Abstract
Aims/hypothesis
This study was designed to determine whether the relationship of glycated haemoglobin to diabetic microvascular complications shows any natural thresholds that could be useful in diagnosing diabetes.
Methods
We examined a population-based sample of 3,190 Malay adults aged 40–80 years in Singapore. The microvascular outcomes of interest were: (1) any retinopathy, defined from fundus photographs; (2) mild retinopathy, defined as in (1); (3) moderate retinopathy, defined as in (1); (4) chronic kidney disease, defined from estimated glomerular filtration rate; (5) micro- or macroalbuminuria, defined from urinary albumin to creatinine ratio; and (6) peripheral neuropathy, defined from neurothesiometer or monofilament sensory testing.
Results
Increasing HbA1c was associated with all microvascular complications. The optimal cut-off points for detecting mild and moderate retinopathy were 6.6% (87.0% sensitivity, 77.1% specificity and area under the receiver operating characteristics [ROC] curve 0.899) and 7.0% (82.9% sensitivity, 82.3% specificity and area under ROC curve 0.904). The prevalences of mild and moderate retinopathy were <1% below the optimal cut-off points. For other complications, the association with HbA1c was linear without evidence of a distinct threshold. Although ROC analysis for these other complications also suggested optimal cut-off points between 6.6% and 7.0%, the sensitivity at these cut-off points was considerably lower than for mild and moderate retinopathy, ranging from 31.8% to 66.5%.
Conclusions/interpretation
Higher levels of HbA1c were associated with microvascular complications. Our data support use of an HbA1c cut-off point of between 6.6 and 7.0% in diagnosing diabetes. Cut-off points in this range were best for the identification of individuals with mild and moderate retinopathy. Any retinopathy, chronic kidney disease, albuminuria and peripheral neuropathy are less well detected at these cut-off points.
Similar content being viewed by others
Introduction
Diabetes mellitus is expected to affect 300 million people by 2025 [1]. Current diagnostic criteria for diabetes are based on the concept that microvascular complications such as retinopathy and nephropathy occur above a threshold level of hyperglycaemia that can be used to differentiate people with and without diabetes [2, 3]. Thus, the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus [2] and World Health Organization [3] have recommended the use of a fasting plasma glucose (FPG) cut-off point of 7.8 mmol/l (later lowered to 7.0 mmol/l for reasons of equivalence with the 2 h oral glucose tolerance test for diagnosing diabetes, largely based on evidence from epidemiological studies showing that retinopathy is rare below these cut-off points but that prevalence increases dramatically above them [2, 4, 5]). However, a recent meta-analysis across three different populations found no consistent FPG threshold for retinopathy, with the data instead suggesting a continuous linear relationship and poor performance of the 7.0 mmol/l FPG cut-off point in discriminating the presence of retinopathy. Such findings raise doubts about the underlying premise of a uniform glucose threshold for retinopathy [6].
Randomised controlled trials and observational studies have shown that glycated haemoglobin or haemoglobin A1c is also a good predictor of microvascular complications [5, 7–10], is highly correlated with FPG [11] and does not require measurement in the fasting state. Thus, the use of HbA1c as a diagnostic test for diabetes has been proposed [12, 13]. Several studies have examined the relationship of HbA1c to microvascular complications, but most have reported inconsistent HbA1c thresholds. These studies were limited as most examined only one or two complications in isolation [4, 5, 8, 14, 15], and all reports to date have focused on HbA1c thresholds with the presence of retinopathy. New evidence suggests the outcome of any retinopathy is not specific to diabetic microvascular complications and that a marker of more severe microvascular damage, such as moderate retinopathy, might be more useful in deriving diagnostic thresholds for diabetes [6].
Therefore we sought to examine the evidence for an HbA1c threshold in a population-based study with data on microvascular complications. We studied the relationship of HbA1c to retinopathy (any, mild and moderate), chronic kidney disease (CKD), micro- and macroalbuminuria and peripheral neuropathy to determine if a natural threshold for discriminating those with and without microvascular complications exists and, if so, what the optimal HbA1c cut-off points might be for the identification of individuals with these complications.
