW, Lau ESH et al (2013) Risk association of HbA1c variability with chronic kidney disease and cardiovascular disease in type 2 diabetes: prospective analysis of the Hong Kong Diabetes Registry. Diabetes Metab Res Rev 29:384–390
Yang HK, Kang B, Lee S et al (2015) Association between hemoglobin A1c variability and subclinical coronary atherosclerosis in subjects with type 2 diabetes. J Diabetes Complicat 29:776–782
Skriver MV, Sandbaek A, Kristensen JK, Stovring H (2015) Relationship of HbA1c variability, absolute changes in HbA1c, and all-cause mortality in type 2 diabetes: a Danish population-based prospective observational study. BMJ Open Diabetes Res Care 3:e000060
Penno G, Solini A, Zoppini G et al (2013) Hemoglobin A1c variability as an independent correlate of cardiovascular disease in patients with type 2 diabetes: a cross-sectional analysis of the renal insufficiency and cardiovascular events (RIACE) Italian multicenter study. Cardiovasc Diabetol 12:98
Kilpatrick ES, Rigby AS, Atkin SL (2008) A1C variability and the risk of microvascular complications in type 1 diabetes: data from the Diabetes Control and Complications Trial. Diabetes Care 31:2198–2202
Rutter MK (2012) Low HbA1c and mortality: causation and confounding. Diabetologia 55:2307–2311
Monnier L, Colette C (2015) Association of HbA1c variability with atherosclerosis in diabetes: simple marker, risk factor or statistical bias? J Diabetes Complicat 29:745–746
Grambsch PM, Therneau TM (1981) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 3:515–526
Makuch RW (1982) Adjusted survival curve estimation using covariates. J Chronic Dis 35:437–443
Therneau TM, Grambsch PM (2000) Expected survival. In: Dietz K, Gail M, Krickeberg K, Samet J, Tsiatis A (eds) Modeling survival data: extending the Cox model, 1st edn. Springer, New York, pp 261–287
Bates D, Chambers J, Dalgaard P, Falcon S, Gentleman R (2009) R Development Core Team. R: a language and environment for statistical computing. Available from www.R-project.org, accessed 27 April 2015
Frontoni S, Di Bartolo P, Avogaro A, Bosi E, Paolisso G, Ceriello A (2013) Glucose variability: an emerging target for the treatment of diabetes mellitus. Diabetes Res Clin Pract 102:86–95
Ceriello A, Ihnat MA (2010) 'Glycaemic variability': a new therapeutic challenge in diabetes and the critical care setting. Diabet Med 27:862–867
Ihnat MA, Thorpe JE, Ceriello A (2007) Hypothesis: the 'metabolic memory', the new challenge of diabetes. Diabet Med 24:582–586
Yu T, Lin C, Chang S, Sung F, Kao C (2014) Increased risk of stroke in patients with chronic kidney disease after recurrent hypoglycemia. Neurology 83:686–694
Monnier L, Mas E, Ginet C et al (2006) Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 295:1681–1687
Frier BM, Schernthaner G, Heller SR (2011) Hypoglycemia and cardiovascular risks. Diabetes Care 34(Suppl 2):S132–S137
Desouza C, Salazar H, Cheong B, Murgo J, Fonseca V (2003) Association of hypoglycemia and cardiac ischemia: a study based on continuous monitoring. Diabetes Care 26:1485–1489
Waden J, Forsblom C, Thorn LM, Gordin D, Saraheimo M, Groop P (2009) A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Diabetes 58:2649–2655
Eeg-Olofsson K, Cederholm J, Nilsson PM et al (2010) New aspects of HbA1c as a risk factor for cardiovascular diseases in type 2 diabetes: an observational study from the Swedish National Diabetes Register (NDR). J Intern Med 268:471–482
Pfister R, Sharp SJ, Luben R, Khaw K, Wareham NJ (2011) No evidence of an increased mortality risk associated with low levels of glycated haemoglobin in a non-diabetic UK population. Diabetologia 54:2025–2032
Currie CJ, Peters JR, Tynan A et al (2010) Survival as a function of HbA(1c) in people with type 2 diabetes: a retrospective cohort study. Lancet 375:481–489
Selvin E, Steffes MW, Zhu H et al (2010) Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 362:800–811
Kontopantelis E, Springate DA, Reeves D et al (2015) Glucose, blood pressure and cholesterol levels and their relationships to clinical outcomes in type 2 diabetes: a retrospective cohort study. Diabetologia 58:505–518
Donnachie E, Hofmann F, Keller M. Qualitätsbericht 2010: Disease Managment Programme in Bayern (2011) [in German]. Available from www.kvb.de/fileadmin/kvb/dokumente/Praxis/Infomaterial/Versorgung/KVB-Bericht-DMP-qualitaetsbericht-2010.pdf, accessed 27 April 2015
Schafer I, Kuver C, Gedrose B et al (2010) Selection effects may account for better outcomes of the German Disease Management Program for type 2 diabetes. BMC Health Serv Res 10:351
Nathan DM, Singer DE, Hurxthal K, Goodson JD (1984) The clinical information value of the glycosylated hemoglobin assay. N Engl J Med 310:341–346
Gerstein HC, Miller ME, Genuth S et al (2011) Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med 364:818–828
Inzucchi SE, Bergenstal RM, Buse JB et al (2012) Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 55:1577–1596
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
FCB, ED, AS and MM designed the study. ED and FCB performed the analysis and wrote the initial version of the manuscript. MM and AS revised the manuscript. All authors read and approved the final manuscript. MM is the guarantor.
Additional information
Florian C. Bonke and Ewan Donnachie contributed equally to this study
Rights and permissions
About this article
Cite this article
Bonke, F.C., Donnachie, E., Schneider, A. et al. Association of the average rate of change in HbA1c with severe adverse events: a longitudinal evaluation of audit data from the Bavarian Disease Management Program for patients with type 2 diabetes mellitus. Diabetologia 59, 286–293 (2016). https://doi.org/10.1007/s00125-015-3797-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3797-z