Abstract
Aims/hypothesis
The spontaneously diabetic Torii (SDT) rat has recently been established as a model of type 2 human diabetes mellitus. Male SDT rats develop severe diabetic ocular complications. This study investigated the nature of the ocular complications in this model and addressed the question of whether the SDT rat is a good model of human proliferative diabetic retinopathy.
Methods
Male SDT rats aged 50 weeks were studied for a period of 8 months. Under deep anaesthesia, one eye of each animal was enucleated following perfusion with fluorescein dextran and a retinal flat mount was prepared to study vascular structure. The other eye was enucleated and investigated histologically by haematoxylin–eosin and azan staining and by immunohistochemistry using antibodies against vascular endothelium (Griffonia simplicifolia isolectin B4 antibody) and vascular endothelial growth factor (VEGF).
Results
From the vascular structure study, 17 of 32 rats (53%) showed proliferative retinopathy without vascular non-perfusion. The histological study revealed traction retinal folds in rats with proliferative retinopathy. Azan staining showed some proliferative matrix in rats with normal retinal structure and those with proliferative retinopathy compared with normoglycaemic controls. Staining with Griffonia simplicifolia isolectin B4 antibody showed no specific vascular changes in any of the rats, while VEGF staining revealed higher immunoreactivity in the retina of rats with normal retinal structure and those with proliferative retinopathy, but only low immunoreactivity in the control animals.
Conclusions/interpretation
There appear to be differences between the SDT rat model of diabetic retinopathy and human proliferative diabetic retinopathy, as the SDT rat develops retinal neovascularisation without retinal ischaemia. This very unique display of ocular neovascularisation may be caused by increased expression of VEGF.
Similar content being viewed by others
Introduction
To provide valuable information on the pathogenesis of human diabetic retinopathy, several animal models of diabetic retinopathy have been established. Despite many attempts to establish suitable models that accurately reflect the human condition, there are very few animal models that develop severe diabetic retinopathy with large areas of retinal non-perfusion and retinal neovascularisation [1–3]. In dog models of diabetic retinopathy, it is necessary to wait at least 5 years before severe retinopathy accompanied by retinal neovascularisation is observed [2]. Rodent models are generally preferred for the following reasons: (1) they have a similar genetic background to humans; (2) various experimental tools, including antibodies to certain peptides, are widely available; (3) they have short reproductive cycles; and (4) the animals are easy to handle. Several kinds of rodent model are now available for research into diabetes mellitus. These include the BioBreeding rat [4], the streptozotocin (STZ) rat or alloxan-induced diabetic rat [5] and the non-obese diabetic mouse [6] as models of type 1 diabetes, and the Zucker diabetic fatty rat [7], the BHE (Bureau of Home Economics) rat [8], the Otsuka–Long–Evans–Tokushima fatty rat [9] and the diet-induced diabetic rat or mouse as models of type 2 diabetes. Although the majority of these models develop significant diabetic retinal microvascular lesions, none have severe retinal changes such as pre-retinal neovascularisation or extensive areas of retinal reperfusion [10].
The spontaneously diabetic Torii (SDT) rat is an inbred rat strain established recently from a colony of normal Sprague–Dawley rats [11]. Male SDT rats develop hyperglycaemia spontaneously without obesity at 20 weeks of age, with an incident rate reaching 100% at 40 weeks of age. As a result, the animals develop severe ocular complications such as cataracts, retinal neovascularisations and retinal detachment, which are similar to the diabetic ocular complications seen in humans [11].
To assess whether the SDT rat is a suitable animal model of human proliferative diabetic retinopathy we compared the nature of retinal neovascularisation in these rats with that of the human condition, focusing on the relationship between vascular endothelial growth factor (VEGF) and retinal vascular changes.