Methods
Study population
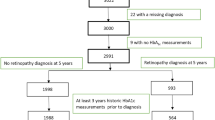
We conducted a population-based study involving 3,280 adults of Malay ethnicity aged 40–80 years in Singapore (78.7% response rate). Participants were selected using an age-stratified random-sampling method from 4,168 eligible individuals, with details of the study design and methods described previously [16]. Informed written consent was obtained from all participants, and ethics approval was obtained from the Singapore Eye Research Institute institutional review board. For this study, we excluded those with missing information on HbA1c (n = 78). Of the remaining 3,202 participants, we further excluded those with missing retinal photographs (n = 12), leaving 3,190 for the retinopathy analysis. Similarly, we further excluded those with missing information on serum creatinine (n = 69), leaving 3,133 for the CKD analysis. In addition, all participants with diabetes and approximately one in five randomly selected non-diabetic participants underwent assessment for peripheral neuropathy and had urine collected. For the former analyses, we included 885 participants with information on neurothesiometer readings and monofilament sensory tests; for the micro- and macroalbuminuria analysis, we included 930 participants who had information on urinary albumin to creatinine ratio (ACR).
Assessment of microvascular complications
Retinopathy was assessed from digital fundus photographs taken following a standardised protocol modified from the Early Treatment Diabetic Retinopathy Study (ETDRS) [16, 17]. After pupil dilation, two photographs, centred at the optic disc (ETDRS Field 1) and macula (Field 2), were taken of both eyes of each participant using a digital retinal camera (Canon CR-DGi with a 10D SLR back; Canon, Tokyo, Japan). Photographs were then sent to the University of Sydney, Australia, and mask-graded for retinopathy and other retinal diseases [18]. Intragrader reliability of retinopathy was very high with kappa statistic of 0.98 (95% CI 0.96–0.99) [18] GFR was estimated from serum creatinine concentration using the Modification of Diet in Renal Disease [MDRD] equation [19] defined as follows: \( {\text{estimated}}\;{\text{GFR}}{\left( {{\text{eGFR}}} \right)} = 186.3 \times \;{\text{serum}}\;{\text{creatinine}}{\left( {{{\text{mg}}} \mathord{\left/ {\vphantom {{{\text{mg}}} {{\text{dl}}}}} \right. \kern-\nulldelimiterspace} {{\text{dl}}}} \right)}^{{ - 1.154}} \times \;{\text{age}}^{{ - 0.203}} \times {\left( {{\text{0}}{\text{.742}}\;{\text{for}}\;{\text{women}}} \right)} \). To convert serum creatinine in mg/dl to SI units (μmol/l) multiply the value by 88.4. Serum creatinine measurement was carried out at the National University Hospital Reference Laboratory, Singapore, and was reported in μmol/l. Spot untimed urine samples were collected for measurement of albumin and creatinine. Urine albumin was measured in mg/l using a kit with a lower detection limit for albumin of 0.5 mg/l (Immulite, DPC, Llanberis, UK). Urine creatinine was measured in mmol/l using a kit that uses the Jaffe reaction (Roche Diagnostics, Mannheim, Germany) with a measuring range of 0.027–32.5 mmol/l. The ratio of urine ACR concentration expressed in mg/mmol was used to estimate total daily albumin excretion. Vibration sense was measured in V at the apex of both big toes and the medial malleoli of both ankles using a neurothesiometer (Horwell, Nottingham, UK). Monofilament sensation at five different points of each foot was tested using a Touch-test Sensory Evaluator 5.07 (North Coast Medical, Morgan Hill, CA, USA). The number of points out of five at which the participant was able to sense the fine touch was recorded.
We defined seven microvascular outcomes as follows: (1) any retinopathy (severity classified based on the worse eye), defined as a severity score of level 15 and above according to a scale graded using the ETDRS adaptation of the modified Airlie House Classification System [17, 20], which corresponds to the presence of any of the following lesions: microaneurysms, haemorrhages, cotton wool spots, intraretinal microvascular abnormalities, hard exudates, venous beading and new vessels; (2) mild retinopathy, defined as a severity score above level 20 (ETDRS > 20); (3) moderate retinopathy, defined as a severity score of level above 43 (ETDRS > 43) [17]; (4) CKD, defined as eGFR <60 ml/min/1.73 m2, consistent with US National Kidney Foundation Kidney Disease Outcome Quality Initiative working group definition [21, 22]; (5) presence of micro- or macroalbuminuria, with microalbuminuria defined as urinary ACR ≥1.9 mg/mmol for men and ≥2.8 mg/mmol for women, and macroalbuminuria as ACR ≥28 mg/mmol for men and ≥40 mg/mmol for women [21]; (6) peripheral neuropathy, defined as either neurothesiometer reading >25 V [23, 24] or monofilament sensory test result below four out of five points on either side of the feet [25].
