Abstract
Purpose
In this systematic literature review, the effects of the application of a checklist during in hospital resuscitation of trauma patients on adherence to the ATLS guidelines, trauma team performance, and patient-related outcomes were integrated.
Methods
A systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-analyses checklist. The search was performed in Pubmed, Embase, CINAHL, and Cochrane inception till January 2019. Randomized controlled- or controlled before-and-after study design were included. All other forms of observational study designs, reviews, case series or case reports, animal studies, and simulation studies were excluded. The Effective Public Health Practice Project Quality Assessment Tool was applied to assess the methodological quality of the included studies.
Results
Three of the 625 identified articles were included, which all used a before-and-after study design. Two studies showed that Advanced Trauma Life Support (ATLS)-related tasks are significantly more frequently performed when a checklist was applied during resuscitation. [14 of 30 tasks (p < 0.05), respectively, 18 of 19 tasks (p < 0.05)]. One study showed that time to task completion (− 9 s, 95% CI = − 13.8 to − 4.8 s) and workflow improved, which was analyzed as model fitness (0.90 vs 0.96; p < 0.001); conformance frequency (26.1% vs 77.6%; p < 0.001); and frequency of unique workflow traces (31.7% vs 19.1%; p = 0.005). One study showed that the incidence of pneumonia was higher in the group where a checklist was applied [adjusted odds ratio (aOR) 1.69, 95% Confidence Interval (CI 1.03–2.80)]. No difference was found for nine other assessed complications or missed injuries. Reduced mortality rates were found in the most severely injured patient group (Injury Severity score > 25, aOR 0.51, 95% CI 0.30–0.89).
Conclusions
The application of a checklist may improve ATLS adherence and workflow during trauma resuscitation. Current literature is insufficient to truly define the effect of the application of a checklist during trauma resuscitation on patient-related outcomes, although one study showed promising results as an improved chance of survival for the most severely injured patients was found.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Background
A specialized trauma team should resuscitate severely injured trauma patients. The goal was to identify and treat life-threatening injuries at an early stage. Previous studies have shown that severely injured patients resuscitated by a trauma team have a higher chance of survival compared to trauma patients resuscitated without a trauma team [1,2,3,4]. Specialized trauma teams are composed of a variable number of medical specialists and paramedical workers and typically consist of a trauma surgeon or an emergency physician, an anesthetist, a radiologist, in some cases a neurologist, emergency nurses, and a diagnostic radiographer. To reduce the time from injury to critical interventions, a predefined set of consecutive tasks is performed by the trauma team members [5].
In most cases, available information about the health status of severely injured patients during resuscitation is limited, while there are potentially many different injuries that could be life-threatening. To adequately identify and treat potentially life-threatening injuries, a full-scale and structured assessment is required. The Advanced Trauma Life Support™ (ATLS™) guidelines are accepted worldwide and are the structural standard for the systematic resuscitation of trauma patients [6]. The ATLS™ guidelines provide guidance to the trauma team during trauma resuscitation by prioritizing diagnostic and treatment procedures.
Previous studies reported that tasks recommended by the ATLS™ guidelines are not always performed during trauma resuscitation, whereas adherence to ATLS™ guidelines varied between 42 and 82% [7,8,9,10,11]. Although procedures within the ATLS™ guidelines are constructed in a chronological and coherent manner, human factors may challenge the natural limitations of our memory [12, 13]. A previous study at our institute illustrates that 35 tasks should be performed during the first 7 min, as recommended by the ATLS™ [14]. Since there are many tasks to fulfill in limited time, tasks could easily be overlooked. Thereby, common situations during trauma resuscitation such as stressful circumstances, sudden interruptions and lack of experience of trauma team members affect the capacity of memory and, therefore, may contribute to suboptimal adherence of ATLS™ guidelines [15,16,17,18].
