Abstract
Purpose
The aim of this work was to evaluate long-term results of moderate hypofractionated stereotactic radiotherapy (hFSRT) for intracranial meningiomas.
Patients and methods
In all, 77 consecutive patients with 80 lesions were included. Median age was 65 years (range 23–82 years), male/female ratio was 21/56, and the median Karnofsky performance status was 90 (range 60–100). In 31 lesions (39 %), diagnosis was based upon clinical and radiological data; 37 lesions were histologically proven as World Health Organization (WHO) grade I and 12 grade II meningiomas. Median treatment volume was 23 cc. Prescribed doses were 45 Gy in 15 fractions of 3 Gy (15 × 3 Gy) or 42 Gy in 14 fractions of 3 Gy (14 × 3 Gy).
Results
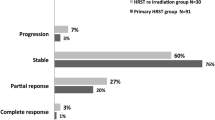
After a median follow-up of 56 months, 49 (61 %) lesions received 14 × 3 Gy and 31 (39 %) 15 × 3 Gy. Local control (LC) rate remained unchanged at 84 % at 5 and 10 years. Overall survival and disease-specific survival (DSS) were 76 and 93 % at 5 years, 72 and 89 % at 10 years, respectively. With univariate analysis, previous surgery and WHO grade II tumor were negative prognostic factors for LC and DSS. With multivariate analysis only tumor grade was an independent prognostic factor for LC. No clinically significant acute and/or late toxicities were observed.
Conclusion
Moderate hFSRT was effective and safe with an excellent tolerance profile. It can be an alternative treatment option for patients with recurrent or inoperable large meningiomas. The low number of fractions administered with hFSRT led to reduce treatment-related discomfort for patients. Grade II tumor and previous surgery were negative prognosis factors.
Zusammenfassung
Ziel
Untersucht wurden die Langzeitergebnisse von moderater hypofraktionierter stereotaktischer Strahlentherapie (hFSRT) bei intrakraniellen Meningeomen.
Patienten und Methoden
Es wurden 77 konsekutive Patienten mit 80 Läsionen ausgewählt. Das durchschnittliche Alter betrug 65 Jahre (Spanne 23–82 Jahre), das Verhältnis Männer/Frauen lag bei 21/56, der mediane Karnofsky-Index betrug 90 (Spanne 60–100). Bei 31 Läsionen (39 %) basierte die Diagnose auf klinischen und radiologischen Daten. Histologisch wurden 37 Läsionen wurden WHO-(World-Health-Organization-)Grad-I- und 12 Läsionen WHO-Grad-II-Meningeomen zugeordnet. Das mediane Behandlungsvolumen betrug 23 ml. Die verschriebene Dosis betrug 45 Gy in 15 Fraktionen von je 3 Gy (15 × 3 Gy) oder 42 Gy in 14 Fraktionen von je 3 Gy (14 × 3 Gy).
Ergebnisse
Nach einer medianen Nachbeobachtungszeit von 56 Monaten erhielten 49 (61 %) der Läsionen 14 × 3 Gy, die verbleibenden 31 (39 %) 15 × 3 Gy. Die lokale Kontrollrate (LC) blieb bei 84 % nach 5 bzw. 10 Jahren. Das Gesamtüberleben und das krankheitsspezifische Überleben (DSS) lagen jeweils bei 76 % bzw. 93 % nach 5 Jahren und bei 72 % bzw. 89 % nach 10 Jahren. Bei univariater Analyse waren frühere Operationen und WHO-Grad-II-Tumoren negative prognostische Faktoren für LC und DSS. Multivariat bleib nur der Tumorgrad ein unabhängiger prognostischer Faktor für LC. Es wurde keine klinisch relevante akute und/oder späte Toxizität beobachtet.
Schlussfolgerung
Moderate hFSRT zeigte sich als wirksam und sicher mit einem ausgezeichneten Verträglichkeitsprofil. Damit bietet sie eine alternative Behandlungsmethode für Patienten mit Rezidiven und inoperablen großen Meningeomen. Die niedrige Anzahl der verabreichten Fraktionen mit hFSRT verringerte die behandlungsbedingten Beschwerden der Patienten. WHO-Grad-II-Tumoren und vorausgegangene Operationen waren negative Prognosefaktoren.



