Abstract
Aims/hypothesis
Circulating lipopolysaccharide-binding protein (LBP) is an acute-phase reactant known to be increased in obesity. We hypothesised that LBP is produced by adipose tissue (AT) in association with obesity.
Methods
LBP mRNA and LBP protein levels were analysed in AT from three cross-sectional (n = 210, n = 144 and n = 28) and three longitudinal (n = 8, n = 25, n = 20) human cohorts; in AT from genetically manipulated mice; in isolated adipocytes; and in human and murine cell lines. The effects of a high-fat diet and exposure to lipopolysaccharide (LPS) and peroxisome proliferator-activated receptor (PPAR)γ agonist were explored. Functional in vitro and ex vivo experiments were also performed.
Results
LBP synthesis and release was demonstrated to increase with adipocyte differentiation in human and mouse AT, isolated adipocytes and human and mouse cell lines (Simpson–Golabi–Behmel syndrome [SGBS], human multipotent adipose-derived stem [hMAD] and 3T3-L1 cells). AT LBP expression was robustly associated with inflammatory markers and increased with metabolic deterioration and insulin resistance in two independent cross-sectional human cohorts. AT LBP also increased longitudinally with weight gain and excessive fat accretion in both humans and mice, and decreased with weight loss (in two other independent cohorts), in humans with acquired lipodystrophy, and after ex vivo exposure to PPARγ agonist. Inflammatory agents such as LPS and TNF-α led to increased AT LBP expression in vivo in mice and in vitro, while this effect was prevented in Cd14-knockout mice. Functionally, LBP knockdown using short hairpin (sh)RNA or anti-LBP antibody led to increases in markers of adipogenesis and decreased adipocyte inflammation in human adipocytes.
Conclusions/interpretation
Collectively, these findings suggest that LBP might have an essential role in inflammation- and obesity-associated AT dysfunction.
Similar content being viewed by others
Introduction
Obesity-induced adipose tissue (AT) dysfunction is characterised by hypertrophy and hyperplasia of resident cells and enrichment of infiltrating inflammatory cells [1, 2]. In this proinflammatory context, AT functionality depends on the resilience of adipocytes to this surrounding hostile cellular environment. Recent investigations have shown a relationship between metabolic endotoxaemia and insulin resistance [3–6]. Proinflammatory actions of lipopolysaccharide (LPS) are known to blunt insulin signalling and to prevent adipogenesis [7, 8]. Several mediators of the LPS response (toll-like receptor 4 [TLR4] and cluster of differentiation 14 [CD14]) are increased in AT in association with metabolic disturbances and systemic inflammation [9, 10].
Lipopolysaccharide-binding protein (LBP) is an acute-phase reactant 65 kDa protein, present in blood at high concentrations and thought to be derived mainly from the liver [11]. LBP recognises the lipid A component of LPS monomers and accelerates LPS binding to CD14, enhancing the sensitivity of cells to LPS [12, 13]. Previous reports have shown a strong association between concentration of circulating LBP and obesity-associated metabolic disturbances [14–17]. In agreement with these studies, we found that concentrations of circulating LBP increased in obesity and decreased after weight loss [18]. However, despite the association of LBP concentration with changes in fat mass, all these studies claimed the liver as the main source of variation in the concentration of circulating LBP [14–18]. A recent study described LBP secretion by 3T3-L1 adipocytes [19] and increased serum LBP levels in genetically and diet-induced obese mice after LPS injection, but AT LBP production was not investigated [19]. Supporting this novel finding, Ge et al found Lbp gene expression and LBP protein secretion in 3T3-F442A cells and in de novo AT formed from 3T3-F442A cells, showing that its regulation was mediated by microRNA 883b (miR883b)-5p [20]. However, they did not study Lbp gene expression in mice adipocytes or mice AT. To the best of our knowledge, no previous studies have addressed the aims of this study, which are to: (1) study LBP gene and protein expression in human and mice AT, in AT fractions (adipocytes vs stromal vascular cells [SVCs]) and during human adipocyte differentiation; (2) test the effects of a high-fat diet, inflammatory cytokines, LPS and peroxisome proliferator-activated receptor (PPAR)γ agonists in AT LBP biosynthesis; and (3) investigate the possible functional role of LBP in subcutaneous and visceral adipocyte differentiation.
Methods
Human studies
Cross-sectional studies
A group of 210 AT samples (110 visceral and 100 subcutaneous depots) were obtained from participants with a BMI between 20 and 68 kg/m2, recruited at the Endocrinology Service of the Hospital Universitari ‘Dr Josep Trueta’ (Girona, Spain) (cohort 1).
An independent replication study of 144 AT samples (72 paired subcutaneous and visceral depots) was performed at the Hospital Universitari Joan XXIII (Tarragona, Spain) (cohort 2).
The lipodystrophy cohort (cohort 3) corresponded to a previously described cohort, comprising: seven HIV-1-infected patients receiving antiretroviral treatment and showing overt peripheral lipoatrophy; seven HIV-1-infected patients receiving antiretroviral treatment without peripheral lipoatrophy; seven naive (non-treated) HIV-1-infected patients; and seven control individuals [21]. Subcutaneous AT (SAT) samples were obtained from the abdominal region. See electronic supplementary material (ESM) Methods for further details.
Longitudinal studies
In order to study the effects of weight loss, two cohorts were recruited: eight white morbidly obese (BMI 50.4 ± 9 kg/m2, aged 40 ± 10 years [mean ± SD]) women with normal glucose tolerance, from whom biopsies of SAT were obtained before and 2 years after bariatric surgery (the study is described in detail elsewhere [22]) (cohort 4); and 25 white obese individuals who underwent bariatric surgery thought Roux-en-Y gastric bypass (RYGB) at Hospital Universitari ‘Dr Josep Trueta’ (see ESM Methods for further details) (cohort 5).