A checklist could complement the naturally limited human memory, which could be even more impaired by the stress felt during initial resuscitation. In general, a checklist could be used as a reminder, in order to completely and adequately fulfill a single complex procedure or a sequence of procedures. For example, safety checklists have been shown to improve medical care and have been used in medicine for several years. Thomassen et al. [19] performed a systematic review in 2014 and summarized medical literature to show the effects of safety checklist. Thirty-four studies were included, of which some had investigated well known-safety checklists such as the SURgical PAtient Safety System (SURPASS) or the World Health Organization (WHO) surgical safety checklist. The auteurs concluded that the use of safety checklist had reduced mortality and morbidity in targeted patients groups [19]. In addition, safety checklists have strengthened compliance with guidelines, improved human factors, and reduced the incidence of adverse events [19]. Comparable positive effects were found by a more recent studies, of Ramsay et al. [20] who investigated the introduction of the SURPASS in Scotland and of de Jager et al. [21] who performed a single center observational study, investigating the effect of the introduction of the surgical safety checklist with a follow-up time of 5 years.
The capability of checklists to complement human memory may also improve trauma resuscitation. Therefore, we aimed to systematically review the literature to determine the effects of the application of a checklist during trauma resuscitation of a trauma patient by a trauma team on adherence to the ATLS™ guidelines, trauma team performance, and patient-related outcomes.
Methods
The systematic review adhered to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) [22].
Search strategy
A systematic search of studies listed in the electronic databases of Pubmed, Embase, CINAHL, and Cochrane was performed from their inception till January 2019. We combined the search terms derived from our research aim in separate search strings for each database (Table 1). Our search terms covered the intended population (Trauma resuscitation, including accessory search terms) and intervention (the application of a checklist, including accessory search terms). By purpose, we did not use search terms for outcomes, in order to avoid the introduction selection bias, as we intended to research all possible outcomes. In addition, all reference lists of included articles were screened for relevant additional citations.
Eligibility criteria
Studies were included if the effect of the application of a checklist during resuscitation of trauma patients by a trauma team in an in-hospital setting was evaluated. We included studies with a randomized controlled—or controlled before-and-after study design. All other forms of observational study designs, reviews, case series or case reports, animal studies, and simulation studies were excluded. Solely English and Dutch publications from peer-review journals were reviewed. There were no restrictions on the year of publication, on the age of patients or on composition or method of application of a checklist during trauma resuscitation.
Study selection
First, all eligible studies were selected by screening the title and abstract. Second, all selected papers were screened full-text. During these two phases, two investigators independently selected articles according to the predefined eligibility criteria and discussed their results. In case of any unresolved disagreements, a third reviewer made the final decision using the same eligibility criteria. The resultant articles after the two phases of screening were included in our systematic review.
Data collection and critical appraisal
Two reviewers independently extracted and inserted the following data into tables: Authors, year of publication, study design, research population, checklist’s items, composition, form, and application during trauma resuscitation and all identified effects reported by the included articles. To assess the methodological quality of the included studies, the Effective Public Health Practice Project Quality Assessment Tool (EPHPP tool) was applied [23]. This tool has been judged suitable to be used in systematic reviews of effectiveness [24] and has been reported to have content and construct validity [25, 26]. Furthermore, this tool is a reliable instrument to assess the quality of randomized controlled trials and before-and-after studies, whereas the overall inter-observer coefficient was found to be 0.77 (95% CI 0.51–0.90) [27]. This inter-observer coefficient value is considered as an excellent agreement [28] (Table 2).
Results
Selection
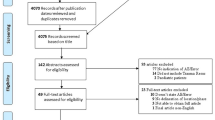
The search strategy yielded 625 potentially relevant titles and abstract. After screening title and abstract, 20 articles remained for full-text screening (Fig. 1). After screening the full texts of remaining articles, three studies were included in our systematic review. No additional studies were found by assessing the reference lists of included studies.