Exposure measurement
All participants had 40 ml venous blood drawn and collected in plain and fluoride oxalate tubes and stored at 4°C for a maximum of 4 h prior to processing. Serum total cholesterol, LDL- and HDL-cholesterol, triacylglycerol, serum creatinine, HbA1c and casual plasma glucose were measured at the National University Hospital Reference Laboratory, which is accredited by the College of American Pathologists. The HbA1c assay was carried out using an HPLC cation exchange chromatography system implemented on a Biorad variant II analyser (Bio-Rad Laboratories, Hercules, CA, USA). The assay was accredited by the National Glycoprotein Standardization Program with controls traceable to the DCCT.
Information on cigarette smoking, alcohol consumption and medical history was obtained using a standardised questionnaire administered by trained personnel. Blood pressure was measured with a digital automatic blood pressure monitor after participants had been seated for at least 5 min. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic pressure ≥90 mmHg or self-reported physician-diagnosed hypertension. Diabetes mellitus was defined as a casual plasma glucose ≥11.1 mmol/l or self-reported physician-diagnosed diabetes or use of glucose-lowering medication. Body mass index was calculated as weight in kilograms divided by the square of height in meters (kg/m2). Participants were considered non-drinkers if their answer was negative to the question, ‘How often do you have an alcoholic drink?’ and drinkers if their answer was affirmative, irrespective of frequency and quantity. Cigarette smoking was categorised into current smoker, ex-smoker or non-smoker.
Statistical analysis
All statistical analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC, USA). We compared selected baseline characteristics of the cohort by HbA1c status, employing the χ 2 test or analysis of variance, as appropriate. We cross-tabulated the prevalence of any retinopathy, mild retinopathy, moderate retinopathy, CKD, micro- or macroalbuminuria and peripheral neuropathy at different HbA1c cut-off points ranging from 5.6% to 8.0% and calculated sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios. We plotted the frequency of any, minimal, mild and moderate retinopathy against HbA1c in intervals chosen to include 6.1% and 7.0%. We examined these plots visually for evidence of an HbA1c threshold above which the prevalence of any, mild and moderate retinopathy increased. We tested statistically for thresholds using change-point models, which assume a constant prevalence below the change point and a linear association above [8, 26]. To assess performance of HbA1c in discriminating microvascular complications, we plotted receiver operating characteristic (ROC) curves and estimated the area under the curve (using the web-based calculator for ROC curves available from Johns Hopkins University, Baltimore, MD, USA [www.jrocfit.org, accessed 30 April 2008]). Finally we used logistic regression models to calculate the odds ratio and 95% confidence interval of the six microvascular complications across different cut-off points of HbA1c using the lowest cut-off point as reference category in two separate models. In the first model we adjusted for age (years) and sex and in the multivariable model we additionally adjusted for body mass index (kg/m2), current smoking (absent, present), hypertension status (absent, present) and HDL-cholesterol (mmol/l). We performed tests for trends using the categories of HbA1c as ordinal variables in multivariable logistic regression models.
Results
The baseline characteristics of the study participants are presented in Table 1. Compared with those with HbA1c <7%, those with HbA1c ≥7.0% were significantly older, were less likely to be current smokers or drinkers, and had higher body mass index, casual plasma glucose and systolic blood pressure.
The prevalence of any retinopathy was 12.9%, mild retinopathy 5.6%, moderate retinopathy 3.9%, CKD 21.3%, micro- or macroalbuminuria 37.2% and peripheral neuropathy 21.2%. Table 2 shows the relationship between HbA1c and microvascular complications. Increasing HbA1c categories had a higher prevalence of any retinopathy, mild retinopathy, moderate retinopathy, CKD, micro or macroalbuminuria and peripheral neuropathy in a dose-dependent manner (p trend<0.0001 for any retinopathy, mild retinopathy, moderate retinopathy, CKD, micro- or macroalbuminuria and p trend=0.02 for peripheral neuropathy). In the multivariable models, HbA1c categories above 7.0% were significantly associated with increased prevalence of microvascular complications compared with the lowest category. In particular, persons with HbA1c in the range 7.0–7.9% and ≥8.0% had ninefold and 30-fold higher prevalences of mild and moderate retinopathy than persons with HbA1c ≤6.9%. The positive association between HbA1c and the six microvascular complications persisted when HbA1c was analysed as a continuous variable. Fig. 1 shows the cross-sectional frequency distribution of any retinopathy, mild retinopathy and moderate retinopathy by HbA1c categories. Prevalence of any, mild and moderate retinopathy increased with increasing levels of HbA1c. The prevalence of any retinopathy at lower levels of HbA1c was about 5% while the prevalence of mild and moderate retinopathy was almost 0% below an HbA1c of 6.0%.
