Abstract
Purpose
To investigate the conversion of prostate cancer radiotherapy (RT) target definition from CT-based planning into an MRI-only-based planning procedure.
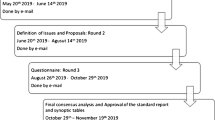
Materials and methods
Using the CT- and MRI-only-based RT planning protocols, 30 prostate cancer patients were imaged in the RT fixation position. Two physicians delineated the prostate in both CT and T2-weighted MRI images. The CT and MRI images were coregistered based on gold seeds and anatomic borders of the prostate. The uncertainty of the coregistration, as well as differences in target volumes and uncertainty of contour delineation were investigated. Conversion of margins and dose constraints from CT- to MRI-only-based treatment planning was assessed.
Results
On average, the uncertainty of image coregistration was 0.4 ± 0.5 mm (one standard deviation, SD), 0.9 ± 0.8 mm and 0.9 ± 0.9 mm in the lateral, anterior–posterior and base–apex direction, respectively. The average ratio of the prostate volume between CT and MRI was 1.20 ± 0.15 (one SD). Compared to the CT-based contours, the MRI-based contours were on average 2–7 mm smaller in the apex, 0–1 mm smaller in the rectal direction and 1–4 mm smaller elsewhere.
Conclusion
When converting from a CT-based planning procedure to an MRI-based one, the overall planning target volumes (PTV) are prominently reduced only in the apex. The prostate margins and dose constraints can be retained by this conversion.
Zusammenfassung
Ziel
Ziel unserer Studie war es, die Umstellung der Strahlentherapieplanung des Prostatakarzinoms von CT-gestützter in ausschließlich MR-gestützte Zieldefinition zu untersuchen.
Material und Methoden
Bei 30 Patienten mit Prostatakarzinom wurden eine CT und eine MRT unter Planungsbedingungen durchgeführt. Zwei Untersucher konturierten die Prostata in CT- und T2-gewichteten MR-Bildern. Mit Hilfe der Position von Goldstiften und der anatomischen Grenzen der Prostata wurden die CT- und MR-Bilder koregistriert. Es wurden die Genauigkeit der Koregistrierung sowie die Unterschiede der Zielvolumina und der Konturierung gemessen. Die Konvertierung der Prostatakonturen und die Dosisbeschränkung von CT- zu ausschließlich MR-gestützter Therapieplanung wurden bewertet.
Ergebnisse
Die Abweichung der Koregistrierung der Bilder betrug im Durchschnitt 0,4 ± 0,5 mm (Standardabweichung: 1 SD) in lateraler, 0,9 ± 0,8 mm in a.-p.- und 0,9 ± 0,9 mm in der Basis-Apex-Richtung. Das durchschnittliche Verhältnis des Prostatavolumens zwischen CT und MRT war 1,20 ± 0,15 (1 SD). Die MR-basierte Konturierung war verglichen mit der CT-basierten Konturierung im Bereich des Apex der Prostata im Durchschnitt um 2–7 mm , in rektaler Richtung um 0–1 mm und in der übrigen Prostata um 1–4 mm kleiner.
Schlussfolgerung
Unsere Ergebnisse zeigen, dass durch Umstellung von CT- in MR-gestützte Strahlentherapieplanung das Planungszielvolumen nur in der Prostataspitze deutlich reduziert wird. Die Umwandlung von CT-gestützter oder CT- und MR-gestützter in ausschließlich MR-gestützte Strahlenplanung erlaubt die Beibehaltung der Prostatakonturen und der Dosisbeschränkung.