Study characteristics
All three included studies had a before-and-after study design to investigate the effect of the application of a checklist during trauma resuscitation. Two included studies of Kelleher et al. [29, 30] originated from the same pediatric trauma center and had the same sample. Two separate analyses and corresponding results were published in two different articles [30]. In their studies all trauma resuscitations had been captured on video during two 4-month periods and were analyzed retrospectively. They included 435 and 437 cases in their analyses, respectively. The third included study, of Lashoher et al. [31], was a multicenter study, including 11 hospitals in eight different countries. A random sample of 20% of all trauma resuscitations was assessed by live observants. Data collection duration varied among the different hospitals and ranged from 3 to 8 months pre- and 3–11 months post-implementation. In total, 3422 resuscitations had been assessed and the results were analyzed.
Critical appraisal
Using the EPHPP quality assessment tool, the quality of the two studies of Kelleher et al. [29, 30] and Lashoher et al. [31] were found to be moderate and weak, respectively (Table 3). Most concerning point that affected the quality of all three studies was the awareness of the participants (trauma team members) of being studied. This effect, also known as the Hawthorne effect [32], could have influenced behavior during trauma resuscitations. Two other points of concern were found in the study of Lashoher et al. [31], whereas no description of the randomization, withdrawal, and dropout of trauma resuscitations was provided.
The checklists
Two different checklists were applied in the three included studies. A paper checklist was used in the two studies of Kelleher et al. [28, 29]. The checklist was applied by the surgical team leader (surgical senior resident, fellow, or attending) or a member of the emergency medicine leadership team (emergency medicine fellow or attending) during trauma resuscitation. The checklist was composed of 30 items extracted from the ATLS™ guidelines, of which 14 items belong to the primary survey and 16 items belong to the secondary survey. The checklist was designed to track task completion by the bedside clinician (surgical junior resident or trauma nurse practitioner) and other team members.
In the study of Lashoher et al. [31], the application of the World Health Organization Trauma Care Checklist was investigated. The WHO trauma care Checklist is based on a literature review of medical errors during initial resuscitation of severely injured patients [33], and contains 19 core items, of which 11 items are tasks also described in the ATLS™ guidelines. Hospital staff of all 11 hospitals participating in the study received checklist- and patient safety training. Furthermore, hospital staff of each participating hopsital were encouraged to modify the checklist to be relevant in their unique setting. The study team of the core checklist approved site-specific final versions. The responsible member of the trauma team and form (e.g. paper or electronic) of the checklist during resuscitation was not described in the included article.
Effects measured
Six different outcomes-related to the applications of a checklist during trauma resuscitation were identified: Mortality, complications, missed injuries, task adherence, mean time to task completion, and workflow.
Mortality
Lashoher et al. [31] found no difference in odds of mortality in the overall study sample after adjusting for patient demographics and injury severity. After an injury-severity-stratified analysis, checklist implementation was associated with a 50% reduction (adjusted odds ratio (aOR) 0.51, 95% Confidence Interval (CI 0.30–0.89) in mortality among patients with the most severe injuries (Injury severity score > 25). No such association was found among patients who were less severely injured (injury severity score < 25) [31].
Complications
Only the incidence of one of the ten complications, pneumonia, was slightly higher after the introduction of the checklist after adjusting for patient characteristics (aOR 1.69, 95% CI 1.03–2.80) in the study of Lashoher et al. [31]. No differences were found for the other nine assessed complications [31].
Missed injuries
The incidence of missed injuries was zero in both groups and did not differ before and after implementation of a checklist after adjusting for patient characteristics and injury severity (aOR 0.62; 95% CI 0.19–2.03; p = 0.437) in the study of Lashoher et al. [31].
Task adherence
Fourteen of the thirty ATLS-related tasks that had been assessed in the study of Kelleher et al. [29] were completed significantly more frequently after checklist introduction (for all p ≤ 0.05). None of the 30 ATLS-related were performed less frequently. After adjustment for type of resuscitation factors and type of tasks (tasks were not further specified), the odds of completing primary survey tasks were 2.66 (95% CI 2.07–3.42) times higher after implementation, and the adjusted odds of secondary survey task completion were 2.46 (95% CI 2.04–2.98) times higher. Lashohor et al. [31] found 18 of the 19 clinical tasks to be significantly (p < 0.05) more frequently performed after implementation of the WHO trauma care checklist.