To study the effect of weight gain, LBP mRNA expression was determined in SAT from 20 healthy male volunteers who participated in a controlled overfeeding protocol (described in detail elsewhere [23]). See ESM Methods for further details.
Ex vivo experiments
Isolated samples of SAT or paired visceral AT (VAT) and SAT samples were obtained from seven obese (mean age 46 ± 6.4 years, BMI 44.9 ± 12.4 kg/m2) individuals undergoing open abdominal surgery (gastrointestinal bypass) under anaesthesia after an overnight fast. See ESM Methods for further details. Ex vivo experiments were performed using AT samples as previously described [24]. Rosiglitazone doses were 0.5 and 5 μmol/l.
Animal studies
Effects of a high-fat diet and LPS
Twelve-week-old male C57BL/6J mice (Charles River Laboratories International, Wilmington, MA, USA) and CD14 mutant male mice (Jackson Laboratory, Bar Harbor, ME, USA) were bred on a C57BL/6J background and housed in a controlled environment (inverted 12 h daylight cycle, lights off at 10:00 hours) with free access to food and water. All the animal experimental procedures to test the effects of a high-fat diet and LPS were studied using mesenteric white AT (WAT). They were approved by the local ethics committee of the Rangueil Hospital, Toulouse, France and were performed as previously described [4, 18, 25, 26].
Effects of PPARγ agonists
The effects of thiazolidinedione (TZD) treatment were studied using epididymal WAT from male 16 week old C57BL/6J WT mice fed a chow diet supplemented with or without 10 parts per million (ppm) rosiglitazone (Avandia) for 3 weeks from week 13 to week 16.
Chow-fed wild-type (WT), obese/obese knockout (ob/ob), Pparg-knockout (PpargKO), and ob/ob/PpargKO (POKO) male mice were generated on a mixed background as previously described [27] and epididymal AT was collected from groups at 4 and 16 weeks of age.
In vitro experiments
LBP expression in isolated cells
Samples of SAT obtained from 12 women (28.9 ± 1.9 kg/m2) were fractionated as described elsewhere [28]. CD14+ cells isolated from the SVC fraction were isolated using magnetic anti-CD14 immunobeads (MACS Technology, Miltenyi Biotec, Madrid, Spain).
LBP during human pre-adipocyte differentiation
Living SVCs from both visceral and SAT samples were resuspended in 2 ml erythrocyte lysis buffer (ammonium chloride) for 10 min on ice, washed two times with 20 ml PBS with 2% penicillin/streptomycin (vol./vol.) and centrifuged at 400 g for 5 min at room temperature. Pure SVCs and isolated pre-adipocytes (Zen-Bio, Research Triangle Park, NC, USA) were cultured as previously described [24].
Effects of TNF-α, LPS and rosiglitazone on human pre-adipocytes
In human pre-adipocytes, treatments were performed during adipocyte differentiation. For TNF-α and LPS-stimulated macrophage-conditioned medium (LPS-MCM) experiments, adipocytes were incubated with fresh medium (control), fresh medium containing TNF-α (100 ng/ml) and macrophage-conditioned medium (MCM; 5%, vol./vol.) from THP-1 cells previously treated with 10 ng/ml LPS. For the rosiglitazone (0.1 and 1 μmol/l) experiment, adipocyte differentiation was performed with rosiglitazone-free differentiation medium. All these treatments were performed in triplicate.
Effects of anti-mouse-LBP antibody in human adipocytes
Anti-mouse-LBP antibody (Ab) biG 33 (0.5 μg/ml) was obtained from Abnova (Taipei, Taiwan). Anti-mouse-LBP Ab, which cross-reacts with human LBP, was administered in the last 2 days of subcutaneous and visceral human adipocyte differentiation. This specific blocking effect on human LBP has been shown elsewhere [29]. After 48 h, the supernatant fractions were centrifuged at 400 g for 5 min, cells were harvested and the pellets and supernatant fractions were stored at −80°C for RNA analysis. All these treatments were performed in triplicate.
Human multipotent adipose-derived stem cells
Human multipotent adipose-derived stem (hMADs) cells were cultured and differentiated as previously described [30]. See ESM Methods for further details.
Simpson–Golabi–Behmel syndrome cell and 3T3-L1 adipocyte differentiation procedures
Confluent Simpson–Golabi–Behmel syndrome (SGBS) pre-adipocytes and 3T3-L1 were induced to differentiate to mature adipocytes in adipocyte differentiation medium over 18 and 7 days, respectively. See ESM Methods for further details.
Effects of TNF-α, LPS-MCM and rosiglitazone on 3T3-L1 cells
TNF-α (10 ng/ml) and LPS-MCM (0.5% and 5%, vol./vol.) were administered during 3T3-L1 differentiation. Rosiglitazone (10 nmol/l) was added during 3T3-L1 differentiation.
Human LBP knockdown
Permanent silencing was performed using LBP-targeted and control short hairpin (sh)RNA lentiviral particles (sc-43890-V and sc-108080, Santa Cruz Biotechnology, CA, USA) and following the manufacturer’s instructions.
Analytical methods
LBP levels, serum glucose, HbA1c, serum insulin, total cholesterol, HDL-cholesterol, LDL-cholesterol and total serum triacylglycerols were measured as previously described [18]. See ESM Methods for further details.
RNA purification and gene expression analysis
RNA purification and gene expression procedures and analyses were performed as previously described [24, 31]. See ESM Methods for further details.
Western blot assays
Western blot analysis was performed as previously described [24] using a 1:1,000 dilution of a rabbit anti-human-LBP Ab (AbCam) and mouse anti-human β-actin Ab (Sigma-Aldrich).
Statistical methods
Statistical analyses were performed using SPSS 12.0 software (SPSS, Chicago, IL, USA). The relationships between variables were analysed by simple correlation (Pearson’s test and Spearman’s test) and multiple regression analyses. One-factor ANOVA with post hoc Bonferroni test, paired t tests and unpaired t tests were used to compare LBP gene expression in cross-sectional and longitudinal cohorts. A non-parametric test (Mann–Whitney test) was used to analyse in vitro experiments. The levels of statistical significance were set at p < 0.05. See ESM Methods for further details.
