Abstract
Objective
Radiotherapy (RT) has an established role in the curative treatment of indolent primary cutaneous B‑cell lymphoma (PCBCL). With the role of low-dose regimens such as 2 × 2 Gy being uncertain, we compared conventional-dose RT to a low-dose approach and investigated outcome and toxicities.
Materials and methods
We retrospectively reviewed the medical records of 26 patients with 44 cutaneous lesions treated at our institution between 2007 and 2017, comprising 22 marginal zone lymphoma (PCMZL) lesions and 22 follicle center lymphoma (PCFCL) lesions. Seven lesions (16%) were treated with low-dose RT (LDRT) (4 Gy) and 37 (84%) with conventional-dose RT (≥24 Gy, median 40 Gy). Median follow-up duration was 76 months.
Results
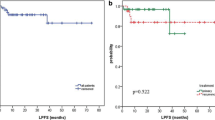
The overall response rate (ORR) was 91% (complete response rate [CRR]: 75%). The 5‑year local control rate (LCR) was 88% and the 10-year LCR was 84%. The response rates were significantly higher following conventional-dose RT (ORR: 92% vs. 86%; CRR: 84% vs. 29%; P = 0.007). In terms of radiation dose, the rate of infield relapses (14% vs. 11%, P = 0.4) and the 5‑year LCR (86% vs. 90%, P = 0.4) were comparable in the LDRT and conventional-dose RT groups. During RT courses, about two-thirds of patients experienced mild toxicities, with grade I and II acute toxicity rates of 61% and 9%, respectively, with lower incidences of grade I (14% vs. 70%) and grade II (0% vs. 8%, P = 0.004) toxicities following LDRT.
Conclusion
This long-term analysis confirms the excellent outcome of RT in the management of PCBCL. The LDRT concept with 4 Gy was associated with a comparable LCR and reduced rates of acute toxicity. However, the response rates were significantly lower for this group and LDRT may therefore not be recommended as standard treatment.
Zusammenfassung
Zielsetzung
Die Strahlentherapie (RT) hat eine etablierte Rolle in der kurativen Behandlung indolenter primär kutaner B‑Zell-Lymphome (PCBCL). Die Rolle einer Niedrigdosis-Behandlung (z. B. 2 × 2 Gy) wird kontrovers diskutiert, sodass in der folgenden Studie ein Vergleich der konventionellen RT-Dosis mit einem Niedrigdosis-Konzept erfolgte und hierbei Effektivität und Toxizitäten analysiert wurden.
Material und Methoden
In einer retrospektiven Analyse wurden 26 Patienten mit 44 kutanen Läsionen identifiziert, die zwischen 2007 und 2017 an unserer Klinik behandelt wurden. Hierunter waren 22 Läsionen von Marginalzonenlymphomen (PCMZL) und 22 Läsionen von Follikelzentrumslymphomen (PCFCL). Es wurden 7 Läsionen (16 %) mit Niedrigdosis-RT (LDRT) (4 Gy) behandelt und 37 Läsionen (84 %) mit einer RT in konventioneller Dosis (≥24 Gy, im Median 40 Gy). Das mediane Follow-up betrug 76 Monate.
Ergebnisse
Die Gesamtansprechrate (ORR) lag bei 91 % (komplette Ansprechrate [CRR]: 75 %). Die 5‑Jahres-Lokalkontrollrate (LCR) war 88 % und die 10-Jahres-LCR 84 %. Die Ansprechraten waren nach Bestrahlung in konventioneller Dosis signifikant höher (ORR: 92 % vs. 86 %; CRR: 84 % vs. 29 %; P = 0,007). Im Hinblick auf die Rate an „Infield“-Rezidiven (14 % vs. 11 %; P = 0,4) und die 5‑Jahres-LCR (86 % vs. 90 %; P = 0,4) waren die Gruppen der LDRT und der konventionellen Bestrahlung vergleichbar. Während der RT traten Grad-I-Toxizitäten bei 61 % und Grad-2-Toxizitäten bei 9 % der Patienten auf, mit signifikant weniger Akuttoxizitäten vom Grad I (14 % vs. 70 %) und vom Grad II (0 % vs. 8 %; P = 0,004) in der LDRT-Gruppe.