Table 3 shows the prevalence of any retinopathy, mild retinopathy, moderate retinopathy, CKD, micro- or macroalbuminuria and peripheral neuropathy above and below the various cut-off points of HbA1c and their corresponding sensitivities, specificities, positive and negative predictive values and positive and negative likelihood ratios. The prevalence of any retinopathy below the HbA1c cut-off point of 7.0% was 7.2% and above the cut-off point it was 35.4%. The sensitivity of this cut-off point for detecting any retinopathy was 55.6%, with specificity of 85.0%. The positive predictive value at this cut-off point was low (35.4%), but the negative predictive value was high (92.9%). A higher cut-off point (8.0%) improved specificity, positive predictive value and positive likelihood ratio, but reduced sensitivity with largely unchanged negative predictive value and negative likelihood ratio. A lower cut-off point at 6.1% increased sensitivity, but reduced specificity, positive predictive value and positive likelihood ratio. The prevalences of mild and moderate retinopathy were 1.3% and 0.8% below the HbA1c cut-off point of 7.0%, and 22.5% and 15.8% above the cut-off point, respectively. The sensitivity and specificity of HbA1c cut-off point 7.0% in detecting mild and moderate retinopathy was higher (>80%) compared with other microvascular complications. The performance of HbA1c was generally poor for other microvascular complications with prevalence of the complications ranging from 11.8% to 23.9% even at the lowest cut-off point of HbA1c (5.6%). In change-point models, a continuous relationship was observed between HbA1c and any retinopathy, mild retinopathy, moderate retinopathy, CKD, micro- or macroalbuminuria and peripheral neuropathy without a threshold effect.
Figure 2 compares the ROC curves for HbA1c and all six microvascular complications. The AUC for any retinopathy was 0.754, mild retinopathy 0.899, moderate retinopathy 0.904 and for other microvascular complications ranged from 0.573 to 0.673. Based on the ROC and the diagnostic value of the different cut-off points, the optimal cut-off point was found to be 7.0% for any retinopathy, moderate retinopathy and micro- or macroalbuminuria, and 6.6% for mild retinopathy, CKD and peripheral neuropathy (Table 4).
ROC curves for HbA1c (%) and the various microvascular complications. AUC for any retinopathy (dark blue line) 0.754; AUC for mild retinopathy 0.899 (dashed red line); AUC for moderate retinopathy (green line) 0.904; AUC for chronic kidney disease (light blue line) 0.615; AUC for micro- and macroalbuminuria (pink line) 0.673; AUC for peripheral neuropathy (brown line) 0.573
We performed several supplementary analyses. First, we repeated the analysis for any, mild and moderate retinopathy in Table 3 after excluding those on glucose-lowering medications (n = 2,588 included). The results remained similar to our main analyses in Table 3. For example, the sensitivity of HbA1c cut-off point of 7.0% for detecting any retinopathy decreased to 19.8%, with specificity of 93.0%, while sensitivities for detecting mild and moderate retinopathy decreased to 65.0% and 66.7% with specificities of 92.5% and 92.4%. In a second supplementary analysis, we evaluated the association between hypertension and lipids with any, mild and moderate retinopathy in participants without diabetes. Hypertension (p = 0.01) and low HDL (p = 0.04) were significantly associated with any retinopathy in the absence of diabetes although mild (p = 0.96 for hypertension and p = 0.15 for HDL) and moderate retinopathy were not (p = 0.96 for hypertension and p = 0.29 for HDL). Fourth, we repeated the Table 3 and ROC curve analyses using casual plasma glucose and obtained results essentially similar to those with HbA1c. For example, the prevalence of any retinopathy below a casual plasma glucose cut-off point of 11.1 mmol/l (cut-point for diagnosing diabetes) was 39.9%, with 9.7% prevalence above this cut-off point. The sensitivity of this cut-off point for detecting any retinopathy was 32.3%, specificity was 92.8% and the area under curve was 0.727. The prevalences of mild and moderate retinopathy below this cut-off point were 2.9% and 1.9%, respectively, while above this cut-off point they were 27.3% and 19.9%. Similar to the HbA1c cut-off point of 7.0%, a casual plasma glucose cut-off point of 11.1 mmol/l had the same specificities (92.0% and 91.4%) but with improved sensitivities (52.1% and 54.6%) and larger areas under ROCs (0.849 and 0.863) for mild and moderate retinopathy, respectively, compared with any retinopathy. Finally, we evaluated the performance of HbA1c in detecting macroalbuminuria. Macroalbuminuria was detected in 4.8% of the study population and an HbA1c cut-off point of 7.0% had improved sensitivity (46.7%), moderate specificity (83.7%) and a larger area under the curve (0.722) for detecting macroalbuminuria compared with micro- or macroalbuminuria (data not shown).