Results
AT LBP in association with obesity and insulin resistance
Anthropometrical and clinical variables from the two cross-sectional cohorts are detailed in Table 1. The LBP gene was found to be expressed in human AT, being substantially increased in SAT vs VAT (0.091 [0.01–0.24] vs 0.023 [0.005–0.052] relative units of gene expression [RU]; p < 0.0001). LBP was expressed at significantly higher levels in obese vs non-obese individuals in parallel to the degree of metabolic deterioration (i.e. with increased fasting glucose, insulin resistance, HbA1c, fasting triacylglycerols and decreased adiponectin levels) and this was confirmed in two independent cohorts in both SAT and VAT (Fig. 1a,b, Table 2). In both cohorts, SAT LBP gene expression was negatively associated with anabolic and adipogenic genes (e.g. PPARγ [also known as PPARG], FABP4, FASN and ACC1) and lipid-droplet-associated genes (perilipin1, PLIN1), and positively associated with proinflammatory and macrophage-related genes (IL6, CD14). Similarly, VAT LBP gene expression was negatively associated with PPARγ, FASN, PLIN1 and omentin (ITLN1), and positively associated with proinflammatory genes such as HIF1α (also known as HIF1A), MCP1, TNF and visfatin. These findings suggested that LBP was regulated during the process of AT expansion and inflammation (Table 3).
LBP gene expression in SAT (a) and VAT (b) from individuals, according to obesity status. * p < 0.05 and ** p < 0.01 compared with normal weight participants; † p < 0.05 and †† p < 0.01 compared with overweight participants. (c) LBP gene expression in human visceral pre-adipocytes and adipocytes vs subcutaneous pre-adipocytes and adipocytes. * p < 0.05 and ** p < 0.01 compared with VAT; † p < 0.05 and †† p < 0.01 compared with respective pre-adipocytes. (d) LBP gene expression during subcutaneous pre-adipocyte differentiation from lean and obese individuals. ** p < 0.01 compared with day 0; † p < 0.05 compared with adipocytes from lean individuals. (e) LBP gene expression and (f) concentration of circulating LBP released into the medium by adipocytes (n = 12) and SVCs (n = 12) over 24 h. (g) LBP released during adipocyte differentiation at day 14. ** p < 0.01 compared with pre-adipocytes. (h) Time course of LBP gene expression and protein release in hMAD cells.* p < 0.05 and ** p < 0.01compared with day 0. (i) LBP gene expression and LBP protein levels during SGBS differentiation. (j) Lbp gene expression and LBP protein released during 3T3-L1 differentiation. * p < 0.05 and ** p < 0.01 compared with day 0. D, day
As TNF-α production in AT is known to be strongly associated with endoplasmic reticulum (ER) stress, we also explored the possible relationship between LBP and ER stress markers (such as heat shock 70 kDa protein 5 [glucose-regulated protein, 78 kDa] [HSPA5] and activating transcription factor 6 [ATF6]). Confirming previous studies, TNF gene expression was significantly correlated with these ER stress markers (with HSPA5 [r = 0.43, p = 0.006] and with ATF6 [r = 0.37, p = 0.02] in VAT, and only with ATF6 [r = 0.32, p = 0.03] in SAT), but no association was found between LBP gene expression and ER stress markers. However, within morbidly obese individuals, LBP gene expression was significantly associated with HSPA5 (r = 0.41, p = 0.02) in VAT, and tended to be associated in SAT (r = 0.28, p = 0.08).
LBP mRNA and protein levels in isolated adipocytes are associated with obesity
In agreement with the AT data, the increase in LBP expression was most prominent in adipocytes derived from SAT vs VAT (at day 14 of adipocyte differentiation, Fig. 1c) in parallel with a more robust activation of the adipogenic programme and fat accumulation in SAT vs VAT (ESM Fig. 1a). LBP gene transcript and LBP protein levels were also higher in adipocytes from obese vs non-obese individuals (Fig. 1d, ESM Fig. 1b). Thus, the increase in LBP synthesis runs in parallel with the differentiation of adipocytes and accumulation of lipid.
LBP gene expression during adipocyte differentiation
Cellular AT fractionation demonstrated that LBP transcript expression is restricted to the adipocyte population (Fig. 1e). In agreement with this, the level of LBP protein released into the media (24 h culture) was significantly increased in cultures of mature adipocytes compared with SVCs (27.6 ± 6.7 vs 2.05 ± 0.15 ng/ml; p < 0.0001; Fig. 1f). To investigate whether changes in LBP expression associated with obesity and insulin resistance were related to AT macrophage infiltration, LBP gene expression was studied in isolated AT macrophages (CD14+ cells). LBP gene expression was increased in CD14− vs CD14+ cells (0.0032 ± 0.002 vs 0.00041 ± 0.0001 RU; p = 0.005) but the absolute contribution to AT changes was meaningless given the low expression levels in macrophages compared with adipocytes (ESM Fig. 1c). LBP protein release from mature adipocytes was higher compared with pre-adipocytes (Fig. 1g). To assess the time-course changes, cells and supernatant fractions were sequentially obtained at days 0, 3, 7, 10 and 13 of human adipocyte differentiation. Levels of LBP transcript and LBP protein progressively increased, mainly in the later stages of adipocyte differentiation (days 10 and 13, Fig. 1h) similar to FASN and ADIPOQ (ESM Fig. 1d). The increase in LBP was independently confirmed in human SGBS cells (Fig. 1i) and mouse 3T3-L1 cells (Fig. 1j) similar to Fasn (ESM Fig. 1e).
