Purpose:
To evaluate the role of radiotherapy (RT) and prognostic factors in 62 patients with brain metastases from transitional cell carcinoma (TCC) of the urinary bladder.
Patients and Methods:
62 patients received either RT (n = 49), including whole-brain radiotherapy (WBRT) and/or stereotactic radiosurgery (SRS), or surgery (OP) combined with WBRT (n = 13). Overall survival (OS), intracerebral control (ICC) and local control (LC) were retrospectively analyzed. Six potential prognostic factors were assessed: age, gender, number of brain metastases, extracerebral metastases, recursive partitioning analysis (RPA) class, and interval from tumor diagnosis to RT.
Results:
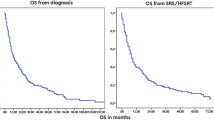
Median OS and ICC for the entire cohort were 9 and 7 months. No significant difference between RT and OP + RT was found for OS (p = 0.696) and ICC (p = 0.996). On multivariate analysis, improved OS was associated with lack of extracerebral metastases (p < 0.001) and RPA class (p < 0.001), and ICC with the latter (p < 0.001). SRS-incorporating RT resulted in 1-, 2-, and 3-year LC probability of 78%, 66%, and 51%. No association between LC and any of the potential prognostic factors was observed. The results of the subgroup RPA class analyses were similar to the entire cohort.
Conclusion:
Patient outcome for the RT-alone arm was not significantly different from OP + RT. SRS-incorporating treatment offers excellent LC rates. RPA class and the presence of extracerebral metastases demonstrated a significant prognostic role for survival. The latter should be used as stratification factors in randomized trials and can help define the cohort of patients that may benefit from more aggressive therapies.
Ziel:
Die Rolle der Strahlentherapie (RT) von Patienten (n = 62) mit Gehirnmetastasen eines Urothelkarzinoms der Harnblase sowie prognostische Faktoren wurden ermittelt.
Patienten und Methodik:
Von 62 Patienten erhielten 49 eine Ganzhirnbestrahlung (WBRT), gefolgt von einem stereotaktischen Boost oder einer alleinigen stereotaktischen Radiochirurgie (SRS). 13 Patienten erhielten eine Resektion (OP), gefolgt von einer WBRT. Gesamtüberleben sowie intrazerebrale und lokale Kontrolle wurden retrospektiv analysiert. Alter, Geschlecht, Metastasenanzahl, extrazerebrale Metastasierung, RPA-Klassifizierung (rekursive Partitionsanalyse) und Zeitintervall zwischen Diagnosestellung und RT wurden als potentielle prognostische Faktoren untersucht.
Ergebnisse:
Medianes Gesamtüberleben und intrazerebrale Kontrolle betrugen 9 und 7 Monate. Ein signifikanter Unterschied zwischen RT und RT + OP hinsichtlich des Gesamtüberlebens (p = 0,696) und der intrazerebralen Kontrolle (p=0,996) konnte nicht festgestellt werden. In der multivariaten Analyse war ein verlängertes Gesamtüberleben mit fehlender extrazerebraler Metastasierung (p < 0,001) und der RPA-Klassenzugehörigkeit (p < 0,001) assoziiert. Die intrazerebrale Kontrolle (p < 0,001) war mit der RPA-Klassenzugehörigkeit (p < 0,001) assoziiert. Die lokalen 1-, 2- und 3-Jahres-Kontrollraten betrugen 78%, 66% und 51%; ein prognostischer Faktor dafür konnte nicht ermittelt werden.
Schlussfolgerung:
Es fanden sich keine signifikanten Unterschiede zwischen alleiniger RT (WBRT ± SRS) und OP + WBRT. Sah das therapeutische Konzept eine SRS vor, waren hervorragende Kontrollraten zu erzielen. RPA-Klassifizierung und das Fehlen von extrazerebralen Metastasen haben prognostische Auswirkung auf das Gesamtüberleben. Weitergehende Studien sollten eruieren, wer von einer aggressiveren Therapie profitiert.