Mean time to task completion
Kelleher et al. [30] found that the average adjusted time to task completion was 9 s faster with the application of a checklist (95% CI − 13.8 to − 4.8 s) Furthermore, six of the 12 primary survey tasks (full exposure, temperature measurement, blood pressure, heart rate measurement, respiratory rate measurement, and oxygen saturation) were performed significantly (all p < 0.05) faster (− 20 till − 43 s) [29].
Workflow
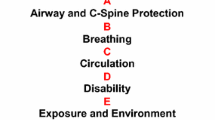
A predefined ideal process model of six ATLS primary survey tasks was created in the study of Kelleher et al. [30] The six ATLS tasks were categorized into Airway (A), Breathing (B), Circulation (C), and Disability (D) which is well known from the ABCDE mnemonic as described in the ATLS Guidelines. The model required that “A” tasks are done before “B” tasks, “B” tasks are done before “C” tasks, and “C” tasks are done before “D” task. Model fitness (degree of agreement with the ideal process model, ranging from 0 to 1), conformance (“yes” if fitness 1; “no” if fitness < 1) was measured and the frequency of unique workflow traces were analyzed. Besides the comparison of the application of a checklist, analysis of a brief pre-arrival notification was performed. The authors found that after implementation of a checklist workflow improved. Model fitness (0.80 vs 0.91; p = 0.007), conformance frequency (26.1% vs 59.4%; p = 0.01), and number of unique workflow traces (19 vs 16; p = 0.01) improved for resuscitations without notification. Comparable improvement was shown after the implementation of the checklist when a brief notification was given, in which case Model fitness (0.90 vs 0.96; p < 0.001), conformance frequency (50.8% vs 77.6%; p < 0.001), and frequency of unique workflow traces (63 vs 35; p = 0.005) also improved. Finally, the effect of the absence of pre-arrival notification on model fitness was also smaller after checklist implementation compared to before the use of the checklist (Cohen’s d = 0.75 (95% CI 0.73–0.82) vs. Cohen’s d = 0.52 (95% CI 0.51–0.56).
Discussion
Our systematic review shows that the application of a checklist may improve adherence to ATLS guidelines and workflow during resuscitation. Furthermore, we found that the application of a checklist might lead to a reduction of mortality among severely injured patients. However, there was no effect found on missed injuries and the incidence of one out of ten complications investigated was even slightly higher when a checklist was applied during resuscitation.
Several limitations in our systematic review and included studies should be considered. First, only three studies could be included and besides adherence to task performance, all effects including patient-related outcomes were investigated only in one study per effect. Therefore, no meta-analysis or other forms of analysis were performed on the collected data.
Second, the quality of the only study investigated patient-related outcome was weak [31]. The limitations in this study may have affected the effect of a checklist on patient-related outcomes. For example, the increased incidence of pneumonia in patients resuscitated with the application of a checklist is unexpected. The authors clarified that there may be systematic errors or misclassifications in both process and outcome measures, such as different available imaging modalities across centers for the diagnosis of complications such as pneumonia. Furthermore, the incidence of missed injuries was zero in both groups. Previous studies, however, show that missed injuries vary between 1.3 and 39% [34]. These low numbers may, therefore, be a result of information bias, which was caused by suboptimal registration of missed injuries. Furthermore, the study of Lashoher et al. [31] did not only measure the effect of a checklist on trauma resuscitation. Hospital staff received checklist- and patient safety training in the context of trauma care and, therefore, the impact of checklist implementation was also studied.
Third, the populations of two of the three studies were pediatric trauma patients. Although ATLS principles are used for resuscitation of injured children and adult patients, interpretation of cardiorespiratory variables, airway anatomy, response to blood loss, thermoregulation, and the trauma team composition are different in pediatric resuscitation and may have influenced ATLS adherence rates and workflow [35, 36].