Effects of decreased fat mass on AT LBP
Weight loss in obese individuals is known to release the pressure on the mechanisms promoting AT expansion and improve insulin sensitivity. Accordingly, in two independent cohorts, weight loss led to a decrease in AT LBP transcription, mirroring improved insulin sensitivity and an increase in the gene expression of markers typically downregulated in insulin-resistant states (Table 4, Fig. 2a and ESM Fig. 2a–c). In addition, the percentage change in weight loss correlated positively with ADIPOQ (r = 0.56, p = 0.003), and negatively with LEP (r = −0.64, p = 0.001), TNF (r = −0.46, p = 0.02) and LBP (r = −0.62, p = 0.001) gene expression. Interestingly, the percentage change in LBP was significantly correlated with the percentage change in LEP (r = 0.73, p < 0.0001) and TNF (r = 0.60, p = 0.002).
(a) LBP gene expression in SAT after surgery-induced weight loss (n = 8). ** p < 0.01 compared with pre-weight loss. (b) LBP gene expression in SAT according to lipodystrophy status in individuals with HIV (n = 28; n = 7 for each group). * p < 0.05 and ** p < 0.01 compared with control participants; † p < 0.05 compared with participants without lipodystrophy. (c) LBP gene expression in SAT after overfeeding weight gain (n = 20). ** p < 0.01 compared with before diet. (d) Comparison of Lbp gene expression in WAT from high-fat-induced obese and insulin-resistant C57BL/6J mice. * p < 0.05 and ** p < 0.01 compared with respective lean mice. (e) Lbp gene expression in WAT from C57BL/6J mice after TZD treatment. ** p < 0.01 compared with control-treated mice. (f) Effects of rosiglitazone (10 nmol/l) on Lbp gene expression during 3T3-L1 differentiation at day 7. ** p < 0.01 compared with vehicle. (g) Effects of rosiglitazone (0.1 and 1 μmol/l) on LBP gene expression during human adipocyte differentiation at day 14. ** p < 0.01 compared with differentiated control. (h) Effects of rosiglitazone (0.5 and 5 μmol/l) on LBP gene expression and LBP secreted protein in human SAT explants. * p < 0.05 compared with control. (i) Effects of rosiglitazone (0.5 and 5 μmol/l) on LBP gene expression in human paired SAT and VAT explants. * p < 0.05 and ** p < 0.01 compared with control. Black bars, SAT; grey bars, VAT. (j) Lbp gene expression in WAT from 4-week-old C57BL/6J knockout mice (ob/ob, PpargKO and POKO). * p < 0.05 and ** p < 0.01 compared with WT mice. All in vitro and ex vivo experiments were performed in triplicate. In (g–i), rosiglitazone concentrations are in μmol/l. Diff, differentiated; LD, lipodystrophy; Ros, rosiglitazone
To dissect the effect of fat mass from that of insulin resistance on LBP levels we investigated the regulation of LBP in lipodystrophy. In this case, and contrary to weight loss, the decrease in fat mass is associated with a primary failure of AT and is associated with insulin resistance and dyslipidaemia [21]. Not surprisingly, the expression of adipocyte gene markers (PPARγ and adiponectin) was decreased in poorly differentiated AT from lipodystrophic patients. Of interest, levels of LBP were also decreased in lipodystrophic samples in comparison with control individuals. These findings suggest that expression of LBP requires normal adipocyte differentiation and excessive fat accretion. However, for the same degree of adipocyte differentiation and fat accumulation, LBP levels were relatively higher among those lipodystrophic patients who were more insulin resistant and dyslipidaemic (Fig. 2b and ESM Fig. 2d–e). Thus, these data also suggest that the induction of LBP mRNA is exacerbated by the degree of insulin resistance and inflammation.
Overfeeding and increased fat mass increases LBP transcription in human and mouse AT
We next evaluated the effect of overnutrition and weight gain on LBP expression in SAT samples from 20 healthy male volunteers who underwent a 56 day overfeeding protocol with a daily excess energy of 3,138 kJ [23]. As a result of this intervention, body weight increased (+2.5 kg) in parallel to increased AT LBP mRNA expression (7.5 ± 0.8 RU before diet vs 10.7 ± 1.5 RU after diet (p = 0.003) (mean fold change: 1.4) (Fig. 2c). These results were recapitulated in VAT from obese murine models in which the Lbp gene was highly expressed in murine mesenteric WAT and correlated with circulating LBP (r = 0.8, p < 0.0001); it increased further in C57BL/6J mice after a high-fat diet (Fig. 2d).
The effect of PPARγ agonists on AT LBP expression
Of note, treatment with a TZD, a drug group known to promote adipogenesis and improve insulin sensitivity, resulted in decreased LBP levels in epididymal WAT in parallel with increased insulin sensitivity (Fig. 2e). Thus, this result raised the question of whether increased LBP expression was not related to the process of AT expansion of fat mass but to the metabolic impairment typically associated with it. This was further investigated using an in vitro system. Specifically, we observed that rosiglitazone led to decreased LBP (Fig. 2f) in parallel to improved insulin signalling markers in 3T3-L1 cells (ESM Fig. 3a–f), in human adipocytes (Fig. 2g) and in human whole AT explants treated ex vivo (Fig. 2h). To elucidate the potentially different effects of rosiglitazone on VAT and SAT, the experiment was performed again in paired SAT and VAT explants. There was a greater reduction in LBP gene expression and secreted protein after rosiglitazone in SAT when compared with VAT explants (Fig. 2i). Similarly, the decrease in leptin and the increase in ADIPOQ gene expression were more marked in SAT explants (ESM Fig. 3g, h).
We next studied this effect in vivo by comparing the expression of LBP in the epididymal WAT of several knockout mice (ob/ob, PpargKO and POKO) characterised by limited fat accretion and exacerbated metabolic disturbance compared with that in WT mice [27]. Our results indicate that at 4 weeks of age, LBP was significantly increased in ob/ob and POKO mice compared with WT and PpargKO mice. This indicated that induction of LBP was more rapid in AT highly challenged to expand (ob/ob genotype) in parallel with the exponential growth phase of adipose expansion characterised by adipocyte differentiation, fat deposition and weight increase (Fig. 2j).