Discussion
HbA1c is an index of mean blood glucose in fasting and postprandial state [27], and is well established and widely used as a clinical measure of chronic glycaemia [28]. Several studies indicate that HbA1c may show a glycaemic threshold with microvascular complications, suggesting it may additionally be useful as a diagnostic test for diabetes [12, 29]. In this population-based study of over 3,000 middle-aged individuals, we found a linear continuous relationship of HbA1c with microvascular complications including any retinopathy, mild retinopathy, moderate retinopathy, CKD, micro- or macroalbuminuria and peripheral neuropathy. We found no evidence for a threshold effect of HbA1c with any retinopathy, micro- or macroalbuminuria, CKD and peripheral neuropathy. However, there was a clear difference in the relationship of HbA1c to mild and moderate retinopathy compared with other microvascular complications (any retinopathy, albuminuria, CKD and peripheral neuropathy). Mild and moderate retinopathy were rare below HbA1c 6.6–7.0% and the prevalence increased 16–17-fold above this level of HbA1c. For mild and moderate retinopathy, the areas under ROC curves for HbA1c were 0.899 and 0.904 and the optimal cut-off points maximising sensitivity and specificity were 6.6% and 7.0%. Several other observations support the validity of using mild and moderate retinopathy, rather than any retinopathy, as specific glycaemic markers for diabetes—the almost complete absence of mild and moderate retinopathy below an HbA1c level of 6.6–7.0%, and the lack of association of hypertension and dyslipidaemia with mild and moderate retinopathy. In contrast, prevalences of microvascular complications other than mild and moderate retinopathy were high below HbA1c 7.0% (7.2% for any retinopathy, 18.8% for CKD, 30.9% for micro- or macroalbuminuria and 17.6% for peripheral neuropathy). Analysis of the ROC curves suggested that an HbA1c cut-off point of between 6.6 and 7.0% optimised sensitivity and specificity for identifying individuals with these other complications, consistent with the optimal cut-off points identified for mild and moderate retinopathy. However, sensitivity at these optimal cut-off points was considerably lower than for mild and moderate retinopathy, ranging from 31.8% to 66.5% depending on the complication.
The HbA1c thresholds for increasing prevalence of any retinopathy were reported to be between 6.1% and 7.0% in studies conducted among different ethnic groups [2, 4, 5, 8]. Few epidemiological studies have examined the optimal cut-off points for HbA1c that maximise sensitivity and specificity. In Pima Indians, the optimal HbA1c cut-off point of 7.0% had 78.1% sensitivity and 84.7% specificity for detecting any retinopathy [5]. In the Hisayama study, the optimal HbA1c cut-off point of 5.7% was reported to have a sensitivity of 86.5% with a specificity of 90.1% [14]. The variability in optimal cut-off points could be due to assay differences in measuring HbA1c. Other reasons for the variability in optimal cut-off points could be the different ethnicities, age and sex distribution and prevalence of diabetes [29]. It should be noted that the Meta-analysis Research Group on the Diagnosis of Diabetes Using Glycated Hemoglobin levels has recommended an HbA1c cut-off point of ≥7.0% [30], which agrees well with our findings.
Our findings of a continuous relationship of HbA1c to microvascular complications without any evidence of a clear threshold effect for most of the microvascular complications examined is consistent with a recent meta-analysis that showed a similar lack of fasting glucose thresholds with retinopathy [6]. Other studies have also documented a continuous association between FPG and CKD [31], microalbuminuria [32] and peripheral neuropathy [33, 34]. Taken together, these results argue against the existence of glycaemic thresholds for the majority of microvascular complications. Given the lack of a distinct glycaemic threshold for most microvascular complications, it is not surprising that the areas under the ROC curves were modest, ranging from 0.573 for peripheral neuropathy to 0.754 for any retinopathy.
Several factors could explain these findings. First, any retinopathy [6, 35–37], and nephropathy [38, 39] may also occur in persons without diabetes as these outcomes are related to non-glycaemic processes such as age, obesity, dyslipidaemia and hypertension [40, 41], which are very common in the population. As such, it should not be surprising that some of these complications that are not specific to hyperglycaemia are seen at the relatively low levels of glycaemia observed in this study. Second, HbA1c was measured at a single time-point, and we did not collect information on previous glycaemia levels, which have been shown to have an impact on the risk of microvascular complications [42–44] and may influence the prevalence of microvascular complications. Unlike in trials of intensive glycaemic control, most of our participants with HbA1c below 7.0% did not have previously diagnosed diabetes (7% had previously diagnosed diabetes below HbA1c = 7%) and were therefore not receiving pharmacological treatment or even therapeutic lifestyle modification to lower blood glucose. We do not believe that, in these circumstances, large changes in glycaemia are likely to have occurred prior to their participation in this study, certainly not of the magnitude seen in the interventional trials. Furthermore, excluding participants on glucose-lowering medication did not change our results appreciably.
