Abstract
Background and purpose
To compare MRI-guided brachytherapy (BT) and two different dose prescriptions for robotic radiosurgery (RRS) in locally advanced cervical cancer.
Methods and materials
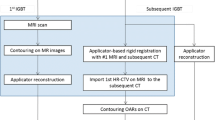
Eleven patients with FIGO stage IIB–IIIB cervical cancer underwent RRS instead of BT for various reasons. A total dose of 30 Gy was administered in five fractions. The maximum dose was chosen such that the prescribed dose was 70 % of the maximum dose (RRS70). To simulate BT more closely, additional plan calculations were carried out for a higher maximum dose with the same enclosing dose of 30 Gy being now 25 % of the maximum dose (RRS25). BT plans were calculated for the same patients (BTRRS). Finally, the resulting three sets of treatment plans were compared with 38 other patients treated with MRI-guided BT and the same dose prescription (BTref). Plan comparisons were performed based on DVH parameters with regard to target coverage (V100), conformation number (CN), and sparing of the organs at risk (OARs).
Results
The best coverage of V100 = 100 ± 0 % was obtained with RRS25, followed by RRS70 with 97.1 ± 2.7 %, BTref with 90.9 ± 8.9 %, and the intraindividual BTRRS with 80.6 ± 6.4 %. The sparing of OARs was associated with D0.1 cc, D2 cc, and D5 cc to the rectum, sigmoid, and bladder walls. OAR doses were compliant with the GEC-ESTRO guidelines and comparable among RRS70, RRS25, BTRRS, and BTref. By contrast, RRS25 could not fulfill these guidelines, exceeding considerably the tolerable dose constraints for the walls of the critical OARs.
Conclusion
Despite of the excellent coverage and higher maximum dose, the unacceptably high exposure to the OARs disqualified RRS25 as an alternative for BT in cervical cancer patients. By contrast, RRS70 offered the best protection for the OARs, comparable to BT, and even better target coverage and conformity than BT.
Zusammenfassung
Hintergrund und Ziel
Vergleich der MRT-basierten Brachytherapie mit zwei unterschiedlichen Dosisverschreibungen der robotergestützten Radiochirurgie (RRS) bei Patientinnen mit lokal fortgeschrittenem Zervixkarzinom.
Material und Methoden
Insgesamt 11 Patientinnen mit Zervixkarzinomen im Stadium FIGOIIB–IIIB erhielten aus verschiedenen Gründen statt der Brachytherapie eine RRS. Die Gesamtdosis von 30 Gy wurde in 5 Einzeldosen appliziert. Die Maximaldosis wurde so gewählt, dass die verschriebene Dosis 70 % (= 6 Gy) der Gesamtdosis (RRS70) entsprach. Als Planvergleich diente die Verschreibung von 25 % der Maximaldosis (= 6-Gy-Einzeldosis; RRS25), um eine der brachytherapieähnliche Verschreibung mit höheren Maxima im Tumor zu simulieren. Es erfolgte ein intraindividueller Planvergleich mit Hilfe der Brachytherapie (BTRRS). Die resultierenden drei Planvergleiche wurden in einem Kollektiv mit identischer Fraktionierung der MRT-basierten Brachytherapie (BTref, n = 38) auf Grundlage der Dosis-Volumen-(DVH-)Parameter bzgl. „Coverage“ (V100), „Conformation number“ (CN) und Schonung der Risikoorgane (OARs) verglichen.
Ergebnisse
Die beste Abdeckung mit einer V100 von 100 ± 0 % erzielte die RRS25, gefolgt von der RRS70 mit einer V100 von 97,1 ± 2,7 %, und der BTref mit 90,9 ± 8,9 % sowie der intraindividuell geplanten BTRRS mit nur 80,6 ± 6,4 %. Die Schonung der Risikoorgane wurde mit Hilfe der Subvolumina D0,1 cc, D2 cc, and D5 cc der Rektumwand, Sigmoid und der Harnblase evaluiert. Die OAR-Dosen wurden auf der Basis der GEC-ESTRO-Guidelines gewählt und verglichen (RRS70 vs. RRS25 vs. BTRRS vs. BTref). Im Gegensatz zu allen gewählten Techniken, konnten mit Hilfe der RRS25 die Dosisbeschränkungen der OARs nicht eingehalten werden.