Materials and methods
Animals
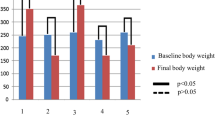
The SDT rats used in this study were male and were aged 50 weeks, as only male animals were supplied from the animal control centre of the SDT rat study group (Torii Pharmaceutical Company, Tokyo, Japan) and we had to wait 50 weeks until all the animals had a blood glucose level of above 2.22 mmol/L. All the rats were confirmed as having diabetes mellitus by checking that their serum blood glucose was above 2.22 mmol/L. A total of 50 ‘diabetic’ SDT rats were housed in the animal facility at Kansai Medical University with a room temperature of 22°C, humidity levels of 20–30% and controlled lighting automatically set to a diurnal rhythm. The wood-chip carpet and drinking water in the cages were changed daily to improve hygiene conditions and prevent infection. Blood sugar concentration was checked monthly. After 8 months all the rats were killed. Under deep ether anaesthesia, one eye from each rat was enucleated, immediately frozen using liquid nitrogen, and embedded in optimal cutting temperature compound. The rats were then perfused with fluorescein dextran for a flat mount vascular structure study. During the 8-month observation period we came across an SDT rat strain from another colony group that remained normoglycaemic. These rats were used as age-matched controls for the flat mount and histological studies.
The study was performed in accordance with the ARVO (Association for Research in Vision and Ophthalmology) Resolution on the Use of Animals in Research.
Histology and immunohistochemistry
Frozen 10-µm sections were taken from the eyes of the SDT rats and stained with haematoxylin and eosin (HE) staining, Azan staining and immunohistochemically with antibodies including biotinylated Griffonia simplicifolia isolectin B4 (GSA; Vector Laboratories, Burlingame, CA, USA) and anti-VEGF (Santa Cruz Biotechnology, Santa Cruz, CA, USA). For immunohistochemistry staining, the slides were fixed in 4% paraformaldehyde-PBS (pH 7.4) for 10 min, and washed with 0.05 mol/l PBS. The slides were then incubated for 30 min in ice-cold methanol/H2O2, washed with PBS and incubated for 30 min in 10% normal swine serum. After excess serum was removed from the slides, they were incubated for 12 h at 4°C with each antibody. After rinsing with Tris-buffered saline, the slides were incubated for 30 min at room temperature with biotin-conjugated goat anti-mouse or anti-rat antibody (DakoCytomation, Glostrup, Denmark). For the anti-GSA staining, this incubation was omitted as the antibody was already biotin conjugated. The slides were then rinsed with PBS and incubated for 30 min at room temperature with avidin coupled to peroxidase (DakoCytomation). After washing with PBS for a further 10 min, the slides were colourised with Simple Stain AEC (Nichirei) to give a red reaction product, and mounted with Aqua Poly/Mount (Polysciences, Warrington, PA, USA).
Preparation of retinal flat mounts
The rats were deeply anaesthetised using ether, and the descending aorta was clamped and the right atrium cut. This was followed by infusion of 3 ml PBS containing 50 mg/ml fluorescein-labelled dextran (average molecular weight: 2×106; Sigma, St Louis, MO, USA) through the left ventricle. This procedure was similar to that described previously by Smith et al. in a mouse model [12]. The eyes were then fixed for 1 h in 10% buffered formalin followed by separation and excision of the cornea, lens and retina with the aid of a microscope. The retinae were cut radially from the edge to the equator, with several incisions made in each eye, and then flat mounted in Aqua Poly/Mount with the vitreous side facing upwards. The flat mounts were examined using a fluorescent microscope (BH-2; Olympus, Tokyo, Japan), and the images were downloaded onto a computer and printed using a Pictrostat 3000 photoprinter (Fuji Photo Film, Tokyo, Japan).
