Abstract
Purpose:
To test for a possible correlation between high-grade acute organ toxicity during primary radio(chemo)therapy and treatment outcome in patients with locally advanced head and neck squamous cell carcinoma (HNSCC).
Patients and Methods:
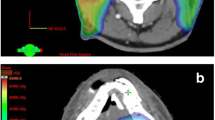
From 05/1994 to 01/2009, 216 HNSCC patients were treated with radio(chemo)therapy in primary approach. They received normofractionated (2 Gy/fraction) irradiation including associated nodal drainage sites to a cumulative dose of 70 Gy. 151 patients received additional concomitant chemotherapy (111 patients 5-fluorouracil/mitomycin C, 40 patients cisplatin-based). Toxicity during treatment was monitored weekly according to the Common Toxicity Criteria (CTC), and any toxicity grade CTC ≥ 3 of mucositis, dysphagia or skin reaction was assessed as high-grade acute organ toxicity for later analysis.
Results:
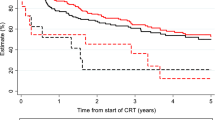
A statistically significant coherency between high-grade acute organ toxicity and overall survival as well as locoregional control was found: patients with CTC ≥ 3 acute organ toxicity had a 5-year overall survival rate of 44% compared to 8% in patients without (p < 0.01). Thereby, multivariate analyses revealed that the correlation was independent of other possible prognostic factors or factors that may influence treatment toxicity, especially concomitant chemotherapy and radiotherapy technique or treatment-planning procedure.
Conclusion:
These data indicate that normal tissue and tumor tissue may behave similarly with respect to treatment response, as high-grade acute organ toxicity during radio(chemo)therapy showed to be an independent prognostic marker in the own patient population. However, the authors are aware of the fact that a multivariate analysis in a retrospective study generally has statistical limitations. Therefore, their hypothesis should be further analyzed on biomolecular and clinical levels and other tumor entities in prospective trials.
Zusammenfassung
Hintergrund und Ziel:
Nach primärer Radio(chemo)therapie lokal fortgeschrittener Kopf-Hals-Tumoren kommt es bei einigen Patienten zu einer kompletten Remission, bei anderen lediglich zu einer partiellen Remission mit frühem Rezidiv. Unterschiedlich ist auch die Strahlenempfindlichkeit des Normalgewebes: Einige Patienten zeigen starke, andere hingegen weniger intensive Akutreaktionen. Im Rahmen dieser Arbeit wurde geprüft, ob Patienten, die höhergradige Akutreaktionen entwickeln, im Vergleich zu Patienten, bei denen diese nicht auftreten, eine bessere Prognose haben.
Patienten und Methodik:
Von 1994 bis 2009 wurden 216 Patienten mit lokal fortgeschrittenen Plattenepithelkarzinomen im Kopf-Hals-Bereich in der eigenen Klinik primär radiotherapiert (70 Gy). 151 Patienten erhielten begleitend eine Chemotherapie (111 Patienten 5-Fluorouracil/Mitomycin C, 40 Patienten Cisplatin-basiert). Jede Akuttoxizität ≥ Grad 3 in Form von Hautreaktion, Mukositis oder Dysphagie wurde als höhergradige akute Organtoxizität gewertet. Akuttoxizität ≥ Grad 3 wurde vor Beginn der Analyse als „cutoff value“ gewählt, da es ab dieser Toxizität zu einer signifikanten Einschränkung der Lebensqualität der Patienten kommt.
Ergebnisse:
Das Gesamtüberleben sowie die lokoregionäre Kontrolle nach 5 Jahren betrugen 18% bzw. 63%. Es fand sich dabei eine statistisch signifikante Korrelation zwischen höhergradiger akuter Organtoxizität und der Prognose: In der Gruppe der Patienten mit höhergradiger akuter Organtoxizität betrugen das Gesamtüberleben und die lokale Kontrolle nach 5 Jahren 44% und 74% im Vergleich zu 8% und 56% bei den Patienten ohne akute höhergradige Nebenwirkungen (p < 0,01, p = 0,04). Diese Korrelation war in multivariater Analyse statistisch unabhängig von anderen Faktoren, die möglicherweise die Toxizität beeinflussen, wie begleitende Chemotherapie oder Strahlentherapieplanung (konventionell/dreidimensional).
Schlussfolgerung:
Höhergradige akute Organtoxizität ist im untersuchten Kollektiv ein unabhängiger positiver prognostischer Faktor. Der Zusammenhang zwischen höhergradiger akuter Organtoxizität unter Radio(chemo)therapie und der Prognose sollte in prospektiven Studien weiter evaluiert werden.
Similar content being viewed by others
References
Adelstein DJ, Li Y, Adams GL, et al. An Intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol 2003;21:92–98.
Balermpas P, Hambek M, Seitz O, et al. Combined cetuximab and reirradiation for locoregional recurrent and inoperable squamous cell carcinoma of the head and neck. Strahlenther Onkol 2009;185:775–781.