Finally, different checklists were applied in the included studies. We did not predefine the type and application style of the checklist for trauma resuscitation since we did not find any evidence in literature on optimal composition and application of checklists during trauma resuscitation. The composition of the checklists was different in the included studies, whereas 30 items were included in the checklist applied in the Kelleher studies and in the study of Lashoher et al. [31] 14 tasks with variation per hospital were formed based on a literature search.
Although this systematic review and included articles have several limitations, the application of a checklist during trauma resuscitation may improve patient- and process- related outcomes. The improvement of ATLS adherence is in line with the results of studies investigating the application of checklists in other fields of medicine, whereas adherence to guidelines for surgical safety procedures and adherence to protocols improved [20, 37,38,39,40,41,42].
Additional research is needed for a more reliable estimation of the effect of the application of a checklist during trauma resuscitation on patient’s- and process-related outcomes. Future studies investigating the effect of the application of a checklist should use a before-and-after study design, whereas in a randomized controlled design introduces recall bias as the members of the trauma team not using the checklist are likely to remember details about the checklist. To minimize bias by observers, the same observer(s) should assess the trauma resuscitations. Analysing videos of recorded trauma resuscitations could obviate the need for multiple observers to observe all resuscitations, especially during the night and weekend, or when there are multiple trauma resuscitations at the same time. Furthermore, missed injuries should be actively searched, for example, by a 30-day follow-up with a clinical re-evaluation of included patients and a retrospective re-evaluation of performed diagnostic imaging. Finally, to our knowledge, no research has been performed to investigate optimal checklist composition and application for trauma resuscitation. Improvement of composition and application may improve the user-friendliness of a checklist and may potentially improve the trauma resuscitation process even further.
Although the evidence is marginal, the application of a checklist during trauma resuscitation seems to improve processes during trauma resuscitation and may even improve the chance to survive for the most severely injured patients. Thereby, no adverse events were noticed at the three included studies. On the other hand, the implementation of a checklist may be paired with several barriers. In the study of Nolan et al. [43] barriers to implementing the World Health Organization’s Trauma Care Checklist are described, including unclear roles, lack of enforcement, poor understanding of the purpose and professional hierarchy. These barriers were comparable to barriers that have been described by previous studies investigating the implementing of the WHO’s Surgical Safety Checklist [44,45,46,47], which have shown to reduce mortality and morbidity [20, 48].
In conclusion, considering the results of our systematic review including limitations and included studies, the application of a checklist could be useful and may be considered to be introduced into daily practice. Further research is needed for a more reliable estimation of the effect of the application of a checklist during trauma resuscitation on patient- and process-related outcomes.
References
Petrie D, Lane P, Stewart TC. An evaluation of patient outcomes comparing trauma team activated versus trauma team not activated using TRISS analysis. Trauma and injury severity score. J Trauma Acute Care Surg. 1996;41:870–3 (Discussion 873–875).
Cornwell EE, Chang DC, Phillips J, Campbell KA. Enhanced trauma program commitment at a level I trauma center: effect on the process and outcome of care. Arch Surg. 2003;138:838–43.
Gerardo CJ, Glickman SW, Vaslef SN, Chandra A, Pietrobon R, Cairns CB. The rapid impact on mortality rates of a dedicated care team including trauma and emergency physicians at an academic medical center. J Emerg Med. 2011;40:586–91.
Rainer TH, Cheung NK, Yeung JH, Graham CA. Do trauma teams make a difference? A single centre registry study. Resuscitation. 2007;73(3):374–81.
Tiel Groenestege-Kreb D, van Maarseveen O, Leenen L. Trauma team. Br J Anaesth. 2014;113(2):258–65.
Henry S. ATLS 10th edition offers new insights into mana ging trauma patients // Bulletin of the American College of Surgeons [Internet] [published 01 Jun; 2018; cited 9 Jul; 2019]. Available from: http://bulletin.facs.org/2018/06/atls-10th-edition-offers-new-insights-into-managing-traumapatients/
Spanjersberg WR, Bergs EA, Mushkudiani N, Klimek M, Schipper IB. Protocol compliance and time management in blunt trauma resuscitation. Emerg Med J. 2009;26(1):23–7.