AT LBP mRNA is induced by inflammation
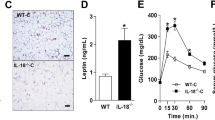
We confirmed the direct involvement of LBP in the inflammatory response by showing that LPS treatment increases AT LBP gene expression (Fig. 3a). This effect was mediated by CD14 as it was not observed in Cd14-knockout mice, consistent with the role of CD14 in the transduction of the LPS signal (Fig. 3a).
(a) Lbp gene expression in WT and Cd14-knockout mice treated with LPS. * p < 0.05 compared with control; † p < 0.05 compared with WT mice treated with LPS. (b–d) Effects of LPS-MCM (0.5 and 5%) on Lbp gene expression (b), LBP protein released (c) and Il6 gene expression (d) in 3T3-L1 cells undergoing differentiation at day 2. * p < 0.05 compared with differentiated control at day 2 (vehicle). Effects of TNF-α (10 ng/ml) on Lbp gene expression (e) and on LBP protein released (f) during 3T3-L1 differentiation. ** p < 0.01 compared with differentiated control. (g) Effects of TNF-α (100 ng/ml) and LPS-MCM (5%) on LBP gene expression in human adipocytes. * p < 0.05 compared with control. In vitro experiments were performed in triplicate. Diff, differentiated; KO, knockout
Treatment with TNF-α and LPS-MCM also led to an increase in LBP in 3T3-L1 cells and human adipocytes in parallel with decreased expression of adipogenic genes (FASN, PPARγ and ADIPOQ) (Fig. 3b–g, ESM Fig. 4a–f). In agreement with this, human adipocytes of obese individuals were characterised by increased LBP and decreased lipogenic gene expression compared with non-obese individuals (Fig. 1d, ESM Fig. 1b).
Collectively, these results suggest that expression of LBP occurs in differentiated adipocytes, and that LBP increases in parallel with increased fat mass, being exacerbated under insulin-resistant conditions.
LBP knockdown and anti-LBP effects on human adipogenesis
LBP knockdown in human subcutaneous and visceral pre-adipocytes using shRNA lentiviral particles, decreasing LBP expression by 50–60%, led to increased expression of adipogenic genes (such as ADIPOQ and GLUT4) and decreased inflammatory genes (such as IL6) during differentiation (Fig. 4a–h). In line with LBP-knockdown results, anti-LBP Ab (0.5 μg/ml) administration in the last 2 days of human adipocyte differentiation (when the maximum adipocyte-secreted LBP concentration was reached [50–60 ng/ml]) led to improved adipogenic status of fully differentiated subcutaneous and visceral adipocytes, increasing the expression of adipogenic genes and reducing IL6 mRNA levels (Fig. 5a–h).
Subcutaneous (a–d) and visceral (e–h) pre-adipocytes were treated with a non-targeted shRNA (control) or with an shRNA targeted to silence LBP (shLBP). Control cells and cells with LBP knockdown were induced to differentiate using a standard adipogenic cocktail, and the mRNA expression levels of the genes LBP (a, e), IL6 (b, f) ADIPOQ (c, g) and GLUT4 (d, h) were measured at the end (day 14) of adipogenic differentiation. * p < 0.05 and ** p < 0.01 compared with control. shC, control cells treated with non-targeted shRNA; shLBP, treated with shRNA targeted to silence LBP
Discussion
A dramatic upregulation of circulating LBP concentration has been reported in obese individuals with increased fat mass [16–18]. Although circulating LBP is thought to derive from the liver [13, 32], the close relationship between circulating LBP and obesity led us to investigate the possible contribution of AT to circulating LBP levels. In support of this relationship, a recent study reported increased LBP gene and protein expression in AT formed de novo using 3T3-F442A-transfected cells with a plasmid containing antagomirs against miR883b-5p [20]. Expression of LBP occurred in human AT and was substantially increased in SAT vs VAT, and in obese vs non-obese individuals. AT LBP mRNA and LBP protein levels were higher with progressive metabolic deterioration (i.e. with increased fasting glucose, insulin resistance, HbA1c, fasting triacylglycerols and decreased adiponectin). Interestingly, LBP gene expression was restricted to adipocytes. That LBP was possibly playing a role in adipocyte biology was suggested by the negative associations of LBP with genes involved in adipogenesis and the structure of lipid droplets, and by the positive associations with inflammation-related genes. In fact, LBP is part of a family of structurally and functionally related lipid-transfer proteins, including bactericidal/permeability-increasing protein (BPI), cholesteryl ester transfer protein (CETP) and phospholipid transfer protein (PLTP) [33, 34]. The involvement in adipocyte biology was confirmed in isolated adipocytes. LBP gene expression and LBP protein release into culture medium increased during differentiation of human adipocytes, reaching maximum production when the adipocyte was fully differentiated. The increase in LBP was confirmed in human SGBS cells and in the mouse 3T3-L1 cell line. Interestingly, LBP knockdown led to improved human adipogenic markers and decreased adipocyte inflammation. Of note, inhibition of LBP activity using a specific anti-LBP Ab led to improved adipogenic status of fully differentiated adipocytes.
We thus confirmed, in several cell models, that the accumulation of lipids in adipocytes was a signal for LBP synthesis to occur. If this hypothesis is correct, lipid depletion should lead to the opposite phenotype. In agreement with this hypothesis, LBP decreased significantly in two models of lipid depletion: after weight loss; and in individuals with acquired lipodystrophy. The decrease after weight loss occurred in parallel with increased insulin sensitivity and decreased IL6 gene expression, suggesting that both insulin action and inflammatory pathways were playing a role in the modulation of LBP. Otherwise, in human and mice, overnutrition-induced weight gain led to significantly increased LBP gene expression in AT.