Similar content being viewed by others
References
Advanced Bladder Cancer (ABC) Meta-analysis Collaboration. Neoadjuvant chemotherapy in invasive bladder cancer: update of a systematic review and meta-analysis of individual patient data Advanced Bladder Cancer (ABC) Meta-analysis Collaboration. Eur Urol 2005;48:202–5, discussion 205–6
Ammirati M, Cobbs CS, Linskey ME, et al. The role of retreatment in the management of recurrent/progressive brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 2010;96:85–96
Anderson RS, el-Mahdi AM, Kuban DA, Higgins EM. Brain metastases from transitional cell carcinoma of urinary bladder. Urology 1992;39:17–20
Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 2004;363:1665–72
Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 2006;295:2483–91
Babaian RJ, Johnson DE, Llamas L, Ayala AG. Metastases from transitional cell carcinoma of urinary bladder. Urology 1980;16:142–4
Bajorin DF, Dodd PM, Mazumdar M, et al. Long-term survival in metastatic transitional-cell carcinoma and prognostic factors predicting outcome of therapy. J Clin Oncol 1999;17:3173–81
Bamias A, Tiliakos I, Karali MD, Dimopoulos MA. Systemic chemotherapy in inoperable or metastatic bladder cancer. Ann Oncol 2006;17:553–61
Bloch JL, Nieh PT, Walzak MP. Brain metastases from transitional cell carcinoma. J Urol 1987;137:97–9
Bruner DW, Wasserman T. The impact on quality of life by radiation late effects. Int J Radiat Oncol Biol Phys 1995;31:1353–5
Dhote R, Beuzeboc P, Thiounn N, et al. High incidence of brain metastases in patients treated with an M-VAC regimen for advanced bladder cancer. Eur Urol 1998;33:392–5
Fokas E, Henzel M, Hamm K, et al. Radiotherapy for brain metastases from renal cell cancer: should whole-brain radiotherapy be added to stereotactic radiosurgery? Analysis of 88 patients. Strahlenther Onkol 2010;186: 210–7
Fokas E, Wacker U, Gross MW, et al. Hypofractionated stereotactic reirradiation of recurrent glioblastomas. A beneficial treatment option after high-dose radiotherapy? Strahlenther Onkol 2009;185:235–40
Gaspar L, Scott C, Rotman M, et al. Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 1997;37:745–51
Gaspar LE, Scott C, Murray K, Curran W. Validation of the RTOG recursive partitioning analysis (RPA) classification for brain metastases. Int J Radiat Oncol Biol Phys 2000;47:1001–6
Henzel M, Gross MW, Hamm K, et al. Stereotactic radiotherapy of meningiomas: symptomatology, acute and late toxicity. Strahlenther Onkol 2006;182:382–8
Henzel M, Hamm K, Sitter H, et al. Comparison of stereotactic radiosurgery and fractionated stereotactic radiotherapy of acoustic neurinomas according to 3-D tumor volume shrinkage and quality of life. Strahlenther Onkol 2009;185:567–73
Kabalin JN, Freiha FS, Torti FM. Brain metastases from transitional cell carcinoma of the bladder. J Urol 1988;140:820–4
Kalkanis SN, Kondziolka D, Gaspar LE, et al. The role of surgical resection in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 2010;96:33–43
Kaufman D, Raghavan D, Carducci M, et al. Phase II trial of gemcitabine plus cisplatin in patients with metastatic urothelial cancer. J Clin Oncol 2000;18:1921–7
Kaufman DS, Shipley WU, Feldman AS. Bladder cancer. Lancet 2009;374: 239–49
Lehmann J, Suttmann H, Albers P, et al. Surgery for metastatic urothelial carcinoma with curative intent: the German experience (AUO AB 30/05). Eur Urol 2009;55:1293–9
Linskey ME, Andrews DW, Asher AL, et al. The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 2010;96:45–68
Mehta MP, Paleologos NA, Mikkelsen T, et al. The role of chemotherapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 2010;96:71–83
Muller-Riemenschneider F, Bockelbrink A, Ernst I, et al. Stereotactic radiosurgery for the treatment of brain metastases. Radiother Oncol 2009;91:67–74
Protzel C, Zimmermann U, Asse E, et al. Gemcitabine and radiotherapy in the treatment of brain metastases from transitional cell carcinoma of the bladder: a case report. J Neurooncol 2002;57:141–5.
Rades D, Bohlen G, Dunst J, et al. Comparison of short-course versus long-course whole-brain radiotherapy in the treatment of brain metastases. Strahlenther Onkol 2008;184:30–5
Rades D, Bohlen G, Pluemer A, et al. Stereotactic radiosurgery alone versus resection plus whole-brain radiotherapy for 1 or 2 brain metastases in recursive partitioning analysis class 1 and 2 patients. Cancer 2007;109:2515–21
Rades D, Kueter JD, Hornung D, et al. Comparison of stereotactic radiosurgery (SRS) alone and whole brain radiotherapy (WBRT) plus a stereotactic boost (WBRT+SRS) for one to three brain metastases. Strahlenther Onkol 2008;184:655–62
Rades D, Kueter JD, Pluemer A, et al. A matched-pair analysis comparing whole-brain radiotherapy plus stereotactic radiosurgery versus surgery plus whole-brain radiotherapy and a boost to the metastatic site for one or two brain metastases. Int J Radiat Oncol Biol Phys 2009;73:1077–81.
Rades D, Pluemer A, Veninga T, et al. Whole-brain radiotherapy versus stereotactic radiosurgery for patients in recursive partitioning analysis classes 1 and 2 with 1 to 3 brain metastases. Cancer 2007;110:2285–92
Reddy S, Hendrickson FR, Hoeksema J, Gelber R. The role of radiation therapy in the palliation of metastatic genitourinary tract carcinomas. A study of the Radiation Therapy Oncology Group. Cancer 1983;52:25–9
Rosenstein M, Wallner K, Scher H, Sternberg CN. Treatment of brain metastases from bladder cancer. J Urol 1993;149:480–3
Salvati M, Cervoni L, Orlando ER, Delfini R. Solitary brain metastases from carcinoma of the bladder. J Neurooncol 1993;16:217–20
Shaw E, Scott C, Souhami L, et al. Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys 2000;47:291–8
Sternberg CN, Yagoda A, Scher HI, et al. M-VAC (methotrexate, vinblastine, doxorubicin and cisplatin) for advanced transitional cell carcinoma of the urothelium. J Urol 1988;139:461–9
Trotti A, Byhardt R, Stetz J, et al. Common Toxicity Criteria: version 2.0. an improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys 2000;47:13–47
von der Maase H, Hansen SW, Roberts JT, et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol 2000;18:3068–77
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00066-011-7159-6
Rights and permissions
About this article
Cite this article
Fokas, E., Henzel, M. & Engenhart-Cabillic, R. A Comparison of Radiotherapy with Radiotherapy plus Surgery for Brain Metastases from Urinary Bladder Cancer. Strahlenther Onkol 186, 565–571 (2010). https://doi.org/10.1007/s00066-010-2159-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-010-2159-5