Results
In the retinal flat mount study, 32 of the 40 rats survived the 8-month observation period. In the flat mount vascular structure study, 17 of the 32 (53%) had vascular abnormalities including retinal folds and neovascularisation (Fig. 1). On the basis of these results, we classified the SDT rats as follows: (1) normoglycaemic controls (SDT-control rats, Fig. 1a); (2) rats with normal retinal structure (SDT-NRS rats, Fig. 1b); or (3) rats with proliferative retinopathy (SDT-PR rats, Fig. 1c). In the SDT-PR rats, all the retinal neovascularisation originated from the optic disc and extended to the peripheral retina, with several of the rats having distorted and elevated retina. No abnormalities were observed in the vascular structure of the peripheral retina. The SDT-control and SDT-NRS rats also had no vascular abnormalities. All the SDT-NRS and SDT-PR rats developed mature cataracts, whereas no cataract formation was observed in the SDT-control animals. The cataracts in the SDT rats were too well developed to allow observation of the fundi using an ophthalmoscope. None of the SDT rats were found to have visible bleeding in the anterior chamber or to have developed a phthisis bulbi. In addition, no vascular non-perfusion, bleeding, or hard or soft exudates were observed in the flat-mount preparations of retinae in the SDT rats. There was no statistically significant difference in blood glucose levels between SDT-NRS (3.46±0.34 mmol/L) and SDT-PR (3.25±0.52 mmol/L) rats following a t-test.
Montage photograph of fluorescein-perfused flat mounts from the retinae of SDT rats. a Normoglycaemic SDT rat (SDT-control). These animals were used as control animals in this study. b Hyperglycaemic SDT rat with normal retinal structure (SDT-NRS). No vascular abnormalities were observed, including retinal folds, vascular occlusion or neovascularisation. c Hyperglycaemic SDT rat with massive vascular proliferation (SDT-PR). Although there is no area of vascular non-perfusion in the peripheral retina, there is massive progression of vascular proliferation originating from the optic disc area. The retina has traction from the proliferative membrane and several retinal folds have formed around the optic disc
Staining with haematoxylin–eosin showed the same retinal structure in SDT-control and SDT-NRS rats (Fig. 2a,b). In the SDT-PR rats we observed tractional retinal changes without retinal detachment (Fig. 2c), with the retina being distorted in a similar way to that in human diabetic tractional retinal changes. However, examination of the peripheral retina, where the retina was not involved in tractional change, showed normal results (Fig. 2d). Azan staining revealed that some proliferative matrix, while not clearly seen in haematoxylin–eosin staining, was markedly present in SDT-NRS and SDT-PR rats (Fig. 2e,f). The proliferative tissue, especially in the SDT-PR rats, originated from the optic disc and adhered to the mid-peripheral retina and posterior pole of the lens (Fig. 2g,h). GSA staining showed no particular vascular changes in the SDT-control and SDT-NRS rats (Fig. 2i,j), whereas there were some GSA-positive cells located in the proliferative tissue in the SDT-PR rats (Fig. 2k). VEGF staining revealed a low level of immunoreactivity in the retinae of SDT-control rats in contrast to a high degree of immunoreactivity in the ganglion cell layer, the inner nuclear layer and the border between the outer nuclear layer and the outer segment of photoreceptors in the SDT-NRS and SDT-PR rats (Fig. 2l–r). We observed high VEGF immunoreactivity in vascular endothelial cells in the SDT-PR rats only (Fig. 2s).
