Abstract
Background
The optimal treatment for patients with a single brain metastasis is controversial. This study investigated the value of a radiation boost given in addition to neurosurgerical resection and whole-brain irradiation (WBI).
Patients and methods
In this retrospective study, outcome data of 105 patients with a single brain metastasis receiving metastatic surgery plus WBI (S + WBI) were compared to 90 patients receiving the same treatment plus a boost to the metastatic site (S + WBI + B). The outcomes that were compared included local control of the resected metastasis (LC) and overall survival (OS). In addition to the treatment regimen, eight potential prognostic factors were evaluated including age, gender, performance status, extent of metastatic resection, primary tumor type, extracerebral metastases, recursive partitioning analysis (RPA) class, and interval from first diagnosis of cancer to metastatic surgery.
Results
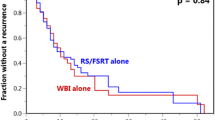
The LC rates at 1 year, 2 years, and 3 years were 38%, 20%, and 9%, respectively, after S + WBI, and 67%, 51%, and 33%, respectively, after S + WBI + B (p = 0.002). The OS rates at 1 year, 2 years, and 3 years were 52%, 25%, and 19%, respectively, after S + WBI, and 60%, 40%, and 26%, respectively, after S + WBI + B (p = 0.11). On multivariate analyses, improved LC was significantly associated with OP + WBI + B (p = 0.006) and total resection of the metastasis (p = 0.014). Improved OS was significantly associated with age ≤ 60 years (p = 0.028), Karnofsky Performance Score > 70 (p = 0.015), breast cancer (p = 0.041), RPA class 1 (p = 0.012), and almost with the absence of extracerebral metastases (p = 0.05).
Conclusion
A boost in addition to WBI significantly improved LC but not OS following resection of a single brain metastasis.
Zusammenfassung
Hintergrund
Die optimale Therapie von Patienten mit einer singulären Hirnmetastase ist nicht hinreichend geklärt. In dieser Studie wurde der Effekt eines zusätzlichen Boosts der Metastasenregion nach Operation (S) plus Ganzhirnbestrahlung (WBI) untersucht.
Patienten und Methoden
In dieser retrospektiven Analyse wurden 105 Patienten mit einer singulären Hirnmetastase, die eine Operation plus WBI (S + WBI) erhalten hatten, mit 90 Patienten, die eine Operation plus WBI plus einen Boost der Metastasenregion (S + WBI + B) erhalten hatten, für die lokale Kontrolle der resezierten Metastase (LC) und das Gesamtüberleben (OS) verglichen. Zusätzlich wurden 8 weitere mögliche Prognosefaktoren untersucht: Alter, Geschlecht, Allgemeinzustand, Resektionsstatus, Art des Primärtumors, extrazerebrale Metastasen, RPA-Klasse („recursive partitioning analysis“) sowie das Zeitintervall von der Erstdiagnose der Tumorerkrankung bis zur Metastasenresektion.
Ergebnisse
Die Raten für die LC nach einem Jahr, nach 2 und nach 3 Jahren betrugen 38%, 20% und 9% nach S + WBI sowie 67%, 51% und 33% nach S + WBI + B (p = 0,002). Die Raten für das OS nach einem Jahr, nach 2 und 3 Jahren betrugen 52%, 25% und 19% nach S + WBI sowie 60%, 40% und 26% nach S + WBI + B (p = 0,11). In der Multivarianzanalyse war eine bessere LC signifikant mit OP + WBI + B (p = 0,006) und kompletter Metastasenentfernung (p = 0,014) assoziiert. Ein besseres OS war signifikant mit einem Alter ≤ 60 Jahren (p = 0,028), einem Karnofsky-Index > 70 (p = 0,015), einem Mammakarzinom als Primärtumor (p = 0,041), einer RPA-Klasse 1 (p = 0,012) und fast signifikant mit dem Nichtvorhandensein extrazerebraler Metastasen (p = 0,05) assoziiert.
Schlussfolgerungen
Bei der Behandlung einer singulären Hirnmetastase verbessert ein zusätzlicher Boost nach der Operation und WBI die lokale Kontrolle, nicht aber das Gesamtüberleben.