Schlussfolgerungen
Trotz der exzellenten Abdeckung und der hohen Tumordosen war die RRS25 als Alternative zur Brachytherapie inakzeptabel bezüglich der Belastung der Risikoorgane. Hingegen zeigte die RRS70 die beste Schonung der umliegenden OARs verbunden mit einer besseren Abdeckung des Tumors im Vergleich zur BT.


Similar content being viewed by others
References
Dimopoulos JC, Pötter R, Lang S et al (2009) Dose–effect relationship for local control of cervical cancer by magnetic resonance image-guided brachytherapy. Radiother Oncol 93:311–315
Schmid MP, Kirisits C, Nesvacil N et al (2011) Local recurrences in cervical cancer patients in the setting of image-guided brachytherapy: a comparison of spatial dose distribution within a matched-pair analysis. Radiother Oncol 100:468–472
Haie-Meder C, Potter R, Van Limbergen E et al (2005) Recommendations from Gynaecological (GYN) GEC-ESTRO working group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol 74:235–245
Pötter R, Dimopoulos J, Kirisits C et al (2005) Recommendations for image-based intracavitary brachytherapy of cervix cancer: the GYN GEC ESTRO working group point of view: in regard to Nag et al. (Int J Radiat Oncol Biol Phys 2004;60:1160–1172) Int J Radiat Oncol Biol Phys 62:293–295
Georg P, Pötter R, Georg D et al (2012) Dose effect relationship for late side effects of the rectum and urinary bladder in magnetic resonance image-guided adaptive cervix cancer brachytherapy. Int J Radiat Oncol Biol Phys 82:653–657
Koom WS, Sohn DK, Kim JY et al (2007) computed tomography-based high-dose-rate intracavitary brachytherapy for uterine cervical cancer: preliminary demonstration of correlation between dose–volume parameters and rectum mucosal changes observed by flexible sigmoidoscopy. Int J Radiat Oncol Biol Phys 68:1446–1454
Pötter R, Dimopoulos J, Georg P et al (2007) Clinical impact of MRI assisted dose volume adaptation and dose escalation in brachytherapy of locally advanced cervix cancer. Radiother Oncol 83:148–155
Viswanathan AN, Creutzberg CL, Craighead P et al (2012) International brachytherapy practice patterns: a survey of the Gynecologic Cancer Intergroup (GCIG). Int J Radiat Oncol Biol Phys 82:250–255
Forrest J, Ackerman I, Barbera L et al (2009) Treatment outcomes for patients with advanced cervical cancer treated with GOG pro- tocol definitive chemoradiotherapy and HDR brachytherapy. Int J Radiat Oncol Biol Phys 75:S151
Barraclough LH, Swindell R, Livsey JE et al (2008) External beam boost for cancer of the cervix uteri when intracavitary therapy cannot be performed. Int J Radiat Oncol Biol Phys 71:772–778
Higginson DS, Morris DE, Jones EL et al (2011) Stereotactic body radiotherapy (SBRT): technological innovation and application in gynecologic oncology. Gynecol Oncol 120:404–412
Hsieh CH, Wei MC, Hsu YP et al (2010) Should helical tomotherapy replace brachytherapy for cervical cancer? Case report. BMC Cancer 10:637
Mollà M, Escude L, Nouet P et al (2005) Fractionated stereotactic radiotherapy boost for gynecologic tumors: an alternative to brachytherapy? Int J Radiat Oncol Biol Phys 62:118–124
Kunos C, von Gruenigen V, Waggoner S et al (2008) Cyberknife radiosurgery for squamous cell carcinoma of vulva after prior pelvic radiation therapy. Technol Cancer Res Treat 7:375–380
Kunos C, Chen W, DeBernardo R et al (2009) Stereotactic body radiosurgery for pelvic relapse of gynecologic malignancies. Technol Cancer Res Treat 8:393–400
Deodato F, Macchia G, Grimaldi L et al (2009) Stereotactic radiotherapy in recurrent gynecological cancer: a case series. Oncol Rep 22:415–419