Histology and immunohistochemistry of retina specimens from SDT rats. a Haematoxylin–eosin staining of posterior retina from a normoglycaemic SDT rat (SDT-control) showing no abnormalities (×200). b Haematoxylin–eosin staining of posterior retina from a hyperglycaemic SDT rat (SDT-NDR) showing no abnormalities (×200). c Haematoxylin–eosin staining of posterior retina from a hyperglycaemic SDT rat with massive vascular proliferation (SDT-PR), showing a membrane starting from the head of the optic disc pulling the retina inward to the vitreous cavity on the right-hand side of the section. The formation of several retinal folds can be seen in this section (×50). d Haematoxylin–eosin staining of peripheral retina from an SDT-PR rat showing no abnormalities (×200). e Azan staining of posterior retina from an SDT-control rat showing no abnormalities (×200). f Azan staining of posterior retina from an SDT-NRS rat (×200). No abnormality was seen in the neurosensory retina, although positive staining was observed in the membrane beneath the retinal surface. g Azan staining of posterior retina from an SDT-PR rat (×50). There is a prominent plexus of matrix-rich membrane, starting from the head of the optic nerve and connecting to the posterior lens and retracted peripheral retina. h A high-magnification photograph of azan staining of posterior retina from an SDT-PR rat, showing the head of the optic nerve and matrix membrane containing some cellular components (×400). i Anti-Griffonia simplicifolia isolectin B4 (GSA) staining of posterior retina from an SDT-control rat (×200). j Anti-GSA staining of posterior retina from an SDT-NRS rat showing no abnormalities in vascular structure (×200). k Anti-GSA staining of posterior retina from an SDT-PR rat (×100). The membrane contains GSA-positive nuclei. No abnormality in vascular structure of the neurosensory retina is present. l Anti-vascular endothelial growth factor (VEGF) staining of posterior retina from an SDT-control rat, showing weak immunoreactivity in the neurosensory retina (×200). m Anti-VEGF staining of posterior retina from an SDT-NRS rat (×200). VEGF immunoreactivity is increased in the ganglion cell layer, the inner nuclear layer and the border of the outer nuclear layer and the photoreceptor outer segment. n Anti-VEGF staining of posterior retina from an SDT-PR rat (×50). The arrows show localisation of VEGF-positive areas in the neurosensory retina. o Anti-VEGF staining of posterior retina from an SDT-PR rat, showing increased VEGF immunoreactivity in the ganglion cell layer, the inner nuclear layer and the border of the outer nuclear layer and the photoreceptor outer segment (×200). p Anti-VEGF staining of posterior retina from an SDT-control rat (×400). q Anti-VEGF staining of posterior retina from an SDT-NRS rat (×400). r Anti-VEGF staining of posterior retina from an SDT-PR rat (×50). The arrows show hyper-immunoreactivity of VEGF, presumably in vascular endothelial cells. s Anti-VEGF staining of posterior retina from an SDT-PR rat (×1,000). There are several VEGF-positive cells in the vascular walls of large retinal vessels that appear to be vascular endothelial cells
Discussion
Male SDT rats exhibit spontaneous glucose intolerance with impaired insulin secretion at 14 weeks of age, and by 20 weeks of age, they develop diabetes with marked hyperglycaemia and hypoinsulinaemia accompanied by decreased body weight and body mass index [11, 13]. The SDT rat is thought to be a non-obese animal model of human type 2 diabetes, as it develops tissue damage in pancreatic islets equivalent to the dysfunction of pancreatic islet tissue that plays a major role in the development of human diabetes. As the SDT rat can survive for a long time without insulin treatment, it is considered a useful model of type 2 human diabetes mellitus. The main difference between the SDT rat model and other rodent models of diabetes is that these rats develop severe ocular complications such as neovascularisation and tractional changes in the retina. There is no rodent model of severe diabetic retinopathy, and the SDT rat may be a very good candidate.
However, in contrast to humans with diabetic retinopathy, the SDT rat does not develop vascular non-perfusion, bleeding, hard exudates or soft exudates in the retina. In this study, only 53% of the rats were found to have proliferative retinal changes. These proliferative changes were caused by retinal neovascularisation originating in the optic disc. Azan staining showed that the tractional changes may have been due to alterations in vitreo-retinal interaction, very similar to the changes that occur in human proliferative diabetic retinopathy.
It is already very clear that VEGF plays a key role in the development of diabetic ocular complications in human eyes, such as ocular neovascularisation and blood ocular barrier breakdown [14–18]. Increased levels of VEGF have also been detected in the eyes of diabetic animals [19–21]. In our immunohistochemical study we also showed increased immunoreactivity of VEGF in the SDT-NRS and SDT-PR rats, with the difference between these two groups being the intensity of immunoreactivity and location of staining in the vascular endothelial cells. Previous reports on the retina of STZ rats have shown high expression of VEGF mRNA in the ganglion cell layer, the inner nuclear layer and the outer nuclear layer, whereas no VEGF expression was found in normal control rats [19, 21]. The STZ rats were reported to have no ischaemic changes in the retina; however, VEGF expression was higher than in normoglycaemic controls, similar to our finding in SDT rats. Intense staining of VEGF antibody to vascular endothelial cells has also been observed in human proliferative diabetic retinopathy [17, 22]. These studies found intense immunoreactivity for VEGF in the fibrovascular membrane, the vascular endothelial cells, the ganglion cell layer and the inner nuclear layer. The VEGF immunohistochemistry results of our study appear to be similar to those reported in human diabetic retinopathy.