Similar content being viewed by others
References
Aoyama H, Tago M, Kato N et al (2007) Neurocognitive function of patients with brain metastasis who received either whole brain radiotherapy plus stereotactic radiosurgery or radiosurgery alone. Int J Radiat Oncol Biol Phys 68:1388–1395
Bruner DW, Wasserman T (1995) The impact on quality of life by radiation late effects. Int J Radiat Oncol Biol Phys 31:1353–1355
Fokas E, Henzel M, Engenhart-Cabillic R (2010) A comparison of radiotherapy with radiotherapy plus surgery for brain metastases from urinary bladder cancer: analysis of 62 patients. Strahlenther Onkol 186:565–571
Gaspar LE, Scott C, Rotman M et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37:745–751
Joiner MC, Van der Kogel AJ (1997) The linear-quadratic approach to fractionation and calculation of isoeffect relationships. In: Steel GG (ed) Basic clinical radiobiology. Oxford University Press, New York, pp 106–112
Kaplan EL, Meier P (1958) Non parametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29:134–141
Meisner J, Meyer A, Polivka B et al (2010) Outcome of moderately dosed radiosurgery for limited brain metastases. Report of a single-center experience. Strahlenther Onkol 186:76–81
Meyers CA, Smith JA, Bezjak A et al (2004) Neurocognitive function and progression in patients with brain metastases treated with whole-brain radiation and motexafin gadolinium: results of a randomized phase III trial. J Clin Oncol 22:157–165
Patchell RA, Tibbs PA, Regine WF et al (1998) Postoperative radiotherapy in the treatment of single metastases to the brain. A randomised trial. JAMA 280:1485–1489
Patchell RA, Tibbs PA, Walsh JW et al (1990) A randomized trial of surgery in the treatment of single metastases of the brain. N Engl J Med 322:494–500
Rades D, Dziggel L, Haatanen T et al (2011) Scoring systems to estimate intracerebral control and survival rates of patients Irradiated for brain metastases. Int J Radiat Oncol Biol Phys 80:1122–1127
Rades D, Nadrowitz R, Buchmann I et al (2010) Radiolabeled cetuximab plus whole-brain irradiation (WBI) for the treatment of brain metastases from non-small cell lung cancer (NSCLC). Strahlenther Onkol 186:458–462
Rades D, Pluemer A, Veninga T et al (2007) A boost in addition to whole-brain radiotherapy improves patient outcome after resection of 1 or 2 brain metastases in recursive partitioning analysis class 1 and 2 patients. Cancer 110:1551–1559
Regine WF, Scott C, Murray K et al (2001) Neurocognitive outcome in brain metastases patients treated with accelerated-fractionation vs. accelerated-hyperfractionated radiotherapy: an analysis from Radiation Therapy Oncology Group Study 91–04. Int J Radiat Oncol Biol Phys 51:711–717
Ruge MI, Kocher M, Maarouf M et al (2011) Comparison of stereotactic brachytherapy (125 iodine seeds) with stereotactic radiosurgery (LINAC) for the treatment of singular cerebral metastases. Strahlenther Onkol 187:7–14
Schoggl A, Kitz K, Reddy M et al (2000) Defining the role of stereotactic radiosurgery versus microsurgery in the treatment of single brain metastases. Acta Neurochir (Wien) 142:621–626
Smalley SR, Schray MF, Laws ER Jr et al (1987) Adjuvant radiation therapy after surgical resection of solitary brain metastasis: association with pattern of failure and survival. Int J Radiat Oncol Biol Phys 13:1611–1616
Sperduto PW, Berkey B, Gaspar LE et al (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70:510–514
Trotti A, Byhardt R, Stetz J et al (2000) Common toxicity criteria: version 2.0. An improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys 47:13–47
Vecht CJ, Haaxma-Reiche H, Noordijk EM et al (1993) Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 33:583–590
Vogelbaum MA, Suh JH (2006) Resectable brain metastases. J Clin Oncol 24:1289–1294
Conflict of interest
No statement made.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rades, D., Kueter, J., Gliemroth, J. et al. Resection plus whole-brain irradiation versus resection plus whole-brain irradiation plus boost for the treatment of single brain metastasis. Strahlenther Onkol 188, 143–147 (2012). https://doi.org/10.1007/s00066-011-0024-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-011-0024-9