Guckenberger M, Bachmann J, Wulf J et al (2010) Stereotactic body radiotherapy for local boost irradiation in unfavourable locally recurrent gynaecological cancer. Radiother Oncol 94:53–59
Choi CW, Cho CK, Yoo SY et al (2009) Image-guided stereotactic body radiation therapy in patients with isolated para-aortic lymph node metastases from uterine cervical and corpus cancer. Int J Radiat Oncol Biol Phys 74:147–153
Park HC, Shimizu S, Yonesaka A et al (2010) High dose three-dimensional conformal boost using the real-time tumor tracking radio-therapy system in cervical cancer patients unable to receive intracavitary brachytherapy. Yonsei Med J 51:93–99
Molla M, Escude L, Nouet P et al (2005) Fractionated stereotactic radiotherapy boost for gynecologic tumors: an alternative to brachytherapy? Int J Radiat Oncol Biol Phys 62:118–124
Jorcano S, Molla M, Escude L et al (2010) Hypofractionated extracranial stereotactic radiotherapy boost for gynecologic tumors: a promising alternative to high-dose rate brachytherapy. Technol Cancer Res Treat 9:509–514
Cengiz M, Dogan A, Ozyigit G et al (2012) Comparison of intracavitary brachytherapy and stereotactic body radiotherapy dose distribution for cervical cancer. Brachytherapy 11:125–129
Haas JA, Witten MR, Clancey O et al (2012) CyberKnife boost for patients with cervical cancer unable to undergo brachytherapy. Frontiers in Radiation Oncology 2:1–5
van’t Riet A, Mak AC, Moerland MA et al (1997) A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation: application to the prostate. Int J Radiat Oncol Biol Phys 37:731–736
Wagner TH, Bova FJ, Friedman WA et al (2003) A simple and reliable index for scoring rival stereotactic radiosurgery plans. Int J Radiat Oncol Biol Phys 57:1141–1149
Webb S, Nahum AE (1993) A model for calculating tumour control probability in radiotherapy including the effects of inhomogeneous distributions of dose and clonogenic cell density. Phys Med Biol 38:653
Sanchez-Nieto B, Nahum AE (1999) The delta-TCP concept: a clinically useful measure of tumor control probability. Int J Radiat Oncol Biol Phys 44:369–380
Tomé WA, Fowler JF (2002) On cold spots in tumor subvolumes. Med Phys 29:1590–1598
Bayer C, Vaupel P (2012) Acute versus chronic hypoxia in tumors: controversial data concerning time frames and biological consequences. Strahlenth Onkol 188:616–627
Georg P, Boni A, Ghabuous A et al (2013) Time course of late rectal- and urinary bladder side effects after MRI-guided adaptive brachytherapy for cervical cancer. Strahlenth Onkol 189:535–540
Sabater S, Sevillano M, Andres I et al (2013) Reduction of rectal doses by removal of gas in the rectum during vaginal cuff brachytherapy. Strahlenth Onkol 189:951–956
Schmid MP, Mansmann B, Federico M et al (2013) Residual tumour volumes and grey zones after external beam radiotherapy (with or without chemotherapy) in cervical cancer patients. A low-field MRI study. Strahlenth Onkol 189:238–234
Acknowledgments
We thank D. Schaal, Etienne Lessard, and Mikhail Gezginci for discussing and reviewing the manuscript.
Compliance with ethical guidelines
Conflict of interest
O. Neumann, A. Kluge, O. Lyubina, W. Wlodarczyk, U. Jahn, C. Köhler, V. Budach, M. Kufeld, and S. Marnitz state that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neumann, O., Kluge, A., Lyubina, O. et al. Robotic radiosurgery as an alternative to brachytherapy for cervical cancer patients. Strahlenther Onkol 190, 538–545 (2014). https://doi.org/10.1007/s00066-014-0614-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-014-0614-4