Santora T, Trooskin S, Blank C. Video assessment of trauma response: adherence to ATLS protocols. Am J Emerg Med. 1996;14(6):564–9.
McCrum ML, McKee J, Lai M, Staples J, Switzer N, Widder SL. ATLS adherence in the transfer of rural trauma patients to a level i facility. Injury. 2013;44:1241–5.
Spanjersberg WR, Bergs EA, Mushkudiani N, Klimek M, Schipper IB. Protocol compliance and time management in blunt trauma resuscitation. Emerg Med J. 2009;26(1):23–7.
Tsang B, McKee J, Engels PT, Paton-Gay D, Widder SL. Compliance to advanced trauma life support protocols in adult trauma patients in the acute setting. World J Emerg Surg. 2013;8(1):39.
Cowan N. The magical mystery four: how is working memory capacity limited, and why? Curr Dir Psychol Sci. 2010;19(1):51–7.
Cowan N. Working memory capacity. New York: Psychology press; 2012.
Lubbert PH, Kaasschieter EG, Hoorntje LE, Leenen LP. Video registration of trauma team performance in the emergency department: the results of a 2-year analysis in a Level 1 trauma center. J Trauma. 2009;67(6):1412–20.
Harvey A, Bandiera G, Nathens AB, LeBlanc VR. Impact of stress on resident performance in simulated trauma scenarios. J Trauma Acute Care Surg. 2012;72(2):497–503.
Xiao Y, Mackenzie CF. Stress and decision-making in trauma patient resuscitation. Baltimore: University of Maryland; 1997.
Tornero-Aguilera JF, Clemente-Suárez VJ. Effect of experience, equipment and fire actions in psychophysiological response and memory of refsoldiers in actual underground operations. Int J Psychophysiol. 2018;128:40–6.
Gabrys RL, Howell JW, Cebulski SF, Anisman H, Matheson K. Acute stressor effects on cognitive flexibility: mediating role of stressor appraisals and cortisol. Stress. 2019;22(2):182–9.
Ramsay G, et al. Reducing surgical mortality in Scotland by use of the WHO surgical safety checklist. Br J Surg. 2019;106:1005–11.
Thomassen Ø, Espeland A, Søfteland E, Lossius H, Heltne J, Brattebø G. Implementation of checklists in health care; learning from high-reliability organisations. Scand J Trauma Resusc Emerg Med. 2011;19:53.
de Jager E, Gunnarsson R, Ho YH. Implementation of the world health organization surgical safety checklist correlates with reduced surgical mortality and length of hospital admission in a high-income country. World J Surg. 2019;43:117–24.
Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Reprinted from Annals of Internal Medicine). Phys Ther. 2009;89(9):873–80.
Effective Public Health Practice Project. (1998). Quality assessment tool for quantitative studies. Hamilton, ON: Effective public health practice project. Available at: http://www.ephpp.ca/index.html. Accessed 7 Mar 2018.
Deeks JJ, et al. Evaluating non-randomised intervention studies. Health Technol Assess (Winch Engl). 2003;7(27):1–73.
Jackson N, Waters E. Criteria for the systematic review of health promotion and public health interventions. Health Promot Int. 2005;20(4):367–74.
Thomas BH, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs. 2004;1(3):176–84.
Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. J Eval Clin Pract. 2012;18(1):12–8.
McDowell I. The theoretical and technical foundations of health measurement. In: Measuring Health: A Guide to Rating Scales and Questionnaires. New York: Oxford University Press; 2006; pp 10–46.
Kelleher DC, Carter EA, Waterhouse LJ, Parsons SE, Fritzeen JL, Burd RS. Effect of a checklist on advanced trauma life support task performance during pediatric trauma resuscitation. Acad Emerg Med. 2014;21(10):1129–34.
Kelleher DC, Jagadeesh Chandra Bose RP, Waterhouse LJ, Carter EA, Burd RS. Effect of a checklist on advanced trauma life support workflow deviations during trauma resuscitations without pre-arrival notification. J Am Coll Surg. 2014;218:459–66.