To confirm the associations with adipogenic pathways, we evaluated different models of insulin sensitisation. LBP gene expression was confirmed in subcutaneous WAT of mice and correlated with level of circulating LBP. In agreement with human data, Lbp mRNA was increased in obese and insulin-resistant mice. Pharmacological insulin sensitisation using rosiglitazone led to decreased Lbp in parallel with increases in markers of insulin signalling in 3T3-L1 cells. Effects similar to those of rosiglitazone were observed in human adipocytes and in human whole AT explants treated ex vivo. The inflammatory state of VAT is known to be more marked when compared with SAT [35]. However, the major proinflammatory cytokines (TNF-α, IL-6) are mainly produced by the stromo-vascular fraction of AT [35]. The LBP gene and LBP protein were expressed mainly in adipocytes, with higher expression in subcutaneous vs visceral adipocytes. According to its proinflammatory activity, LBP would be expected to be increased in visceral adipocytes, but this was not the case. However, leptin is another factor with recognised proinflammatory activity that is increased in subcutaneous vs visceral adipocytes. Interestingly, weight loss led to tightly linked reduced expression of these adipocyte factors, leptin and LBP. Furthermore, in both SAT and VAT explants, rosiglitazone led to a greater reduction in LBP in parallel with that of LEP, whereas ADIPOQ gene expression was higher in SAT vs VAT.
We then investigated the role of inflammation in LBP expression. LPS, one of the most potent inflammatory triggers, led to increased AT LBP gene expression, while this was prevented in Cd14-knockout mice, consistent with the role of CD14 in the transduction of the LPS signal. TNF-α- and LPS-stimulated MCM also led to increased LBP in parallel with decreased expression of adipogenic genes in 3T3-L1 cells and in human adipocytes. In fact, human adipocytes from obese individuals were also characterised by increased LBP and decreased lipogenic gene expression when compared with those from non-obese individuals. Inflammation-induced AT LBP biosynthesis may promote macrophage infiltration and recruitment in AT by increasing nuclear factor of κ light polypeptide gene enhancer in B cells 1 (NFκB) proinflammatory activity in adipocytes [36–38]. Supporting this idea, Lbp gene expression preceded the expression of different macrophage markers in Pparγ +/− and POKO mice. Previous findings demonstrated that TLR4 knockdown in whole AT led to decreased inflammatory responses in mice fed a high-fat diet and that saturated fatty acids are the main triggers of TLR4 activation in AT [39–42]. It is known that LBP enhancement of LPS inflammatory effects in macrophages requires TLR4 [12, 13]. Additional experiments will be necessary to elucidate whether the well-known proinflammatory activity of LBP might underlie its negative effects on adipocyte differentiation. The association between LBP and HSPA5 in VAT from morbidly obese individuals suggests a possible link between inflammation-triggered adipocyte LBP biosynthesis and ER stress, at least in morbid obesity. This finding should be explored further.
Taken together, the data reported in the current study lead us to conclude that LBP is a novel adipokine that might display an essential role in inflammation- and obesity-associated AT dysfunction. Induction of LBP in the context of overnutrition and positive energy balance may contribute to obesity-associated metabolic complications through the prevention of AT expansion, leading to adipocyte dysfunction. In this context, increased LBP levels may cause metabolic stress and contribute to a vicious cycle that prevents further AT expansion and exacerbates the AT inflammatory response (Fig. 6). Current findings point at novel therapeutic approaches directed to inhibit LBP to uncouple the effects of positive energy balance from its associated metabolic effects. Furthermore, measurement of LBP levels may constitute an early biomarker related to AT dysfunctionality.
Abbreviations
- Ab:
-
Antibody
- AT:
-
Adipose tissue
- CD14:
-
Cluster of differentiation 14
- ER:
-
Endoplasmic reticulum
- hMADs:
-
Human multipotent adipose-derived stem cells
- HSPA5:
-
Heat shock 70 kDa protein 5 (glucose-regulated protein, 78 kDa)
- LBP:
-
Lipopolysaccharide-binding protein
- LPS:
-
Lipopolysaccharide
- LPS-MCM:
-
LPS-stimulated macrophage-conditioned medium
- MCM:
-
Macrophage-conditioned medium
- ob/ob :
-
Obese/obese knockout
- POKO:
-
ob/ob/PpargKO
- PPAR:
-
Peroxisome proliferator-activated receptor
- PpargKO:
-
Pparg-knockout
- RU:
-
Relative unit of gene expression
- SAT:
-
Subcutaneous AT
- SGBS:
-
Simpson–Golabi–Behmel syndrome cell line
- shRNA:
-
Short hairpin RNA
- SVCs:
-
Stromal vascular cells
- TLR4:
-
Toll-like receptor 4
- TZD:
-
Thiazolidinedione
- VAT:
-
Visceral adipose tissue
- WAT:
-
White adipose tissue
- WT:
-
Wild-type
References
Wormser D, Kaptoge S, Di Angelantonio E et al (2011) Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet 377:1085–1095
Ouchi N, Parker JL, Lugus JJ, Walsh K (2011) Adipokines in inflammation and metabolic disease. Nat Rev Immunol 11:85–97
Cani PD, Amar J, Iglesias MA et al (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56:1761–1772
Cani PD, Bibiloni R, Knauf C et al (2008) Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57:1470–1481