The main strengths of our study are its population-based sample, our precise estimation of any, mild and moderate retinopathy, and the inclusion of data on other microvascular endpoints collected using standardised protocols. In addition, HbA1c was measured according to internationally accepted standards.
Limitations of this study should also be noted. First, we did not have information on FPG, and were unable to compare the performance of HbA1c against FPG as a diagnostic test for diabetes. This was not the aim of the study and requires further investigation. Second, we took a single measurement of HbA1c, which could potentially misclassify chronic glucose exposure. We obtained similar results with an alternative glycaemic measure (casual plasma glucose) suggesting this potential misclassification would not have influenced our conclusions. Third, this was a cross-sectional study and we are thus unable to determine the relationship of HbA1c to incident microvascular outcomes. Follow-up of the study population is currently in progress. Fourth, we examined micro- and macroalbuminuria and peripheral neuropathy in only a sample of participants. Fifth, we obtained photographs of two central retinal fields, which is less sensitive than using seven retinal fields; however, this is unlikely to introduce much bias as most diabetic retinopathy, particular mild and moderate retinopathy, occurs in those two fields [45]. Finally, the study was performed in a homogeneous Malay population, and requires confirmation in other ethnic groups and more ethnically heterogeneous populations. However, the racial homogeneity of the study population offers the advantage of precluding confounding by race.
The current American Diabetes Association and WHO guidelines for diagnosing diabetes do not take HbA1c into account and are based on FPG, casual blood glucose and OGTTs. This is despite the many advantages to using HbA1c over other glycaemic measures such as less intra-individual variation [29], good ability to detect undiagnosed diabetes [46, 47] and predict risk of developing microvascular complications both in type 1 and type 2 diabetes [9, 10, 48], and widespread acceptance as a common endpoint in clinical trials. Our study suggests that HbA1c may be a useful measure for diagnosing diabetes and supports a possible cut-off point at between 6.6% and 7.0%, which is in line with current recommendations [12, 13, 30, 47]. It should, however, be noted that thresholds within this range are particularly useful for the identification of mild and moderate retinopathy rather than other complications. This may be appropriate for the prevention of retinal disease associated with hyperglycaemia as previous longitudinal studies conducted in diabetic patients have demonstrated little development or progression of retinopathy or overt proteinuria if mean HbA1c level is maintained below 7.0% [48–50]. Thus, failure to detect a significant proportion of individuals with earlier forms of retinopathy may not be critical to the prevention of visual loss, as long as HbA1c remains below 7.0%. With regards to the other microvascular complications associated with hyperglycaemia, it appears that there is poor, or limited, support for a discrete inflection point that can be used for diagnostic purposes. However, high HbA1c levels were still positively associated with microvascular complications (e.g. those with an HbA1c level above 8% were seven times as likely to have micro- or macroalbuminuria than those with an HbA1c below 6%). An area of future research is comparing the performance of HbA1c with that of other measures of glycaemia such as FPG or oral glucose tolerance test in dichotomising these microvascular complications.
In conclusion, we report a continuous linear association between HbA1c and microvascular complications, including any, mild and moderate retinopathy, CKD, micro- and macroalbuminuria and peripheral neuropathy without any clear and consistent threshold effect across the different outcomes. Despite the lack of an abrupt threshold, HbA1c cut-off points in the range 6.6 to 7.0% were optimal for detecting microvascular complications and performed well at discriminating presence of mild and moderate retinopathy. Together with the significant advantages of HbA1c over other glycaemic measures, for example, no requirement of fasting, less variability, consistent associations with micro- and macrovascular complications, and improved international standardisation of measurement, our data support use of an HbA1c cut-off point between 6.6% and 7.0% in diagnosing diabetes. However, it will be important to examine the impact of using alternative tests of glycaemia, or other diagnostic strategies, to identify those with microvascular complications. The public health impact of such strategies should also be carefully examined as the detection of these complications early will have an impact on healthcare resource use and the benefits of such early detection must be clearly delineated.