Lashoher A, et al. Implementation of the World Health Organization Trauma Care Checklist program in 11 centers across multiple economic strata: effect on care process measures. World J Surg. 2017;41:954–62.
Franke RH, Kaul JD. The Hawthorne experiments: first statistical interpretation. Am Sociol Rev. 1978;43(5):623–43.
WHO Trauma Care Checklist. Available at: http://www.who.int/emergencycare/publications/trauma-care-checklist.pdf?ua=1 Accessed Oct 22, 2017.
Pfeifer R, Pape H-C. Missed injuries in trauma patients: a literature review. Patient Saf Surg. 2008;2:20.
Stallion A. Initial assessment and management of pediatric trauma patient. Respir Care Clin N Am. 2001;7(1):1–11.
McFadyen JG, Ramaiah R, Bhananker SM. Initial assessment and management of pediatric trauma patients. Int J Crit Illn Inj Sci. 2012;2(3):121–7.
Makary MA, et al. Operating room briefings and wrong-site surgery. J Am Coll Surg. 2007;204(2):236–43.
Verdaasdonk EGG, Stassen LPS, Hoffmann WF, Van Der Elst M, Dankelman J. Can a structured checklist prevent problems with laparoscopic equipment? Surg Endosc Other Interv Tech. 2008;22(10):2238–43.
Byrnes MC, et al. Implementation of a mandatory checklist of protocols and objectives improves compliance with a wide range of evidence-based intensive care unit practices. Crit Care Med. 2009;37(10):2775–81.
Hall AJ, Toner NS, Bhatt PM. The introduction of a neurosurgical postoperative checklist improved quality of care and patient safety. Br J Neurosurg. 2019. https://doi.org/10.1080/02688697.2019.1606894.
Molina RL, et al. Delivery practices and care experience during implementation of an adapted safe childbirth checklist and respectful care program in Chiapas, Mexico. Int J Gynecol Obstet. 2019;145(1):101–9.
Khajuria A, et al. Implementation of a checklist to enhance operation note quality at a UK burns centre. Burns. 2018;45:835–40.
Nolan B, Zakirova R, Bridge J, Nathens AB. Barriers to implementing the world health organization’s trauma care checklist: a canadian single-center experience. J Trauma Acute Care Surg. 2014;77(5):679–83.
Bosk CL, Dixon-Woods M, Goeschel CA, Pronovost PJ. Reality check for checklists. Lancet. 2009;374(9688):444–5.
Vats A, Vincent CA, Nagpal K, Davies RW, Darzi A, Moorthy K. Practical challenges of introducing WHO surgical checklist: UK pilot experience. BMJ. 2010;340:b5433.
Fourcade A, Blache J-L, Grenier C, Bourgain J-L, Minvielle E. Barriers to staff adoption of a surgical safety checklist. BMJ Qual Saf. 2012;21(3):191–7.
Levy SM, et al. Implementing a surgical checklist: more than checking a box. Surg (US). 2012;152(3):331–6.
Haynes A, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–9.
Acknowledgements
The authors would like to thank Cassandra Nemzoff and Toon van der Gronde for their English manuscript correction services.
Author information
Authors and Affiliations
Contributions
OEC defined the search strategy and eligibility criteria, supervised study selection, interpreted data, wrote the major part of the manuscript, acts as corresponding author, and checked the references. WHW Supervised development of work, wrote parts of the manuscript, helped in data interpretation, and manuscript evaluation. NLM and TFF performed study selection, wrote parts of the manuscript and checked the references. LPH Supervised development of work, helped in data interpretation and manuscript evaluation
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
van Maarseveen, O.E.C., Ham, W.H.W., van de Ven, N.L.M. et al. Effects of the application of a checklist during trauma resuscitations on ATLS adherence, team performance, and patient-related outcomes: a systematic review. Eur J Trauma Emerg Surg 46, 65–72 (2020). https://doi.org/10.1007/s00068-019-01181-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01181-7