Schlussfolgerung
Diese Langzeitanalyse bestätigt die exzellenten Ergebnisse der RT in der Behandlung von PCBCL. Die LDRT mit 4 Gy war mit einer vergleichbaren LCR und niedrigeren Toxizitäten verbunden. Allerdings waren die Ansprechraten signifikant niedriger, sodass die LDRT nicht als Standard empfohlen werden kann.


Similar content being viewed by others

References
Dippel E, Assaf C, Becker JC et al (2017) S2k guidelines—cutaneous lymphomas update 2016—part 1: classification and diagnosis (ICD10 C82–C86): German guidelines for cutaneous lymphomas. J Dtsch Dermatol Ges 15:1266–1273. https://doi.org/10.1111/ddg.13372
Nicolay JP, Wobser M (2016) Cutaneous B‑cell lymphomas—pathogenesis, diagnostic workup, and therapy. J Dtsch Dermatol Ges 14:1207–1224. https://doi.org/10.1111/ddg.13164
Willemze R, Hodak E, Zinzani PL et al (2018) Primary cutaneous lymphomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 29(iv30):iv40. https://doi.org/10.1093/annonc/mdy133
Willemze R, Cerroni L, Kempf W et al (2019) The 2018 update of the WHO-EORTC classification for primary cutaneous lymphomas. Blood. https://doi.org/10.1182/blood-2018-11-881268
Senff NJ, Noordijk EM, Kim YH et al (2008) European Organization for Research and Treatment of Cancer and International Society for Cutaneous Lymphoma consensus recommendations for the management of cutaneous B‑cell lymphomas. Blood 112:1600–1609. https://doi.org/10.1182/blood-2008-04-152850
World Health Organization (2017) WHO classification of tumours of haematopoietic and lymphoid tissues. International Agency for Research on Cancer, Lyon (revised 4th edn)
Dippel E, Assaf C, Becker JC et al (2018) S2k guidelines—cutaneous lymphomas update 2016—part 2: treatment and follow-up (ICD10 C82–C86): German guidelines for cutaneous lymphomas. J Dtsch Dermatol Ges 16:112–122. https://doi.org/10.1111/ddg.13401
Specht L, Dabaja B, Illidge T et al (2015) Modern radiation therapy for primary cutaneous lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 92:32–39. https://doi.org/10.1016/j.ijrobp.2015.01.008
Christensen L, Cooper K, Honda K, Mansur D (2018) Relapse rates in patients with unilesional primary cutaneous B‑cell lymphoma treated with radiation therapy: a single-institution experience. Br J Dermatol 179:1172–1173. https://doi.org/10.1111/bjd.16783
De Felice F, Grapulin L, Pieroni A et al (2018) Radiation therapy in indolent primary cutaneous B cell lymphoma: a single institute experience. Ann Hematol 97:2411–2416. https://doi.org/10.1007/s00277-018-3471-x
Eich HT, Eich D, Micke O et al (2003) Long-term efficacy, curative potential, and prognostic factors of radiotherapy in primary cutaneous B‑cell lymphoma. Int J Radiat Oncol Biol Phys 55:899–906
Gauci M‑L, Quero L, Ram-Wolff C et al (2018) Outcomes of radiation therapy of indolent cutaneous B‑cell lymphomas and literature review. J Eur Acad Dermatol Venereol 32:1668–1673. https://doi.org/10.1111/jdv.14972
Goyal A, Carter JB, Pashtan I et al (2018) Very low-dose versus standard dose radiation therapy for indolent primary cutaneous B‑cell lymphomas: a retrospective study. J Am Acad Dermatol 78:408–410. https://doi.org/10.1016/j.jaad.2017.07.053
Hoefnagel JJ, Vermeer MH, Jansen PM et al (2005) Primary cutaneous marginal zone B‑cell lymphoma: clinical and therapeutic features in 50 cases. Arch Dermatol 141:1139–1145. https://doi.org/10.1001/archderm.141.9.1139
Kirova YM, Piedbois Y, Le Bourgeois J‑P (1999) Radiotherapy in the management of cutaneous B‑cell lymphoma. Our experience in 25 cases. Radiother Oncol 52:15–18. https://doi.org/10.1016/S0167-8140(99)00089-4