Abbreviations
- ACR:
-
Albumin to creatinine ratio
- CKD:
-
Chronic kidney disease
- eGFR:
-
Estimated glomerular filtration rate
- ETDRS:
-
Early Treatment Diabetic Retinopathy Study
- FPG:
-
Fasting plasma glucose
- MDRD:
-
Modification of Diet in Renal Disease
- ROC:
-
Receiver operating characteristic
References
King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 21:1414–1431
Anonymous (2003) Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 26(Suppl 1):S5–S20
World Health Organization (2008) Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. Available from www.who.int/diabetes/publications/en/, accessed 5 August 2008
Engelgau MM, Thompson TJ, Herman WH et al (1997) Comparison of fasting and 2-hour glucose and HbA1c levels for diagnosing diabetes. Diagnostic criteria and performance revisited. Diabetes Care 20:785–791
McCance DR, Hanson RL, Charles MA et al (1994) Comparison of tests for glycated haemoglobin and fasting and two hour plasma glucose concentrations as diagnostic methods for diabetes. BMJ 308:1323–1328
Wong TY, Liew G, Tapp RJ et al (2008) Relation between fasting glucose and retinopathy for diagnosis of diabetes: three population-based cross-sectional studies. Lancet 371:736–743
American Diabetes Association (2007) Standards of medical care in diabetes–2007. Diabetes Care 30:S4–S41
Tapp RJ, Zimmet PZ, Harper CA et al (2006) Diagnostic thresholds for diabetes: the association of retinopathy and albuminuria with glycaemia. Diabetes Res Clin Pract 73:315–321
Anonymous (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The diabetes control and complications trial research group. N Engl J Med 329:977–986
Anonymous (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 352:837–853
Ito C, Maeda R, Ishida S, Sasaki H, Harada H (2000) Correlation among fasting plasma glucose, two-hour plasma glucose levels in OGTT and HbA1c. Diabetes Res Clin Pract 50:225–230
Saudek CD, Herman WH, Sacks DB, Bergenstal RM, Edelman D, Davidson MB (2008) A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab 93:2447–2453
Barr RG, Nathan DM, Meigs JB, Singer DE (2002) Tests of glycemia for the diagnosis of type 2 diabetes mellitus. Ann Intern Med 137:263–272
Miyazaki M, Kubo M, Kiyohara Y et al (2004) Comparison of diagnostic methods for diabetes mellitus based on prevalence of retinopathy in a Japanese population: the Hisayama Study. Diabetologia 47:1411–1415
Klein R, Klein BE, Moss SE (1996) Relation of glycemic control to diabetic microvascular complications in diabetes mellitus. Ann Intern Med 124:90–96
Foong AW, Saw SM, Loo JL et al (2007) Rationale and methodology for a population-based study of eye diseases in Malay people: the Singapore Malay Eye Study (SiMES). Ophthalmic Epidemiol 14:25–35
Wong TY, Cheung N, Tay WT et al (2008) Prevalence and risk factors for diabetic retinopathy the Singapore Malay Eye Study. Ophthalmology 15:1869–1875
Mitchell P, Smith W, Wang JJ, Attebo K (1998) Prevalence of diabetic retinopathy in an older community. The Blue Mountains Eye Study. Ophthalmology 105:406–411
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470
Anonymous (1991) Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 98:786–806
Anonymous (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1–266
Shankar A, Leng C, Chia KS et al (2008) Association between body mass index and chronic kidney disease in men and women: population-based study of Malay adults in Singapore. Nephrol Dial Transplant 23:1910–1918
Young MJ, Every N, Boulton AJ (1993) A comparison of the neurothesiometer and biothesiometer for measuring vibration perception in diabetic patients. Diabetes Res Clin Pract 20:129–131
O'Neill J, McCann SM, Lagan KM (2006) Tuning fork (128 Hz) vs neurothesiometer: a comparison of methods of assessing vibration sensation in patients with diabetes mellitus. Int J Clin Pract 60:174–178
Kumar S, Fernando DJ, Veves A, Knowles EA, Young MJ, Boulton AJ (1991) Semmes-Weinstein monofilaments: a simple, effective and inexpensive screening device for identifying diabetic patients at risk of foot ulceration. Diabetes Res Clin Pract 13:63–67
Ulm K (1991) A statistical method for assessing a threshold in epidemiological studies. Stat Med 10:341–349
Nathan DM, Turgeon H, Regan S (2007) Relationship between glycated haemoglobin levels and mean glucose levels over time. Diabetologia 50:2239–2244
Saudek CD, Derr RL, Kalyani RR (2006) Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. JAMA 295:1688–1697