Similar content being viewed by others
References
Chen Z, Ma CM, Paskalev K et al (2006) Investigation of MR image distortion for radiotherapy treatment planning of prostate cancer. Phys Med Biol 51:1393–1403
Kapanen M, Collan J, Beule A et al (2013) Commissioning of MRI-only based treatment planning procedure for external beam radiotherapy of prostate. Magn Reson Med 70:127–135
Korhonen J, Kapanen M, Keyriläinen J et al (2014) Influence of MRI-based bone outline definition errors on external radiotherapy dose calculation accuracy in heterogeneous pseudo-CT images of prostate cancer patients. Acta Oncol 53:1100–1106
Lee YK, Bollet M, Charles-Edwards G et al (2003) Radiotherapy treatment planning of prostate cancer using magnetic resonance imaging alone. Radiother Oncol 66:203–216
Chen L, Price RA, Nguyen T-B et al (2004) Dosimetric evaluation of MRI-based treatment planning for prostate cancer. Phys Med Biol 49:5157–5170
Chen L, Price RA, Wang L et al (2004) MRI-based treatment planning for radiotherapy: dosimetric verification for prostate IMRT. Int J Radiat Oncol Biol Phys 60:636–647
Jonsson JH, Karlsson MG, Karlsson M et al (2010) Treatment planning using MRI data: an analysis of the dose calculation accuracy for different treatment regions. Radiat Oncol 5:62–69
Kapanen M, Tenhunen M (2013) T1/T2*-weighted MRI provides clinically relevant pseudo-CT density data for the pelvic bones in MRI-only based radiotherapy treatment planning. Acta Oncol 52:612–618
Korhonen J, Kapanen M, Keyriläinen J et al (2014) A dual model HU conversion from MRI intensity value within and outside of bone segment for MRI-based radiotherapy treatment planning of prostate cancer. Med Phys 41:011704
Rasch C, Barillot I, Remeijer P et al (1999) Definition of the prostate in CT and MRI: a multi-observer study. Int J Radiat Oncol Biol Phys 43:57–66
Debois M, Oyen R, Maes F et al (1999) The contribution of magnetic resonance imaging to the three-dimensional treatment planning of localized prostate cancer. Int J Radiat Oncol Biol Phys 45:857–865
Sannazzari GL, Ragona R, Ruo Redda MG et al (2002) CT-MRI image fusion for delineation of volumes in three-dimensional conformal radiation therapy in the treatment of localized prostate cancer. Br J Radiol 75:603–607
Smith WL, Lewis C, Bauman G et al (2007) Prostate volume contouring: a 3D analysis of segmentation using 3DTRUS, CT, and MR. Int J Radiat Oncol Biol Phys 67:1238–1247
Hentschel B, Oehler W, Strauss D et al (2011) Definition of the CTV prostate in CT and MRI by using CT-MRI image fusion in IMRT planning for prostate cancer. Strahlenther Onkol 187:183–190
Parker C, Damyanovich A, Haycocks T et al (2003) Magnetic resonance imaging in the radiation treatment planning of localized prostate cancer using intra-prostatic fiducial markers for computed tomography co-registration. Radiother Oncol 66:217–224
Wachter S, Wachter-Gerstner N, Bock T et al (2002) Interobserver comparison of CT and MRI-based prostate apex definition. Clinical relevance for conformal radiotherapy treatment planning. Strahlenther Onkol 178:263–268
Roberson P, McLaughlin P, Narayana V et al (2005) Use and uncertainties of mutual information for computed tomography/magnetic resonance (CT/MR) registration post permanent implant of the prostate. Med Phys 32:473–482
Nyholm T, Nyberg M, Karlsson MG et al (2009) Systematisation of spatial uncertainties for comparison between a MR and a CT-based radiotherapy workflow for prostate treatments. Radiat Oncol 4:54–62
Zhong H, Wen N, Gordon JJ et al (2015) An adaptive MR-CT registration method for MRI-guided prostate cancer radiotherapy. Phys Med Biol 60:2837–2851
Stanescu T, Wachowicz K, Jaffray DA (2012) Characterization of tissue magnetic susceptibility-induced distortions for MRIgRT. Med Phys 39:7185–7193
Polat B, Guenther I, Wilbert J et al (2008) Intra-fractional uncertainties in image-guided intensity-modulated radiotherapy (IMRT) of prostate cancer. Strahlenther Onkol 184:668–673
Sander L, Langkilde NC, Holmberg M et al (2014) MRI target delineation may reduce long-term toxicity after prostate radiotherapy. Acta Oncol 53:809–814
Doemer A, Chetty IJ, Glide-Hurst C et al (2015) Evaluating organ delineation, dose calculation and daily localization in an open-MRI simulation workflow for prostate cancer patients. Radiat Oncol 10:309
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was financially supported by grant from the Helsinki University Central Hospital Research Funds, Helsinki, Finland. The authors alone are responsible for the content and writing of the paper.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Seppälä, T., Visapää, H., Collan, J. et al. Converting from CT- to MRI-only-based target definition in radiotherapy of localized prostate cancer. Strahlenther Onkol 191, 862–868 (2015). https://doi.org/10.1007/s00066-015-0868-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-015-0868-5