Pashtan I, Mauch PM, Chen Y‑H et al (2013) Radiotherapy in the management of localized primary cutaneous B‑cell lymphoma. Leuk Lymphoma 54:726–730. https://doi.org/10.3109/10428194.2012.723707
Senff NJ, Hoefnagel JJ, Neelis KJ et al (2007) Results of radiotherapy in 153 primary cutaneous B‑Cell lymphomas classified according to the WHO-EORTC classification. Arch Dermatol 143:1520–1526. https://doi.org/10.1001/archderm.143.12.1520
Smith BD, Glusac EJ, McNiff JM et al (2004) Primary cutaneous B‑cell Lymphoma treated with radiotherapy: a comparison of the European organization for research and treatment of cancer and the WHO classification systems. J Clin Oncol 22:634–639. https://doi.org/10.1200/JCO.2004.08.044
Akhtari M, Reddy JP, Pinnix CC et al (2016) Primary cutaneous B‑cell lymphoma (non-leg type) has excellent outcomes even after very low dose radiation as single-modality therapy. Leuk Lymphoma 57:34–38. https://doi.org/10.3109/10428194.2015.1040012
Hoskin PJ, Kirkwood AA, Popova B et al (2014) 4 Gy versus 24 Gy radiotherapy for patients with indolent lymphoma (FORT): a randomised phase 3 non-inferiority trial. Lancet Oncol 15:457–463. https://doi.org/10.1016/S1470-2045(14)70036-1
Lowry L, Smith P, Qian W et al (2011) Reduced dose radiotherapy for local control in non-Hodgkin lymphoma: a randomised phase III trial. Radiother Oncol 100:86–92. https://doi.org/10.1016/j.radonc.2011.05.013
Neelis KJ, Schimmel EC, Vermeer MH et al (2009) Low-dose palliative radiotherapy for cutaneous B‑ and T‑cell lymphomas. Int J Radiat Oncol Biol Phys 74:154–158. https://doi.org/10.1016/j.ijrobp.2008.06.1918
Elsayad K, Reinartz G, Oertel M et al (2019) Radiotherapy of extranodal low-grade follicular and marginal zone lymphomas: long-term follow-up of 159 patients. Strahlenther Onkol. https://doi.org/10.1007/s00066-019-01538-2
Mian M, Marcheselli L, Luminari S et al (2011) CLIPI: a new prognostic index for indolent cutaneous B cell lymphoma proposed by the International Extranodal Lymphoma Study Group (IELSG 11). Ann Hematol 90:401–408. https://doi.org/10.1007/s00277-010-1083-1
König L, Stade R, Rieber J et al (2016) Radiotherapy of indolent orbital lymphomas: two radiation concepts. Strahlenther Onkol 192:414–421. https://doi.org/10.1007/s00066-016-0962-3
König L, Hörner-Rieber J, Bernhardt D et al (2018) Response rates and recurrence patterns after low-dose radiotherapy with 4 Gy in patients with low-grade lymphomas. Strahlenther Onkol 194:454–461. https://doi.org/10.1007/s00066-018-1277-3
Sampogna F, Frontani M, Baliva G et al (2009) Quality of life and psychological distress in patients with cutaneous lymphoma. Br J Dermatol 160:815–822. https://doi.org/10.1111/j.1365-2133.2008.08992.x
Hamilton SN, Wai ES, Tan K et al (2013) Treatment and outcomes in patients with primary cutaneous B‑cell lymphoma: the BC cancer agency experience. Int J Radiat Oncol Biol Phys 87:719–725. https://doi.org/10.1016/j.ijrobp.2013.07.019
Dabaja B (2017) Renaissance of low-dose radiotherapy concepts for cutaneous lymphomas. Oncol Res Treat 40:255–260. https://doi.org/10.1159/000470845
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Oertel, K. Elsayad, C. Weishaupt, K. Steinbrink, and H.T. Eich declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Oertel, M., Elsayad, K., Weishaupt, C. et al. De-escalated radiotherapy for indolent primary cutaneous B-cell lymphoma. Strahlenther Onkol 196, 126–131 (2020). https://doi.org/10.1007/s00066-019-01541-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01541-7