Bennett CM, Guo M, Dharmage SC (2007) HbA(1c) as a screening tool for detection of Type 2 diabetes: a systematic review. Diabet Med 24:333–343
Peters AL, Davidson MB, Schriger DL, Hasselblad V (1996) A clinical approach for the diagnosis of diabetes mellitus: an analysis using glycosylated hemoglobin levels. Meta-analysis research group on the diagnosis of diabetes using glycated hemoglobin levels. JAMA 276:1246–1252
Fox CS, Larson MG, Leip EP, Meigs JB, Wilson PW, Levy D (2005) Glycemic status and development of kidney disease: the Framingham Heart Study. Diabetes Care 28:2436–2440
Mykkanen L, Haffner SM, Kuusisto J, Pyorala K, Laakso M (1994) Microalbuminuria precedes the development of NIDDM. Diabetes 43:552–557
Ziegler D, Rathmann W, Dickhaus T, Meisinger C, Mielck A (2008) Prevalence of polyneuropathy in pre-diabetes and diabetes is associated with abdominal obesity and macroangiopathy: the MONICA/KORA Augsburg Surveys S2 and S3. Diabetes Care 31:464–469
Polydefkis M, Griffin JW, McArthur J (2003) New insights into diabetic polyneuropathy. JAMA 290:1371–1376
Chao JR, Lai MY, Azen SP, Klein R, Varma R (2007) Retinopathy in persons without diabetes: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci 48:4019–4025
Wong TY, Barr EL, Tapp RJ et al (2005) Retinopathy in persons with impaired glucose metabolism: the Australian Diabetes Obesity and Lifestyle (AusDiab) study. Am J Ophthalmol 140:1157–1159
Kawasaki R, Wang JJ, Wong TY, Kayama T, Yamashita H (2008) Impaired glucose tolerance, but not impaired fasting glucose, is associated with retinopathy in Japanese population: the Funagata study. Diabetes Obes Metab 10:514–515
Gerstein HC, Pogue J, Mann JF et al (2005) The relationship between dysglycaemia and cardiovascular and renal risk in diabetic and non-diabetic participants in the HOPE study: a prospective epidemiological analysis. Diabetologia 48:1749–1755
Haffner SM, Gonzales C, Valdez RA et al (1993) Is microalbuminuria part of the prediabetic state? The Mexico City Diabetes Study. Diabetologia 36:1002–1006
Yu T, Mitchell P, Berry G, Li W, Wang JJ (1998) Retinopathy in older persons without diabetes and its relationship to hypertension. Arch Ophthalmol 116:83–89
Miljanovic B, Glynn RJ, Nathan DM, Manson JE, Schaumberg DA (2004) A prospective study of serum lipids and risk of diabetic macular edema in type 1 diabetes. Diabetes 53:2883–2892
Anonymous (2002) Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA 287:2563–2569
Anonymous (2003) Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the Epidemiology of Diabetes Interventions and Complications (EDIC) study. JAMA 290:2159–2167
Gaede P, Lund-Andersen H, Parving HH, Pedersen O (2008) Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358:580–591
Moss SE, Meuer SM, Klein R, Hubbard LD, Brothers RJ, Klein BE (1989) Are seven standard photographic fields necessary for classification of diabetic retinopathy? Invest Ophthalmol Vis Sci 30:823–828
Edelman D, Olsen MK, Dudley TK, Harris AC, Oddone EZ (2004) Utility of hemoglobin A1c in predicting diabetes risk. J Gen Intern Med 19:1175–1180
Rohlfing CL, Little RR, Wiedmeyer HM et al (2000) Use of GHb (HbA1c) in screening for undiagnosed diabetes in the U.S. population. Diabetes Care 23:187–191
Anonymous (1995) The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes 44:968–983
Ohkubo Y, Kishikawa H, Araki E et al (1995) Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract 28:103–117
Warram JH, Scott LJ, Hanna LS et al (2000) Progression of microalbuminuria to proteinuria in type 1 diabetes: nonlinear relationship with hyperglycemia. Diabetes 49:94–100
Acknowledgements
The authors thank the staff and participants in the Singapore Malay Eye Study for their important contributions. The authors also thank P. Chen, Department of Statistics and Applied Probability, National University of Singapore, for her help with the figures. This study was supported by National Medical Research Council grants 0796/2003, IRG07nov013 and STaR/0003/2008.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sabanayagam, C., Liew, G., Tai, E.S. et al. Relationship between glycated haemoglobin and microvascular complications: Is there a natural cut-off point for the diagnosis of diabetes?. Diabetologia 52, 1279–1289 (2009). https://doi.org/10.1007/s00125-009-1360-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-009-1360-5