Bonner JA, Harari PM, Giralt J, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol 2010;11:21–28.
Borgmann K, Hoeller U, Nowack S, et al. Individual radiosensitivity measured with lymphocytes may predict the risk of acute reaction after radiotherapy. Int J Radiat Oncol Biol Phys 2008;71:256–264.
Browman GP, Hodson DI, Mackenzie RJ, et al. Choosing a concomitant chemotherapy and radiotherapy regimen for squamous cell head and neck cancer: a systematic review of the published literature with subgroup analysis. Head Neck 2001;23:579–589.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341–1346.
Cuzick J, Sestak I, Cella D, Fallowfield L. Treatment-emergent endocrine symptoms and the risk of breast cancer recurrence: a retrospective analysis of the ATAC trial. Lancet Oncol 2008;9:1143–1148.
Dahl O, Horn A, Mella O. Do acute side-effects during radiotherapy predict tumour response in rectal carcinoma? Acta Oncol 1994;33:409–413.
de Castro G Jr, Snitcovsky IM, Gebrim EM, et al. High-dose cisplatin concurrent to conventionally delivered radiotherapy is associated with unacceptable toxicity in unresectable, non-metastatic stage IV head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol 2007;264:1475–1482.
Franzmann EJ, Lundy DS, Abitbol AA, Goodwin WJ. Complete hypopharyngeal obstruction by mucosal adhesions: a complication of intensive chemoradiation for advanced head and neck cancer. Head Neck 2006;28:663–670.
Jeremic B, Milicic B, Dagovic A, et al. Radiation therapy with or without concurrent low-dose daily chemotherapy in locally advanced, nonmetastatic squamous cell carcinoma of the head and neck. J Clin Oncol 2004;22:3540–3548.
Kuhnt T, Richter C, Enke H, Dunst J. Acute radiation reaction and local control in breast cancer patients treated with postmastectomy radiotherapy. Strahlenther Onkol 1998;174:257–261.
Patel UA, Thakkar KH, Holloway N. Patient compliance to radiation for advanced head and neck cancer at a tertiary care county hospital. Laryngoscope 2008;118:428–432.
Pignon JP, Bourhis J, Domenge C, Designe L. Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. MACH-NC Collaborative Group. Meta-Analysis of Chemotherapy on Head and Neck Cancer. Lancet 2000;355:949–955.
Rades D, Fehlauer F, Sheikh-Sarraf M, et al. Toxicity of two cisplatin-based radiochemotherapy regimens for the treatment of patients with stage III/IV head and neck cancer. Head Neck 2008;30:235–241.
Steinmann D, Cerny B, Karstens JH, Bremer M. Chemoradiotherapy with weekly cisplatin 40 mg/m2 in 103 head-and-neck cancer patients: a cumulative dose-effect analysis. Strahlenther Onkol 2009;185:682–688.
Strasser H, Grabenbauer GG, Sprung CN, et al. DNA double-strand break induction and repair in irradiated lymphoblastoid, fibroblast cell lines and white blood cells from ATM, NBS and radiosensitive patients. Strahlenther Onkol 2007;183:447–453.
Tang Y, Zhang Y, Guo L, et al. Relationship between individual radiosensitivity and radiation encephalopathy of nasopharyngeal carcinoma after radiotherapy. Strahlenther Onkol 2008;184:510–514.
Tribius S, Kronemann S, Kilic Y, et al. Radiochemotherapy including cisplatin alone versus cisplatin + 5-fluorouracil for locally advanced unresectable stage IV squamous cell carcinoma of the head and neck. Strahlenther Onkol 2009;185:675–681.
Trotti A, Byhardt R, Stetz J, et al. Common Toxicity Criteria: version 2.0. An improved reference for grading the acute effects of cancer treatment: impact on radiotherapy. Int J Radiat Oncol Biol Phys 2000;47:13–47.
Trotti A, Colevas AD, Setser A, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 2003;13:176–181.
Wolff HA, Gaedcke J, Jung K, et al. High-grade acute organ toxicity during preoperative radiochemotherapy as positive predictor for complete histopathologic tumor regression in multimodal treatment of locally advanced rectal cancer. Strahlenther Onkol 2010;186:30–35.
Wolff HA, Raus I, Jung K, et al. High-grade acute organ toxicity as positive prognostic factor in primary radiochemotherapy for anal carcinoma. Int J Radiat Oncol Biol Phys 2010:in press.
Author information
Authors and Affiliations
Corresponding author
Additional information
Both authors share senior authorship.
Rights and permissions
About this article
Cite this article
Wolff, H.A., Bosch, J., Jung, K. et al. High-Grade Acute Organ Toxicity as Positive Prognostic Factor in Primary Radio(chemo)therapy for Locally Advanced, Inoperable Head and Neck Cancer. Strahlenther Onkol 186, 262–268 (2010). https://doi.org/10.1007/s00066-010-2136-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-010-2136-z