Lassenius MI, Pietiläinen KH, Kaartinen K et al (2011) Bacterial endotoxin activity in human serum is associated with dyslipidemia, insulin resistance, obesity, and chronic inflammation. Diabetes Care 34:1809–1815
Osto M, Zini E, Franchini M et al (2011) Subacute endotoxemia induces adipose inflammation and changes in lipid and lipoprotein metabolism in cats. Endocrinology 152:804–815
Chung S, Lapoint K, Martinez K, Kennedy A, Boysen Sandberg M, McIntosh MK (2006) Preadipocytes mediate lipopolysaccharide-induced inflammation and insulin resistance in primary cultures of newly differentiated human adipocytes. Endocrinology 147:5340–5351
Creely SJ, McTernan PG, Kusminski CM et al (2007) Lipopolysaccharide activates an innate immune system response in human adipose tissue in obesity and type 2 diabetes. Am J Physiol Endocrinol Metab 292:E740–E747
Schäffler A, Schölmerich J (2010) Innate immunity and adipose tissue biology. Trends Immunol 31:228–235
Fernández-Real JM, Pérez del Pulgar S, Luche E et al (2011) CD14 modulates inflammation-driven insulin resistance. Diabetes 60:2179–2186
Myc A, Buck J, Gonin J, Reynolds B, Hammerling U, Emanuel D (1997) The level of lipopolysaccharide-binding protein is significantly increased in plasma in patients with the systemic inflammatory response syndrome. Clin Diagn Lab Immunol 4:113–116
Tobias PS, Soldau K, Ulevitch RJ (1989) Identification of a lipid A binding site in the acute phase reactant lipopolysaccharide binding protein. J Biol Chem 264:10867–10871
Hailman E, Lichenstein HS, Wurfel MM et al (1994) Lipopolysaccharide (LPS)-binding protein accelerates the binding of LPS to CD14. J Exp Med 179:269–277
van Dielen FM, Buurman WA, Hadfoune M, Nijhuis J, Greve JW (2004) Macrophage inhibitory factor, plasminogen activator inhibitor-1, other acute phase proteins, and inflammatory mediators normalize as a result of weight loss in morbidly obese subjects treated with gastric restrictive surgery. J Clin Endocrinol Metab 89:4062–4068
Ruiz AG, Casafont F, Crespo J et al (2007) Lipopolysaccharide-binding protein plasma levels and liver TNF-alpha gene expression in obese patients: evidence for the potential role of endotoxin in the pathogenesis of non-alcoholic steatohepatitis. Obes Surg 17:1374–1380
Sun L, Yu Z, Ye X et al (2010) A marker of endotoxemia is associated with obesity and related metabolic disorders in apparently healthy Chinese. Diabetes Care 33:1925–1932
Gonzalez-Quintela A, Alonso M, Campos J, Vizcaino L, Loidi L, Gude F (2013) Determinants of serum concentrations of lipopolysaccharide-binding protein (LBP) in the adult population: the role of obesity. PLoS One 8:e54600
Moreno-Navarrete JM, Ortega F, Serino M et al (2012) Circulating lipopolysaccharide-binding protein (LBP) as a marker of obesity-related insulin resistance. Int J Obes (Lond) 36:1442–1449
Nakarai H, Yamashita A, Nagayasu S et al (2012) Adipocyte-macrophage interaction may mediate LPS-induced low-grade inflammation: potential link with metabolic complications. Innate Immun 18:164–170
Ge Q, Gerard J, Noel L, Scroyen I, Brichard SM (2012) MicroRNAs regulated by adiponectin as novel targets for controlling adipose tissue inflammation. Endocrinology 153:5285–5296
Giralt M, Domingo P, Guallar JP et al (2006) HIV-1 infection alters gene expression in adipose tissue, which contributes to HIV- 1/HAART-associated lipodystrophy. Antivir Ther 11:729–740
Guidone C, Manco M, Valera-Mora E et al (2006) Mechanisms of recovery from type 2 diabetes after malabsorptive bariatric surgery. Diabetes 55:2025–2031
Alligier M, Meugnier E, Debard C et al (2012) Subcutaneous adipose tissue remodeling during the initial phase of weight gain induced by overfeeding in humans. J Clin Endocrinol Metab 97:183–192
Moreno-Navarrete JM, Ortega FJ, Rodríguez-Hermosa JI et al (2011) OCT1 expression in adipocytes could contribute to increased metformin action in obese subjects. Diabetes 60:168–176
Burcelin R, Crivelli V, Dacosta A, Roy-Tirelli A, Thorens B (2002) Heterogeneous metabolic adaptation of C57BL/6J mice to high-fat diet. Am J Physiol Endocrinol Metab 282:E834–E842
Sulpice T, Prunet-Marcassus B, Molveaux C et al (2009) An adiponectin-like molecule with antidiabetic properties. Endocrinology 150:4493–4501
Medina-Gomez G, Gray SL, Yetukuri L et al (2007) PPARg2 prevents lipotoxicity by controlling adipose tissue expandability and peripheral lipid metabolism. PLos Gen 27:e64
Curat CA, Miranville A, Sengenès C et al (2004) From blood monocytes to adipose tissue-resident macrophages: induction of diapedesis by human mature adipocytes. Diabetes 53:1285–1292
Gutsmann T, Müller M, Carroll SF, MacKenzie RC, Wiese A, Seydel U (2001) Dual role of lipopolysaccharide (LPS)-binding protein in neutralization of LPS and enhancement of LPS-induced activation of mononuclear cells. Infect Immun 69:6942–6950
Bezaire V, Mairal A, Ribet C et al (2009) Contribution of adipose triglyceride lipase and hormone-sensitive lipase to lipolysis in hMADS adipocytes. J Biol Chem 284:18282–18291
Neville MJ, Collins JM, Gloyn AL, McCarthy MI, Karpe F (2011) Comprehensive human adipose tissue mRNA and microRNA endogenous control selection for quantitative real-time-PCR normalization. Obesity (Silver Spring) 19:888–892
Wurfel MM, Kunitake ST, Lichenstein H, Kane JP, Wright SD (1994) Lipopolysaccharide (LPS)-binding protein is carried on lipoproteins and acts as a cofactor in the neutralization of LPS. J Exp Med 180:1025–1035
Kirschning CJ, Au-Young J, Lamping N et al (1997) Similar organization of the lipopolysaccharide-binding protein (LBP) and phospholipid transfer protein (PLTP) genes suggests a common gene family of lipid-binding proteins. Genomics 46:416–425