In a mouse model of hypoxia-induced retinal neovascularisation it has been shown that upregulation of VEGF mRNA secondary to large areas of vascular non-perfusion results in massive retinal neovascularisation [23]. In contrast to this model of hypoxia-induced retinopathy, neither SDT nor STZ rats develop areas of vascular non-perfusion. Accordingly, we hypothesise that there are mechanisms other than hypoxia that stimulate the retina to produce VEGF.
Why, then, do SDT rats develop retinal neovascularisation without ischaemic change? One possible reason is the change in the vitreo-retinal interface. In diabetic traction retinal detachment in the human eye, the posterior hyaloid membrane plays a major role in the development of ocular proliferation [24]. It has also been shown in human diabetic retinopathy that the site where vitreous adhesion persists is very likely to be the base for vascular proliferation [25]. In SDT rats, azan staining revealed some adherence, presumably of vitreous cortex, to the retina in SDT-NRS and SDT-PR rats, but not in SDT-control rats. This finding indicates that hyperglycaemia, high levels of VEGF expression, or other factors specific to the SDT diabetic rat caused thickening of the posterior vitreous cortex or modified vitreo-retinal interactions [25, 26].
The other possible reason why diabetic rat models such as the STZ rat reportedly never develop pre-retinal neovascularisation [10] is that diabetic rodents tend not to live long enough to develop severe stages of diabetic retinopathy. However, while the STZ rat is not able to survive without insulin treatment, the SDT rat is able to live for long periods without medical support. This allows the retinal vasculature to be exposed to high levels of VEGF for a longer period.
As described above, there appear to be differences between the SDT rat model of diabetic retinopathy and human proliferative diabetic retinopathy, as the SDT rat develops retinal neovascularisation without prominent retinal ischaemia. However, the SDT rat is a very unique model for ocular neovascularisation caused by increased expression of VEGF secondary to hyperglycaemia. Therefore, we consider the SDT rat a useful model for the further study of ocular neovascularisation and the interaction between VEGF and vascular endothelial cells.
Abbreviations
- GSA:
-
Griffonia simplicifolia isolectin B4 antibody
- SDT:
-
spontaneously diabetic Torii
- SDT-control:
-
control SDT rat with normoglycaemia
- SDT-NRS:
-
SDT rat with normal retinal structure
- SDT-PR:
-
SDT rat with proliferative retinopathy
- STZ:
-
streptozotocin
- VEGF:
-
vascular endothelial growth factor
References
Kern T, Kowlulu R, Engerman R (1994) Questions raised by studies of experimental diabetic retinopathy. Elsevier Science, Japan
Kador PF, Takahashi Y, Wyman M, Ferris F III (1995) Diabetes-like proliferative retinal changes in galactose-fed dogs. Arch Ophthalmol 113:352–354
Buechi E, Kurosawa A, Tso M (1996) Retinopathy in diabetic hypertensive monkeys: a pathologic study. Graefes Arch Clin Exp Ophthalmol 234:388–398
Sima AA, Chakrabarti S, Garcia-Salinas R, Basu PK (1985) The BB-rat – an authentic model of human diabetic retinopathy. Curr Eye Res 4:1087–1092
Mansford KR, Opie L (1968) Comparison of metabolic abnormalities in diabetes mellitus induced by streptozotocin or by alloxan. Lancet 1:670–671
Hanafusa T, Maiyagawa J, Nakajima H et al (1994) The NOD mouse. Diabetes Res Clin Prac 24[Suppl]:S307–S311
Peterson R, Shaw M, Neel M-A, Eichberg J (1990) Zucker diabetic fatty rat as model for non-insulin-dependent diabetes melllitus. ILAR News 32:16–19