Similar content being viewed by others
References
Bondy M, Ligon BL (1996) Epidemiology and etiology of intracranial meningiomas: a review. J Neurooncol 29:197–205
Rogers L, Barani I, Chamberlain M, Kaley TJ, McDermott M, Raizer J, Schiff D, Weber DC, Wen PY, Vogelbaum MA (2014) Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg 24:1–20
Johnson WD, Loredo LN, Slater JD (2008) Surgery and radiotherapy: complementary tools in the management of benign intracranial tumors. Neurosurg Focus 24:E2
McCutcheon IE (1996) The biology of meningiomas. J Neurooncol 29:207–216
Shrivastava RK, Sen C, Costantino PD, Della Rocca R (2005) Sphenoorbital meningiomas: surgical limitations and lessons learned in their long-term management. J Neurosurg 103:491–497
Chin LS, Szerlip NJ, Regine WF (2003) Stereotactic radiosurgery for meningiomas. Neurosurg Focus 14:E6
DiBiase SJ, Kwok Y, Yovino S, Arena C, Naqvi S, Temple R (2004) Factors predicting local tumor control after gamma knife stereotactic radiosurgery for benign intracranial meningiomas. Int J Radiat Oncol Biol Phys 60:1515–1519
Kondziolka D, Levy EI, Niranjan A, Flickinger JC, Lunsford LD (1999) Long-term outcomes after meningioma radiosurgery: physician and patient perspectives. J Neurosurg 91:44–50
Henzel M, Gross MW, Hamm K, Surber G, Kleinert G, Failing T, Strassmann G, Engenhart-Cabillic R (2006) Stereotactic radiotherapy of meningiomas: symptomatology, acute and late toxicity. Strahlenther Onkol 182:382–388
Baumert BG, Villa S, studert G, Mrimanoff RO, Davis JB, Landau K, Ducrey N, Arruga J, Lambin P, Pica A (2004) Early improvements in vision after fractionated stereotactic radiotherapy for primary optic nerve sheath meningioma. Radiother Oncol 72:169–174
Elia AE, Shih HA, Loeffler JS (2007) Stereotactic radiation treatment for benign meningiomas. Neurosurg Focus 23:E5
Shrieve DC, Hazard L, Boucher K, Jensen RL (2004) Dose fractionation in stereotactic radiotherapy for parasellar meningiomas: radiobiological considerations of efficacy and optic nerve tolerance. J Neurosurg 101:390–395
Fokas E, Henzel M, Surber G, Hamm K, Engenhart-Cibillic R (2014) Stereotactic radiation therapy for benign maningioma: long-term outcome in 318 patients. Int J Radiat Oncol Biol Phys 89:569–575
Trippa F, Maranzano E, Costantini S, Giorgi C (2009) Hypofractionated stereotactic radiotherapy for intracranial meningiomas: preliminary results of a feasible trial. J Neurosurg Sci 53:7–11
Nagele T, Petersen D, Klose U, Grodd W, Opitz H, Voigt K (1994) The “dural tail” adjacent to meningiomas studied by dynamic contrast-enhanced MRI: a comparison with histopathology. Neuroradiology 36:303–307
Liu L, Bassano DA, Prasad SC, Hahn SS, Chung CT (2003) The linear-quadratic model and fractionated stereotactic radiotherapy. Int J Radiat Oncol Biol Phys 57:827–832
Shigematsu N, Kunieda E, Kawaguchi O, Takeda A, Ihara N, Yamashita S, Kubo A, Ito H (2000) Indications on stereotactic irradiation for brain lesions. Acta Oncol 39:597–603
Debus J, Hug EB, Liebsch NJ, O’Farrel D, Finkelstein D, Efird J, Munzenrider JE (1997) Brainstem tolerance to conformal radiotherapy of skull base tumors. Int J Radiat Oncol Biol Phys 39:967–975
Trotti A, Covales AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, Rubin P (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Sem Radiat Oncol 13:176–181
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Cox D (1972) Regression models and life tables. J R Stat Soc B 34:187–220
Marks LB, Spencer DP (1991) The influence of volume on the tolerance of the brain to radiosurgery. J Neurosurg 75:177–180
Han J, Girvigian MR, Chen JTC, Miller MJ, Lodin K, Rahimian J, Arellano A, Cahan BL, Kaptein JS (2014) A comparative study of stereotactic radiosurgery, hypofractionated, and fractionated stereotactic radiotherapy in the treatment of skull base meningioma. Am J Clin Oncol 37:255–260
Hoffmann W, Mühleisen H, Hess CF, Kortmann RD, Schmidt B, Grote EH, Bamberg M (1995) Atypical and anaplastic meningiomas-does the new who-classification of brain tumors affect the indication for postoperative irradiation? Acta Neurochir 135:171–178
Milker-Zabel S, Zabel-du Bois A, Huber P, Schlegel W, Dedus J (2006) Fractionated stereotactic radiation therapy in the management of benign cavernous sinus meningiomas. Strahlenther Onkol 182:635–640
Soldà F, Wharram B, De Ieso PB, Bonner J, Ashley S, Brada M (2013) Long-term efficacy of fractionated radiotherapy for benign meningiomas. Radiother Oncol 109:330–334
Milker-Zabel S, Zabel A, Schulz-Ertner D, Schlegel W, Wannenmacher M, Debus J (2005) Fractionated stereotactic radiotherapy in patients with benign or atypical intracranial meningioma: long-term experience and prognostic factors. Int J Radiat Oncol Biol Phys 61:809–816
Kaul D, Budach V, Wurm R, Gruen A, Graaf L, Habbel P, Badakhshi H (2014) Linac-based stereotactic radiotherapy and radiosurgery in patients with meningioma. Radiat Oncol 9:78–87
Buglione M, De Bari B, Trevisan F, Ghirardelli P, Pedretti S, Triggiani L, Magrini SM (2014) Role of external beam radiotherapy in the treatment of relapsing meningioma. Med Oncol 31:866
Minniti G, Amichetti M, Enrici RM (2009) Radiotherapy and radiosurgery for benign skull base meningiomas. Radiat Oncol 4:42
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Maranzano, L. Draghini, M. Casale, F. Arcidiacono, P. Anselmo, F. Trippa, C. Giorgi state that there are no conflicts of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 (in its most recently amended version). Informed consent was obtained from all patients included in the study.
Rights and permissions
About this article
Cite this article
Maranzano, E., Draghini, L., Casale, M. et al. Long-term outcome of moderate hypofractionated stereotactic radiotherapy for meningiomas. Strahlenther Onkol 191, 953–960 (2015). https://doi.org/10.1007/s00066-015-0915-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-015-0915-2