Kirschning CJ, Unbehaun A, Fiedler G et al (1997) The transcriptional activation pattern of lipopolysaccharide binding protein (LBP) involving transcription factors AP-1 and C/EBP beta. Immunobiology 198:124–135
Ibrahim MM (2010) Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev 11:11–18
Vitseva OI, Tanriverdi K, Tchkonia TT et al (2008) Inducible Toll-like receptor and NF-kappaB regulatory pathway expression in human adipose tissue. Obesity (Silver Spring) 16:932–937
Gillum MP, Kotas ME, Erion DM et al (2011) SirT1 regulates adipose tissue inflammation. Diabetes 60:3235–3245
Lê KA, Mahurkar S, Alderete TL et al (2011) Subcutaneous adipose tissue macrophage infiltration is associated with hepatic and visceral fat deposition, hyperinsulinemia, and stimulation of NF-κB stress pathway. Diabetes 60:2802–2809
Suganami T, Tanimoto-Koyama K, Nishida J et al (2007) Role of the Toll-like receptor 4/NF-kappaB pathway in saturated fatty acid-induced inflammatory changes in the interaction between adipocytes and macrophages. Arterioscler Thromb Vasc Biol 27:84–91
Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS (2006) TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 116:3015–3025
Youssef-Elabd EM, McGee KC, Tripathi G et al (2012) Acute and chronic saturated fatty acid treatment as a key instigator of the TLR-mediated inflammatory response in human adipose tissue, in vitro. J Nutr Biochem 23:39–50
Huang S, Rutkowsky JM, Snodgrass RG et al (2012) Saturated fatty acids activate TLR-mediated proinflammatory signaling pathways. J Lipid Res 53:2002–2013
Acknowledgements
We acknowledge the clinical help of Oscar Rovira (Department of Endocrinology, Hospital Universitari ‘Dr Josep Trueta’, Girona, Spain) and Martin Wabitsch (Department of Pediatrics and Adolescent Medicine, Ulm University, Germany) for sharing SGBS cells. We would like to thank Pere Tubert (Laboratori d'Enginyeria de Proteïnes, Department of Biology, Facultat de Ciències, University of Girona, Girona, Spain) for his help in preparing Fig. 6.
Funding
This work was partially supported by research grants from the Ministerio de Educación y Ciencia (SAF2008-02073), European Collaborative Project ADAPT (HEALTH-F2-2008-2011 00) and the FLORINASH project. CIBERObn Fisiopatología de la Obesidad y Nutrición is an initiative by the Instituto de Salud Carlos III, Spain. AVP is funded by the Medical Research Council (MRC) and National Institute for Health Research (NIHR) Biomedical Research Centre (BRC).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
JMM-N, AZ, HV, AV-P, JV, RB and JMF-R participated in study design. JMM-N, XE, FO, MSe, MCampb, M-CM, ML, GX, EL, PDo, MSa, AW, GP, JS, MG, JIR-H, MCamps, CIK, NV, JG, PDe, FV, DL, GM, WR, GF, AZ, HV, AV-P, JV, RB and JMF-R participated substantially in data collection, analysis and drafting of the article or revising it critically for important intellectual content. JMM-N and JMF-R wrote and edited the manuscript. All authors participated in final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Research Design and Methods
PDF 370 kb
ESM Figure 1
A) FASN and Adipoq gene expression in visceral preadipocytes and adipocytes vs. subcutaneous preadipocytes and adipocytes. *p < 0.05 compared with VAT; and †p < 0.05 compared with preadipocytes; ††p < 0.01 compared with preadipocytes. B) FASN and Adipoq gene expression during subcutaneous preadipocytes differentiation from lean and obese subjects. **p < 0.01 compared with day 0; and ††p < 0.01 compared with adipocytes from lean subjects; C) LBP gene expression in isolated adipocytes, estromo-vascular cells (SVC), CD14+ and CD14− cells (n = 5) D) FASN and Adipoq gene expression and LBP protein levels during SGBS differentiation. E) FASN gene expression during 3T3-L1 differentiation. *p < 0.05 compared with day 0; **p < 0.01 compared with day 0 (PDF 58 kb)
ESM Figure 2
FASN (A), Adipoq (B) and IL-6 (C) gene expression in SAT after surgery-induced weight loss (n = 8). Comparison of PPARγ (D) and Adipoq (E) in SAT according to lipodystrophy in HIV subjects (n = 28, 7 for each group. *p < 0.05 and **p < 0.01 compared with pre-weight loss or compared with control participants; ††p < 0.05 compared with participants without lipodystrophy (PDF 25 kb)
ESM Figure 3
Effects of Rosiglitazone (10 nmol/l) on FASN (A), Adipoq (B), PPARγ (C) and Pref-1 (D) gene expression and insulin-stimulated pSer473Akt (E) and pPanTyrIRS1 (F) during 3T3-L1 differentiation at day 7. *p < 0.05 compared with vehicle; **p < 0.01 compared with vehicle. Effects of rosiglitazone (0.5 and 5 μmol/l) on ADIPOQ (G) and LEP (H) gene expression in human paired SAT and VAT explants *p < 0.05 compared with control; **p < 0.01 compared with control (PDF 14 kb)
ESM Figure 4
TNF-α (10 ng/ml) (A–C), LPS-MCM (0.5 and 5%) (D–F) effects on FASN (A, D), PPARγ (B, E) and Adipoq (C, F) gene expression during in 3T3-L1 differentiation. *p < 0.05 compared with differentiated control; **p < 0.01 compared with differentiated control (PDF 26 kb)
Rights and permissions
About this article
Cite this article
Moreno-Navarrete, J.M., Escoté, X., Ortega, F. et al. A role for adipocyte-derived lipopolysaccharide-binding protein in inflammation- and obesity-associated adipose tissue dysfunction. Diabetologia 56, 2524–2537 (2013). https://doi.org/10.1007/s00125-013-3015-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-013-3015-9