Berdanier CD (1991) The BHE rat: an animal model for the study of non-insulin-dependent diabetes mellitus. FASEB J 5:2139–2144
Kuwano K, Hirashima T, Mori S, Saitoh Y, Kurosumi T, Natori T (1992) Spontaneous long-term hyperglycemic rat with diabetic complications: Otsuka–Long–Evans–Tokushima Fatty (OLETF) strain. Diabetes 41:1248–1422
Engerman R, Finkelstein D, Aguirre G et al (1982) Ocular complications. Diabetes 31[Suppl 1]:82–88
Shinohara M, Masuyama T, Shoda T et al (2000) A new spontaneously diabetic non-obese Torii rat strain with severe ocular complications. Int J Exp Diabetes Res 1:89–100
Smith L, Woesolowski E, McLellan A et al (1994) Oxygen-induced retinopathy in the mouse. Invest Ophthalmol Vis Sci 35:101–111
Masuyama T, Komeda K, Hara A et al (2003) Chronological characterization of diabetes development in male spontaneously diabetic Torii rats. Biochem Biophys Res Commun 314:870–877
Aiello L, Avery R, Arig P et al (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487
Adamis A, Miller J, Bernal M-T et al (1994) Increased vascular endothelial growth factor levels in the vitreous of eyes with proliferative diabetic retinopathy. Am J Ophthalmol 118:445–450
Gerhardinger C, Brown LF, Roy S, Mizutani M, Zucker CL, Lorenzi M (1998) Expression of vascular endothelial growth factor in the human retina and in nonproliferative diabetic retinopathy. Am J Pathol 152:1453–1462
Pe’er J, Folberg R, Itin A, Gnessin H, Hemo I, Keshet E (1996) Upregulated expression of vascular endothelial growth factor in proliferative diabetic retinopathy. Br J Ophthalmol 80:241–245
Amin RH, Frank RN, Kennedy A, Eliott D, Puklin JE, Abrams GW (1997) Vascular endothelial growth factor is present in glial cells of the retina and optic nerve of human subjects with nonproliferative diabetic retinopathy. Invest Ophthalmol Vis Sci 38:36–47
Murata T, Nakagawa K, Khalil A, Ishibashi T, Inomata H, Sueishi K (1996) The relation between expression of vascular endothelial growth factor and breakdown of the blood-retinal barrier in diabetic rat retinas. Lab Invest 74:819–825
Sone H, Kawakami Y, Okuda Y et al (1997) Ocular vascular endothelial growth factor levels in diabetic rats are elevated before observable retinal proliferative changes. Diabetologia 40:726–730
Hammes HP, Lin J, Bretzel RG, Brownlee M, Breier G (1998) Upregulation of the vascular endothelial growth factor/vascular endothelial growth factor receptor system in experimental background diabetic retinopathy of rat. Diabetes 47:401–406
Boulton M, Foreman D, Williams G, McLeod D (1998) VEGF localisation in diabetic retinopathy. Br J Ophthalmol 82:561–568
Pierce E, Avery R, Foley E, Aiello L, Smith L (1995) Vascular endothelial growth factor/vascular permeability factor expression in a mouse model of retinal neovascularization. Proc Natl Acad Sci U S A 92:905–909
Rand LI, Prud’homme GJ, Ederer F, Canner PL, Group tDRS (1985) Factors influencing the development of visual loss in advanced diabetic retinopathy. Invest Ophthalmol Vis Sci 26:983–991
Kishi S, Shimizu K (1993) Clinical manifestations of posterior precortical vitreous pocket in proliferative diabetic retinopathy. Ophthalmology 100:225–229
Frank RN (2004) Diabetic retinopathy. N Engl J Med 350:48–58
Acknowledgements
The SDT rats were kindly provided by the SDT rat study group (Torii Pharmaceutical Company, Tokyo, Japan).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamada, H., Yamada, E., Higuchi, A. et al. Retinal neovascularisation without ischaemia in the spontaneously diabetic Torii rat. Diabetologia 48, 1663–1668 (2005). https://doi.org/10.1007/s00125-005-1809-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1809-0